Mushrooms are constant companions of humans. Thus, a fungus of the genus Candida lives in virtually every person. As long as everything is in order with the immune system, such a neighborhood is not dangerous. But as soon as any malfunction occurs in the body, the mushrooms begin to actively multiply, ceasing to be “peaceful neighbors.”
Reproducing by spores, the fungus is easily transmitted through the air or through household contact. At the same time, the spores are very “tenacious” - they persist for a long time on clothes, bedding, hygiene items and are ready to become active at any time.
What to do to prevent the colonization of pathological microorganisms and how to cure hair fungus so that the disease does not return again and again - we will understand the symptoms, diagnosis and treatment features.
What is a fungus
A group of microorganisms that parasitize the skin and its stratum corneum (hair and nails) are called dermatomycetes, or dermatophytes. They readily master keratin-containing substances.
Mushrooms are essentially heterotrophs, that is, they use ready-made organic substances for their nutrition. Their digestion is external. This means that all waste products of fungi end up on the skin and mucous membranes of humans. Forming entire colonies, they penetrate the epidermis and provoke inflammation. In this case, healthy cells die, including the hair follicle, which often cannot be restored after successful treatment.
Taking a history of a patient with hair loss
The complaint of “hair loss” may indicate one of two things: an increased amount of hair being lost daily (effluvium) or visible baldness (alopecia). Up to 100 hairs are typically lost daily (3). It is important to ask patients about the medications they are taking. While “hair loss” is listed as a possible side effect in almost all drug labels, only some drugs actually have this as an issue (e1). For example, hair loss after 2-4 months is not uncommon after multiple injections of heparin (e2). Women should be asked about gynecologic factors such as initiating or stopping hormonal contraceptives. Transient postpartum hair loss is normal: labor stress and hormonal changes after childbirth cause many hair follicles to transition from the anagen to telogen phase, and thus hair loss may be noticeable after 2–4 months (2). Highly toxic factors such as chemotherapy drugs can cause severe damage to the follicles, causing hair to break off within the follicle within one to three weeks. As a reassurance, patients can be told that this process synchronizes the growth phases of the follicles so that when the hair grows back, it is often thicker than before. Structural changes may occur in which initially straight hair will re-grow as curly hair, or vice versa (4).
Terminology
Increased daily hair loss is called “effluvium”; visible baldness is called “alopecia.”
How does scalp fungus manifest itself: the most common symptoms
The cause of itching, flaking (dandruff), and hair loss is very often a fungus (mycosis). The most common areas of the scalp are:
- Microsporum: cause microsporia;
- Trichophyton: are the causative agents of trichophytosis (ringworm);
- Malassezia furfur: leads to seborrhea.
Each infection will manifest itself differently, but some of the most common alarming symptoms can be identified - the simultaneous manifestation of two or more should alert every person:
- sudden deterioration in the general condition of the hair: it became dry, dull, and began to fall out profusely;
- dandruff has appeared (even though this has not been observed before), and/or its amount is increasing;
- separately localized flaky areas appeared;
- bald spots and bald spots form, which quickly grow;
- wounds, crusts, and bumps of unknown origin were found on the scalp;
- the hair becomes brittle at the base of the follicle, resulting in black spots appearing on the skin.
Mycoses do not reveal themselves at an early stage, so you should be very careful and if any symptom appears, immediately contact a specialist. Trichologists or dermatologists deal with problems of the scalp.
Laboratory tests for diffuse effluvium
In patients with effluvium of unknown cause, laboratory testing should be performed to exclude, in particular, the following: Iron deficiency (ferritin) (7) Thyroid dysfunction (TSH, T3, T4) Stage II syphilis (TPPA test). Syphilis is very rare, but omitting an appropriate history or TPPA test in a patient with hair loss can have serious consequences for both the patient and the clinician if neurosyphilis develops further.
Main symptoms of seborrhea
This fungus can be localized not only on the scalp, but also in the area of the eyebrows, mustache, and beard. Develops against the background of disruption of the sebaceous glands. If fat is produced excessively, we are talking about oily seborrhea. If, on the contrary, there is not enough fat, then dry seborrhea. An inflamed sebaceous gland can become infected, for example, with staphylococci, which live on the skin of 90% of people, resulting in fester in the deeper layers of the skin.
