Alcoholic liver disease (ALD) is a complex of pathological changes in the liver, the development of which is caused by chronic alcohol consumption in toxic doses.
About 30% of all diffuse lesions of liver tissue are associated with ALD1. Long-term consumption of alcoholic beverages negatively affects all organs and systems, including the liver. The fact is that ethanol in the liver cells is metabolized into acetaldehyde, which has a toxic effect on the cells.9 It is worth noting that women, on average, have lower activity of the enzyme that produces acetaldehyde compared to men, which explains more severe ALD among women and the development of alcohol-induced liver damage in a shorter period of time and at lower doses of alcohol consumed1 (20 g/day for women compared with 30 g/day for men).10
Liver cirrhosis in Russia
In most developed countries, ALD is one of the most common diseases, diagnosed in 10-25% of men and slightly less frequently among women2. WHO (World Health Organization) studies have shown that liver cirrhosis in Russia ranks sixth among all causes of mortality2.
ALD could be called alcoholic fatty liver disease, which is associated with the development of fatty liver in the first stage of the disease with systematic consumption of ethanol in high doses.1 This phenomenon, the accumulation of fat in liver cells, also occurs in non-alcoholic fatty liver disease.
Relevance of the problem
The problem of excessive alcohol consumption and its consequences has long attracted attention in almost all countries of the world. According to official statistics, the highest consumption is observed in European countries, where about 50% (58 million people) drink alcohol excessively. Per capita alcohol consumption among persons over 15 years of age is 11 liters of ethanol per year.
How does the liver react to alcohol?
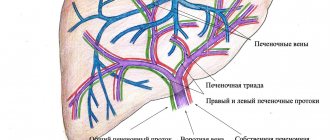
Under the influence of alcohol, processes are launched in hepatocytes (liver cells) that lead to the destruction of cell membranes, substances are produced that destroy liver cells and block the mechanisms of regeneration (restoration) of the liver.
Long-term exposure of the liver to toxic doses of alcohol leads to the formation of dense fatty tissue instead of destroyed liver cells. It does not perform the numerous functions that are characteristic of liver cells, which provide basic vital processes in the body. The terminal stage of the disease is characterized by the development of hepatic cellular failure.
In addition, dense adipose tissue interferes with normal internal circulation with a subsequent increase in pressure in the portal vein (portal hypertension) and an enlarged spleen. A real threat to life is internal bleeding from the dilated veins of the stomach and esophagus.
With the same alcohol consumption in different people, the severity of liver damage depends on their individual sensitivity to the toxic effects of alcohol. In this case, gender, age, genetic characteristics, type of drinks consumed, the presence of hepatitis viruses, iron overload and other factors matter.
The amount of alcohol consumed per day and its quality are also important prognostic indicators of its effect on the liver.
Reasons for development
The main reason for the development of ALD is alcohol abuse. Doses exceeding 30 ml of vodka (cognac, whiskey), 150 ml of wine or 250 ml of beer per day for women and 60 ml of vodka (cognac, whiskey), 300 ml of wine or 500 ml of beer per day for men are considered dangerous. The fact of abuse is easy to determine using a special questionnaire (CAGE). This is evidenced by at least two positive answers to the following questions:
- Have you ever thought that you should reduce your alcohol consumption?
- Does it happen that people who criticize your alcohol consumption irritate you?
- Do you feel bad or guilty after drinking alcohol?
- Do you sometimes drink alcohol in the morning to improve your mood or get rid of a hangover?
Additional risk factors for liver damage are:
- drinking beer or strong alcohol;
- malnutrition;
- drinking alcoholic beverages on an empty stomach;
- female;
- deficiency of vitamins A and E, protein;
- excess polyunsaturated fats in the diet;
- obesity and overweight;
- hepatitis C;
- hereditary predisposition.
Mechanism of treatment of the syndrome
The goal of treatment is to stop the further development of liver disease and stop necrosis of organ cells. The most important thing is that the patient completely stops drinking alcohol. Diet is also a significant factor in recovery. The patient needs to be provided with good nutrition with vitamin supplements and plenty of fluids.
Diuretics and antihypertensive drugs are also used in therapy. They lower liver blood pressure. If liver function is so poor that waste products such as ammonia are not eliminated naturally, they affect the brain and liver failure (hepatic encephalopathy) develops. Since ammonia is produced in the colon, its elimination can be increased with the help of laxatives. Cirrhosis is treated with antibiotics and protein-rich diets.
