Consultation with a dermatologist-venereologist – 1,750 rubles.
- Symptoms
- Diagnostics
- Treatment
- Prevention
Pityriasis versicolor is a chronic fungal skin disease. The fungus is present on the surface of the skin of most people and, when exposed to certain circumstances, can quickly multiply and cause a pathological process.
Provoking circumstances include:
- immunodeficiency states;
- pathologies of internal organs;
- excessive sweating;
- living in conditions of high air humidity;
- disorders of the hormonal system.
The most typical lesion for this pathology is the upper part of the body: face, neck, chest and back. It mainly affects males.
Symptoms
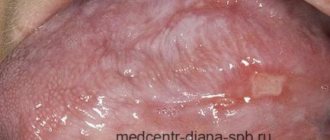
The main symptom of pityriasis versicolor is the appearance on the surface of the skin of asymmetrically located round spots with clear boundaries . They can vary in size and tend to grow larger as the disease progresses. At later stages of pathology, the lesions are characterized by fusion.
The color of such spots is very different and can vary from whitish to pink-red. Layers of small scales are visible on the surface. The skin in these places thickens and changes its structure. The lesions are not characterized by itching or other unpleasant sensations. They do not tan when exposed to ultraviolet radiation and can disappear on their own over time.
Pityriasis versicolor during pregnancy
During pregnancy, women may experience various diseases, including skin inflammation. The causes of lichen, like many ailments, in pregnant women are often a decrease in immunity or hormonal changes.
As a rule, pityriasis versicolor is not treated during pregnancy, or a gentle course with carefully selected components is prescribed so as not to harm the fetus, but to improve the quality of life of the expectant mother. Treatment is always strictly individual.
Pityriasis versicolor in children
This is a common disease in children. It usually affects the scalp, but can appear on the face and body. For young children and adolescents, as well as for pregnant women, treatment can only be prescribed externally (in particularly difficult cases, the use of medications and drugs is possible). Parents of infected children need to monitor the child’s hygiene and not allow the baby to scratch the spots in order to prevent the spread of the disease and not create a favorable background for the occurrence of other diseases.
How dangerous is solar lichen? Is pityriasis versicolor contagious or not?
If the disease does not have complications and does not occur in parallel with other diseases, then it does not pose a danger to human health, except for the psychological discomfort mentioned above, especially if spots appear on the face.
The disease can be called conditionally contagious, since the fungus (causative agent) of skin inflammation is present on the skin of any person (it is part of the microflora) or can be transmitted from person to person, but the disease itself will occur only in the event of an external “irritant”.
Infection is possible:
- during personal contacts;
- through personal and hygiene items;
- in public changing rooms or fitting rooms.
How and how to treat pityriasis versicolor in humans (colored, multi-colored, etc.)?
If you notice signs of this disease, it is important to remember three simple rules:
- do not self-medicate, because the wrong medicine can only worsen the condition;
- do not wait until everything goes away on its own (the disease has a wave-like nature, that is, it can be repeated at different intervals and does not always return in a mild form);
- Do not use dubious, suggested by someone, or self-selected remedies for pityriasis versicolor.
Seeing a doctor is a sure way to not only get cured, but also strengthen your immune system, as well as get rid of annoying aesthetic skin defects that bring psychological discomfort.
Diagnostics
Diagnosis of this pathology is carried out by a dermatovenerologist and is based on objective examination data and additional research methods. Most often, the Balser iodine test is used to clarify the diagnosis. The essence is to stain the spots with a 2% iodine solution, under the influence of which the foci of pityriasis versicolor become colored. The method with an ultraviolet Wood lamp is also used.
Additional examination for the presence of fungi in the layers of the skin is possible.
Treatment of erythrasma
To diagnose a patient with erythrasma, a dermatologist first uses a visual examination. This is especially true for rashes in the groin area, which have characteristic distinctive features in the form of pronounced protrusions and bubbles along the edges. Also, the affected areas of the skin are illuminated with a Wood's lamp and a microscopic examination of the scraping is performed to exclude other diagnoses: pityriasis versicolor or pityriasis rosea, candidiasis, dermatitis or eczema.
Treatment of erythrasma is primarily based on the use of antibacterial ointments that are used to treat the affected areas of the skin.