A characteristic symptom is crusts (the surface layer of the skin cracks and peels off), as well as profuse dandruff. Reddish-pink spots may appear. Patients note a feeling of tight skin and itching when cold water hits the scalp.
Seborrhea most often affects infants and adolescents.
Causes of problems
The reasons that can lead to hair problems can be divided into external and internal:
- External – hair dyeing and bleaching, prolonged wearing of tight and uncomfortable hats, tight hairstyles, injuries, improper care, aggressive environmental factors
- Internal - these are various skin diseases, intoxications of the body, infectious diseases, the postoperative period, allergic reactions, hormonal disorders, disorders of the nervous system, deficiency conditions, disruption of the gastrointestinal tract, etc.
Signs of trichophytosis
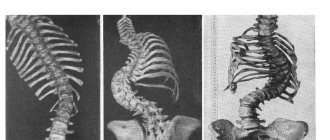
Perhaps the most severe type of mycosis of the scalp is in the hair growth area, as a result of which the patient loses hair. Differentiate between superficial and deep forms.
With superficial trichophytosis, you can first detect flaky lesions and brittle hair at the base of the follicles, as a result of which the scalp is covered with black dots. On the remainder of the hair after breaking, you can notice a gray coating. The affected areas may become red, itchy, and swollen.
The deep form manifests itself as general malaise, hyperthermia; an infected person may notice swelling and tenderness of the lymph nodes, and a rash. Pink-red spots can be found on the scalp, rising above the surface of the epidermis. They have clear contours and a round shape. The most abundant peeling is observed along the contour of the spot. Less commonly, vesicles (bubbles with liquid) can form along the contour. Such lesions spread quite quickly, which is highly likely to lead to an abscess.
General principles of treatment
In complex cases of seborrheic dermatitis, doctors prescribe medications to improve digestion and improve metabolism. Therapy often also includes vitamins, minerals, and hormonal pills.
Depending on your medical history, your doctor may prescribe hair growth activators. For oily seborrhea, drying shampoos containing tar, sulfur or salicylic acid are used.
A specialist may prescribe the use of balms with moisturizing and nutritional components - amino acids, keratin, protein.
There are two main groups of care products that can stop hair loss due to seborrhea:
- stopping the formation of dandruff;
- stimulating hair growth.
The first includes antifungal shampoos, lotions, and scrubs. It is important to use them in accordance with the instructions. The second group includes herbal tinctures, masks, and oils for rubbing into the scalp. Their task is to strengthen hair and stimulate growth.
Features of diagnosing hair fungus
A specialist can determine the presence and type of fungus relatively easily and reliably with the help of laboratory tests using microscopic and cultural methods. The first involves taking hair and skin flakes from the patient to examine for the presence of mycelial spores, gas bubbles, and fragments of large mushrooms. The cultural method is used if the presence of a fungus is nevertheless detected and allows one to determine the specific type of mycelium that has colonized the patient’s scalp. To do this, the detected fungus is grown in a nutrient medium, after which the grown colony is examined, in particular, the growth pattern is assessed (the process takes several days).
One of the modern tools used to determine mycosis is a Wood's lamp. The device emits a wave of a certain length and allows you to illuminate the colonies, giving an idea of the size and location, but not providing an answer regarding the type of microorganism, and therefore the treatment tactics.
Hair care during the treatment of seborrheic loss
Homemade masks and decoctions, selected together with a doctor, are a good help in the treatment of seborrheic hair loss. For example, you can use these tips:
- infusions and decoctions of oak bark and chamomile are suitable for disinfecting the skin;
- softening and nutrition - burdock root;
- drying - lemon water, soda water, a decoction of string;
- softening - a decoction of celandine or onion peels.
Warming masks have a beneficial effect. They stimulate blood circulation and accelerate hair growth. For such masks, take red pepper, onion, and mustard.
It is not recommended to wash your hair every day, as this can dry out your skin. If your hair quickly becomes oily at the roots, then you need to wash it 2-3 times a week, and dry hair once is enough.