In cases of severe jaundice and alcoholic inflammation, they are treated with the adrenal cortical hormone - prednisole.
Mechanisms of liver damage
A key role in alcohol damage to the liver is played by ethanol and its more toxic derivative, acetaldehyde. Several mechanisms of damage can be distinguished.
- Firstly, alcohol promotes increased formation of fatty acids and reduces their oxidation. This leads to the accumulation of excess fat in liver cells (hepatocytes), that is, to the development of fatty degeneration.
- The second mechanism of liver damage is associated with the oxidation of alcohol by enzymes, in particular alcohol dehydrogenase. As a result, free oxygen radicals (oxidative stress) and acetaldehyde are formed in excess, which have a damaging effect on its cells.
- The third mechanism is due to increased permeability of the intestinal wall. As a result, lipopolysaccharides (waste products of gram-negative intestinal flora) penetrate through the blood into the liver, where they stimulate the production of proinflammatory cytokines by Kupffer cells - biologically active substances that cause inflammation.
- The fourth mechanism is associated with free radical activation of the immune system and immune-mediated inflammation and liver damage.
The consequence of inflammation is the destruction of hepatocytes (cytolysis), their death (necrosis) and the proliferation of connective tissue (fibrosis). Progressive fibrosis leads to disruption of the normal lobular structure of the liver - cirrhosis, and subsequently to primary cancer - hepatocellular carcinoma.
Tests needed for alcoholic liver disease
The examination is carried out to clarify the extent of liver damage by alcohol. This information is obtained using biochemical blood tests, which characterize how correctly the liver cells function and how actively they are being destroyed by alcohol. Biochemical tests include indicators of cytolysis (ALT, AST, GGT), functional indicators of the state of liver cells (protein fractions and total protein), indicators of cholestasis (bilirubin, etc.). Indirect signs of liver damage are a clinical blood test and coagulogram, as well as all indicators of iron metabolism.
Ultrasound diagnostics can reveal: an inflammatory process in the liver, an increase in its size, a change in the structure of the liver tissue. In addition, it is possible to assess the speed of blood flow in the portal vein, which decreases when dense adipose tissue forms in the liver, preventing the free flow of fluid.
An important indicator is the diameter of the main vessels, which indicates pressure in the portal system and the possible presence of portal hypertension, which may also be accompanied by an enlarged spleen.
To clarify the degree of liver damage with its possible transformation into cirrhosis, it is necessary to perform elastometry using the FibroScan device, or other, preferably non-traumatic, methods to assess the degree of fibrosis (FibroMax, FibroTest). It is characterized by degrees from 0 to 4, fibrosis degree 4 allows a diagnosis of cirrhosis.
The cost of the examination is about 25,000 rubles.
Symptoms of the disease
ALD can be asymptomatic. However, symptoms of alcoholic liver damage may be nonspecific. These include complaints such as heaviness or pain in the right hypochondrium, bloating, abnormal stool, nausea, etc.
In addition to the liver, other organs and systems may be involved in the pathological process. In particular, there may be atrophy of the muscles of the shoulder girdle, impaired sensitivity in the extremities (polyneuropathy), heart disease (cardiomyopathy), and pancreas disease (pancreatitis).
What complications occur at different stages?
As patients continue to drink alcohol, alcoholic steatosis will necessarily progress to the following stages: hepatitis, fibrosis, cirrhosis of the liver. The consequences of alcoholic hepatitis can be:
- brain damage (encephalopathy);
- manifestations of hemorrhagic syndrome with hemorrhages in internal organs;
- hepatorenal syndrome, accompanied by blocking the filtration function of the kidneys with renal failure;
- hypoglycemic state;
- bacterial peritonitis due to infection;
- in the chronic course - hypertension in the portal vein system, ascites.
The development of complications indicates a poor prognosis. The fibrosis stage progresses to liver cirrhosis and is accompanied by:
- hypertension in the portal venous zone with bleeding from the veins of the esophagus and stomach;
- development of renal and hepatic failure;
- anemia;
- severe ascites and swelling in the legs;
- decompensation of cardiac activity, arrhythmias;
- high risk of developing into cancer.
Diagnosis of the disease
Laboratory methods
Laboratory symptoms are primarily
- increased levels of liver enzymes: ALT (alanine aminotransferase) and AST (aspartate aminotransferase) in the blood, with an AST:ALT ratio > 1.5.
