Author Alexandra Balan-Senchuk
09/30/2019 12:06 (Updated: 05/25/2021 09:41)
Health
The lymphatic system plays an important role in the body by circulating lymph throughout the body to collect foreign bodies such as bacteria, viruses and waste products. The waste can be filtered out by lymphocytes, which are designed to fight infections in the body. But sometimes there are failures in this process.
General information
Elephantiasis is usually called swelling and chronic stagnation of lymph, manifested in the form of deformation and persistent diffuse increase in the size of any part of the human body, most often the limbs and scrotum. Elephantiasis is usually accompanied by painful growth - hyperplasia of the skin and subcutaneous fat.
These changes are fibrotic and irreversible, affecting the skin, subcutaneous tissue and fascia. The pathology most often affects the lower extremities, which become similar to the legs of an elephant, hence the origin of the name of the disease.
The causes of elephantiasis can be different, from parasitic agents to congenital defects of the lymphatic system. These include blockage of the lymphatic capillary system and impaired lymph circulation.
Etiology
Before listing the etiological factors, it should be noted that elephantiasis is divided into primary and secondary.
Primary elephantiasis has the following causes:
- excessive production of interstitial fluid;
- underdevelopment of lymphatic vessels or dysplasia;
- Shereshevsky-Turner syndrome;
- Milroy-Mage disease;
- other gene pathologies associated with sex chromosomes.
Secondary elephantiasis can be caused by etiological reasons such as:
- infectious infection (pathogen - hemolytic streptococcus);
- violation or complete obstruction of the lymph nodes;
- erysipelas;
- phlegmon;
- filaria infection;
- complications after syphilis;
- negative effects of radiation;
- eczema in chronic form;
- pathological processes in the veins, which leads to deterioration in the nutrition of soft tissues and lymph nodes;
- extensive injuries, burns, frostbite - such factors most often provoke elephantiasis of the legs;
- advanced venereological diseases in severe form;
- surgery to remove lymph nodes.
Secondary elephantiasis is often accompanied by venous disease.
Since damage to the lower extremities occurs most often, this etiology should be highlighted separately.
Causes of elephantiasis in the feet include:
- previous operations on the legs affecting blood vessels;
- frequent and prolonged hypothermia;
- constant static load;
- varicose veins in chronic form;
- vasculitis
Elephantiasis lymphostasis is a serious disease, so special attention should be paid to prevention, since it is impossible to completely recover from it.
Pathogenesis
Elephantiasis begins with slight swelling and swelling, which may subside or reappear. Eventually, after about 1-3 years, there is a two to threefold thickening of the lower leg and possibly the thigh if the leg is affected. The shape of the leg is awkward and cylindrical, turning into thickenings, for example, the deepening of the ankle joint can be smoothed out.
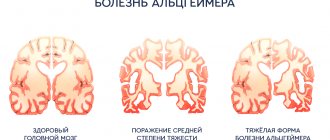
Stages of development of elephantiasis
The mechanism of excessive thickening of the affected parts is based on stagnant processes affecting the lymphatic system. They can arise as a result of factors such as:
- blockage of lymphatic vessels by parasites - nematodes , for example, filaria , chyluria , etc.;
- suppuration and subsequent scarring of the lymph glands, for example, the inguinal glands;
- inflammation of the lymphatic vessels with lymphangitis , phlebitis , erysipelas , varicose ulcers, chronic eczema , syphilis , lupus , with repeated frostbite and other chronic or recurrent processes leading to inflammatory edema.
The resulting stagnation of lymph leads to its penetration into tissue crevices and provides excessive nutrition to the structures of adjacent tissues, which causes hyperplasia as a result of the proliferation of connective tissue in the subcutaneous tissue. This process is chronic, lasts for many years, and therefore is practically undetectable in adolescents.
Attention! Wuchereriosis and other filariasis are caused by parasitism in the human body of very thin worms (no more than 0.3 mm in diameter, up to half a meter long) that can block the lymphatic system. They are spread and dispersed by blood-sucking insects, so it is extremely important to protect yourself with repellents and mosquito nets when on vacation in tropical countries, because they can not only cause elephantiasis, but also penetrate into the eyes, causing blindness .