How to properly treat hair fungus
As already noted, a person discovers the fungus when it has already “settled” in the hair. Like any disease, mycosis at a later stage is much more difficult to treat and relying on traditional methods in this matter means risking precious time.
Treatment tactics are determined by a specialist, based on data such as the depth and area of the lesions, the type of fungus, the general condition of the body, and the patient’s medical history. Treatment is usually complex and includes systemic medications and external agents (for example, taking tablets and using ointments). Immunotherapy or vitamin therapy may also be prescribed, since the fungus develops “with the permission” of the immune system.
Mycoses can be successfully treated - today there are effective antifungal drugs. However, a fungal infection is much more difficult to treat than a bacterial one - fungal cells are very similar in structure to human cells. If in the case of antibacterial therapy the results can be judged already on the second day, then in the case of mycosis - only on the seventh. After the clinical manifestations subside, it is important to take antifungal drugs for another 2 weeks. Thus, treatment requires time and patience - it may take up to 3 weeks. But in no case should you stop as soon as the results appear - this will definitely lead to a relapse, and new colonies may turn out to be more resistant to the drug used.
Dermatomycosis is not always an independent disease. They are often triggered by other diseases. A competent trichologist will not only be able to prescribe an effective course of treatment that will get rid of hair fungus as soon as possible, but will also be able to suspect the root cause of mycosis, thereby ensuring that the disease is detected at an earlier stage.
The conclusion is simple: to get rid of hair fungus, it is best to go to an appointment with a trichologist, who will accurately determine the type of mycosis and prescribe treatment. You should not self-medicate, leaving colonies of pathogenic microorganisms even the slightest chance of survival. In addition, you should take into account the fact that antifungal drugs have a serious effect on the liver, so treatment with such medications can only be prescribed and under the supervision of a specialist who will help you choose the most gentle and effective treatment tactics.
Methods of therapy
With seborrheic dermatitis, hair can fall out both on the entire surface of the head and in certain areas (on the back of the head, temples, frontal part). It is better to prevent the problem from developing; it is very important to intervene at an early stage. The treatment is simple. However, the process is very lengthy and requires patience, an integrated approach and consistency. Work is being carried out in a number of areas:
- organization of proper nutrition;
- use of special hair care products;
- physiotherapy;
- drug treatment.
Alopecia areata
An autoimmune disease characterized by non-scarring hair loss. It is a widespread pathology - up to 3.8% of all dermatologist patients suffer from focal alopecia. About 20% of patients are children, and in 60% the disease manifests itself before the age of 20 years.
Pathogenesis of alopecia areata
The exact pathogenesis of alopecia areata is unknown. The most popular hypothesis is that it is an autoimmune condition associated with a T-cell immune response in genetically predisposed individuals.
Clinic for alopecia areata
Alopecia areata is usually asymptomatic, but some patients experience burning or itching in the affected area. About 80% of patients have 1 area of baldness, 12.5% have 2 areas, 7.7% have 3 or more areas. Alopecia areata most often affects the scalp - 70–95% of cases, less often the beard - 28%, eyebrows - 3.8% and limbs - 1.3%.
Localized form (alopecia areata) - less than 50% of the hair falls out, the affected areas are limited, in most patients the hair grows back spontaneously within a few months ( Fig. 5 ).
Common form (total/universal alopecia) - more than 50% of hair falls out; this option is less common (on average in 7% of patients). In 30% of patients with total alopecia, complete hair loss occurs within 6 months after the onset of the disease.
Rice . 5. Alopecia areata (Danish national service on dermato-venereology)
https://www.danderm-pdv.is.kkh.dk/atlas/4-18-4-1.html
Trichoscopy for alopecia areata
- Short vellus hair
- Yellow dots
- Black dots ( Fig. 6 )
- Broken hair
- crimped hair
- Exclamation mark hair
Rice. 6. Trichoscopic signs of alopecia areata: black spots ( blue arrow ) and crimped hair ( red arrow ) (Jha AK, et al. Dermoscopy of alopecia areata - a retrospective analysis. Dermatol Pract Concept 2017; 7(2): 53–57)