Under their influence, corynebacteria die, and the spots gradually lighten, decrease in diameter and disappear. On average, such therapy takes at least 7-10 days. Used in parallel:
- Antiseptics. Treatment with them is carried out before applying antibacterial ointment, as well as after it, to maintain dryness of the affected areas and prevent re-infection.
- Antifungal drugs. They are prescribed together with antibacterial drugs, since corynebacteria are similar in structure to fungal micelles.
- Exfoliating ointments. They help cleanse the skin of a layer of dead cells, activating its regeneration.
- Ultraviolet irradiation. Promotes skin disinfection and restoration. Patients benefit from both natural sunbathing and physiotherapeutic UV irradiation.
If the disease has not reached an advanced stage, the use of external medications is sufficient to solve the problem. But in some cases, with multiple skin lesions, to obtain the desired result, patients are prescribed systemic antibacterial therapy.
Prices for services
Initial appointment with a dermatologist (assessment of patient complaints, history taking, examination, preliminary diagnosis, consultation)
Primary appointment – visiting a doctor of a specific specialty for the first time. Make an appointment
1500 ₽
Repeated appointment with a dermatologist
Make an appointment
800 ₽
Appointment with a dermatologist during removal of tumors (evaluation of complaints, medical history, dermatoscopy if indicated)
Make an appointment
500 ₽
Recommendations
During treatment, hygiene rules must be observed. Wash clothes and bedding in high temperature water. Iron clothes on both sides. Clean the premises thoroughly and every day. Change the washcloth frequently and disinfect it.
- Stye: causes, symptoms and treatment
Ringworm on the face - types, causes, symptoms, treatment and prevention. 115 photos and videos of disease manifestations
Ringworm on the leg - 125 photos of what lichen looks like, common lesions and video tips on choosing a treatment method
You cannot be in the sun; the spots become light and differ from healthy skin. During treatment, the diet should be complete with a sufficient amount of vitamins, vegetables and fresh herbs, and include cereals and dairy products.
A healthy lifestyle, rest and good sleep during the treatment process will help you heal quickly. When treating hair, it is better to use detergents with ketoconazole.
Prevention
To prevent relapses, you need to treat chronic diseases, maintain immunity at the proper level, harden yourself, and eat well. Wear clothes made from natural fabrics that do not restrict movement.
Do not wear other people's clothes, do not use other people's objects. On particularly hot days, wipe the skin with water with the addition of alcohol or lemon. Maintain cleanliness and order.
Take antifungal medications once monthly. Although the lesion is not accompanied by painful sensations, it spoils the appearance and causes inconvenience.
Ringworm on the arm - 115 photos of what lichen looks like and video recommendations from dermatologists for treating the diseaseRingworm - symptoms, development, types, tips on how to quickly and effectively cure at home (105 photos and videos)
Lichen planus - first symptoms, causes, information about the disease and effective treatment (100 photos)
What kind of disease is this?
Pityriasis versicolor, also called pityriasis versicolor or pityriasis versicolor, is an infectious fungal disease. Its causative agent is fungi of the genus Malassezia from the group of dermatomycosis. It is believed that the population of southern countries is more susceptible to pityriasis versicolor, due to the hot climate. But in our country, the disease is quite common; according to various sources, from 5 to 15% of the population suffers from it. Most often, pityriasis versicolor affects people with a special predisposition to it. Exacerbations of the disease occur during the sunny season. Because of this, pityriasis versicolor is popularly called sun fungus. However, if you are “lucky enough” to catch a “sun” sore, then the consequences will not be so bright. Treatment of pityriasis versicolor can drag on for... years. The fact is that under certain circumstances the fungus tends to recur repeatedly and can drive its “host” to despair. Fortunately, the disease does not lead to disability and is not life-threatening.
Are there predisposing factors?
The fungus, which is the causative agent of pityriasis versicolor, can live on the skin for quite a long time without appearing outwardly. In order for its signs to be revealed, a push is needed. Such an impetus for the active development of fungus can be endocrine pathologies, increased sweating, weakened immunity, stressful situations for the skin that disrupt the protective function of the skin - solarium, excessive exposure to the sun, frequent use of antibacterial soaps and shower gels.
IMPORTANT!
The thought of self-medicating pityriasis versicolor is tempting. It seems so simple - I bought antifungal ointment, did it as indicated in the instructions for use, and it’s done. Alas! Without an individual, qualified course of therapy, the fungus will simply adapt to the drugs used, and further treatment will be complicated. Unsystematic or symptomatic self-treatment is highly undesirable.