Causes of elephantiasis of the feet
There are two main causes of elephantiasis:
- congenital or acquired disorders in the lymphatic system, including overproduction of lymph, defects, aplasia, insufficiency of the valve system, stenosis and occlusion of lymphatic vessels, as well as diseases such as Nonne-Milroy syndrome, Shereshevsky-Turner syndrome ;
- infectious, more often parasitic agents, which include Bancroft's filamentum - causes wuchereriosis , but there may also be a streptococcal infection;
- mechanical injuries and thermal burns (usually repeated frostbite);
- tumors that can compress the lymphatic capillaries;
- Iatrogenesis - can be caused by radiation or surgery;
- disorders of the circulatory system - chronic venous insufficiency and postthrombophlebitic syndrome ;
- damage to the central nervous system;
- endocrine disorders.
Life cycles of various representatives of filariae
Elephantiasis, caused by various parasitic roundworms (filariasis), is more common among residents of tropical zones (Indian archipelago, Arabia, the west coast of Africa, Central America), where mosquitoes spread and transmit the infection. In the former CIS countries it is very rare.
Diagnosis of elephantiasis of the lower extremities
If the symptoms described above appear, do not delay visiting your doctor. The treatment of diseases of the lymphatic system is carried out by a specialized specialist - a lymphologist. If you do not have the opportunity to visit this doctor, make an appointment with a phlebologist or angiosurgeon: since the lymphatic and circulatory systems function interconnectedly, a vascular specialist can tell you how to treat elephantiasis in the legs.
To make an accurate diagnosis, not only a medical examination is important, but also additional research. This is especially necessary in the initial stages of elephantiasis, when its symptoms may be mistaken for manifestations of vascular diseases (in particular, thrombosis). Before starting treatment for elephantiasis, the following diagnostic procedures are recommended:
- Dopplerography of blood vessels.
- Lymphangiography.
- CT.
- MRI.
- Laboratory tests: general and biochemical blood test, serological test, blood test after taking Diethylcarbamazine. The latest study reveals the presence of filaria in the human body.
- Performing the McClure-Aldrich test.
Methods for treating elephantiasis of the feet
Symptoms of elephantiasis
In addition to hypertrophy and hyperplasia - swelling, changes in shape and increase in size of the pathologically altered part of the body, patients may experience symptoms such as:
- the occurrence of papillomatous growths, ulcers and warts (as in the photo below, elephantiasis of the legs);
- the skin may become shiny, pale or bluish, and does not fold;
- lymphatic and venous stasis;
- edema;
- pain;
- stiffness of movements;
- the development of hypertrophic processes in the layers of skin and subcutaneous tissue, caused by an increase in intermuscular space as a result of the proliferation of connective and bone tissue, which ultimately causes thickening of the bone.
Patient with elephantiasis
If the disease is caused by erysipelas , then in the affected area of a sharply elevated painful ridge, a burning sensation, redness (erythema), increased temperature, pinpoint hemorrhages, erosions, trophic ulcers, blisters may occur, which may subside, forming brown crusts.
Erysipelas on the leg
Stages of the disease
At an early stage, lymphedema is quite difficult to recognize: it appears in the evening and disappears after a night's rest. The limbs feel soft to the touch, and patients may confuse them with swelling that occurs after exercise. As the disease progresses, lymphedema increases, becomes permanent, and becomes dense. The skin in the area of the second toe cannot be folded (positive Stemmer's sign). Swelling begins on the foot and spreads higher up the leg.
When the disease reaches the third stage, doctors talk about elephantism, or elephantiasis. The disease leads to the fact that one leg is seriously different in size from the other (if lymphedema is observed only on one limb), it is difficult, and sometimes impossible, for the patient to choose clothes or shoes, and it is difficult to move. The swelling becomes dense, since the lymph contains a lot of protein, and the penetration of protein molecules into the tissue leads to the formation of fibrous fibers there. Elephantiasis is accompanied by the appearance of papillomas on the skin, vesicles from which lymph may leak.
Tests and diagnostics
To confirm the diagnosis of filariasis, clinical data and epidemiological history information, results of laboratory and instrumental research methods are studied. The most important factor is the detection of microfilariae in blood tests using microscopy at low magnification. In addition, immunological techniques can be used, but they do not give strictly specific results.
If the nature of the pathology is not parasitic, then a more complete picture can be given by ultrasound of the lower extremities, rheovasography, lymphography, duplex scanning of blood vessels, radiography and MRI. In addition, general blood tests, urine tests, and a blister test may be performed during the examination.
Prevention
Elephantiasis is a disease spread by mosquitoes. Prevention can be carried out in the following ways:
- avoid mosquitoes or take precautions to reduce the risk of mosquito bites;
- avoid mosquito breeding areas;
- use of mosquito nets;
- wearing insect repellent;
- wear long-sleeved shirts and pants in areas with a lot of mosquitoes;
- purchase diethylcarbamazine (DEC), albendazole and ivermectin as prophylaxis before traveling to areas where elephantiasis is endemic.
In men
In addition to enlargement of the lower extremities, the pathology can affect the external genitalia. In men, this is the scrotum, which as a result resembles a sac-like tumor and can reach colossal sizes - up to 54 kg of weight, hanging down to the level of the knees and even the floor. In this case, elephantiasis develops in the form of dropsy of the membranes of the testicles - hydrocele. Microfilariae are found in the fluid punctate.
Elephantiasis of the scrotum
Elephantiasis can also spread to the penis, but does not affect the cavernous bodies, urethra and testicles. As with elephantiasis of other parts of the body, the scrotum, perineum and foreskin may become covered with warty and papillomatous growths, and hyperkeratosis , ulcerations, excoriations or eczematous dermatitis If a secondary staphylococcal or streptococcal infection has been associated, the pathology may acquire a purulent-septic character.
Elephantiasis of the scrotum is extremely dangerous, because hypertrophy of the foreskin makes urination difficult, disrupts sexual function, making erection painful and causing impotence .
Among women
Women can also suffer from elephantiasis and, like men, the external genital area, that is, the labia majora and minora, can be affected. Such rare cases are more typical for tropical latitudes; in our climate, elephantistic enlargement of the external genital organs occurs only in women providing paid sexual services. The affected parts can become deformed and reach the size of a fist, sometimes become covered with bubbles that can easily burst and release a clear liquid - lymph, which coagulates in the air. This usually occurs as a result of dilation of the lymphatic vessels and may be accompanied by massive discharge - lymphorrhea .
Diet for elephantiasis
Diet for lymphostasis of the lower extremities
- Efficacy: no data
- Timing: as prescribed by the doctor
- Cost of products: 1500-1600 rubles. in Week
Swelling and impaired lymphatic drainage require compliance with a special drinking regime and diet. The main recommendations include:
- eating easily digestible foods;
- enriching the menu with dishes containing rice, peas, lentils, as well as vegetable soups and, in general, boiled food;
- maximum limitation of salt and white sugar consumption; for an afternoon snack, ripe fruits and salads made from them are best suited;
- ban on fried and fatty foods;
- eliminating coffee, black tea, and tobacco completely;
- Your daily diet should include a glass of light cow's or coconut milk, water with honey, orange, pomegranate or grape juice.
Consequences and complications
thrombophlebitis or erysipelas (usually with streptococcal infection) can develop against the background of elephantiasis All these changes can lead to:
- lymphostasis or in other words - lymphedema ;
- possible addition of purulent-septic infections;
- malignancy of papillomas ;
- lymphorrhea , ulcers , eczema and muscle atrophy, since the upper integument and muscle tissue also suffer due to lack of trophism.
Elephantiasis can significantly limit freedom of movement, since it is much more difficult to walk on “heavy legs”; this may also be partly due to the degeneration of muscle tissue. As a result, all this can lead to complete immobilization and disability.
Drug therapy
At the first stage of elephantiasis the following are used:
- antihistamines to relieve allergic reactions (Loratadine);
- anthelmintic drugs that prevent parasites from multiplying (piperazine);
- angioprotectors to normalize tissue nutrition (Rutoside);
- pyridoxine to improve metabolism.
At the second stage of the disease, the following is prescribed:
- angioprotectors for relaxing vascular muscles (Troxerutin);
- enzymes to normalize the state of fiber (Lidase);
- non-steroidal anti-inflammatory drugs (Reopirin);
- desensitizing drugs to relieve inflammation (Claritin);
- biostimulants that soften connective tissue;
- vitamins.
At the third stage, to maintain the body, the following is prescribed:
- angioprotectors to reduce edema (Troxerutin);
- antibiotics to destroy infection in diseased tissues (Azithromycin);
- venotonics to improve fluid circulation in blood vessels (Detralex).