- increased blood levels of gamma-glutamyl transpeptidase (GGT), a carbohydrate-deficient transferrin
- reduction in the size of blood cells - red blood cells (erythrocyte microcytosis).
Ultrasonography
Ultrasound examination (US) can detect an increase in the size of the liver (hepatomegaly), its heterogeneity and increased echogenicity. In addition to ultrasound, computed tomography (CT) and magnetic resonance imaging (MRI) are used as imaging methods.
Biopsy
The diagnosis and stage of the lesion can be accurately determined by biopsy. A non-invasive alternative to biopsy is elastography. It is a timely diagnostic method that allows you to assess the elasticity of organ tissue using an ultrasound sensor.
Establishing diagnosis
The doctor determines the duration of alcohol use or the degree of alcoholism. Based on these data, the patient is prescribed a medical examination. Both general diagnostics and blood tests can determine the extent of liver damage. For this purpose the following is carried out:
- Lab tests.
- Histological studies.
- Ultrasound. To have a visual idea of the disease picture, an ultrasound examination of the liver is performed.
- Biopsy. To do this, the doctor removes a tissue sample using a needle.
- Magnetic resonance and computed tomography.
Treatment methods for ALD
Drug and non-drug approaches to therapy can be distinguished.
Medication
Non-drug treatment requires complete abstinence from alcohol .
Medication
A drug for the treatment of alcoholic liver disease should have an antioxidant effect, suppress inflammation and prevent the progression of fibrosis. Such a drug is Phosphogliv*
, which has demonstrated all these effects in clinical studies. It should be taken 2 capsules 3 times a day with meals, without chewing, with a small amount of liquid. The course duration is usually 3 months.
If you suspect the development of liver disease, you should consult a doctor.
Pathogenesis
The disease can develop over a long period of time: months and years. The pathological influence of viruses on liver cells, toxic substances (drugs, alcohol), impaired blood supply to the organ, immune mechanisms, and the influence of inflammatory mediators lead to massive death of hepatocytes and replacement with connective tissue. This process disrupts all vital functions of the liver.
- 1. Fatty degeneration. Initial changes in the structure and function of hepatocytes, which can completely disappear within a few weeks if the intake of alcohol in the body is stopped.
- 2. Steatohepatitis. An inflammatory process develops. The structure and size of hepatocytes change; in severe cases, the cells die, which affects the general condition of the liver. At this stage, disturbances in the functioning of the organ already occur, and specialized treatment is also required.
- 3. Cirrhosis. The formation of irreversible fibrous changes in the organ, disruption of the general structure: the appearance of tuberosity, reduction in size. If left untreated, the condition progresses and liver functionality decreases. Dangerous complications develop not only in the organ itself, but also in the structures dependent on it.
The sooner you consult a doctor and, most importantly, stop drinking alcohol, the higher your chances of getting rid of the problem.
Differential diagnosis with non-alcoholic fatty lesion
Non-alcoholic steatohepatitis or fatty liver disease (NAFLD) is a fairly common type of pathology. In different countries, it affects from ¼ to half of the population.
It is observed more often in women aged 40–60 years, in children with metabolic disorders accompanying:
- obesity;
- hypertension;
- diabetes;
- hormonal disorders;
- taking corticosteroid medications, contraceptives;
- poor nutrition (both the predominance of easily digestible carbohydrates and fats, and sudden weight loss during fasting).
Acute fatty hepatosis can be triggered by pregnancy. Disease activation factors include:
- chronic pancreatitis;
- stomach or duodenal ulcer:
- gout;
- lung diseases;
- psoriasis;
- systemic pathology of connective tissue.
The process of disruption of fat metabolism begins with the accumulation of triglycerides in the liver tissue
Normally, triglycerides are broken down to release energy. In pathological conditions, their excessive quantity can:
- deposited inside the cytoplasm of cells;
- disrupt the integrity of cell membranes;
- activate fibrosis processes.
Patients complain:
- for weakness, fatigue;
- heaviness and pain in the abdomen;
- headache;
- bowel disorders.
In advanced cases, an enlarged liver and spleen are detected. The important differences are:
- no long-term alcohol history;
- increased weight of patients;
- a significant increase in triglycerides in the blood test;
- hyperglycemia;
- 40% of patients have skin pigmentation in the neck and armpits.
Among the clinical manifestations, jaundice indicates concomitant hepatitis, which is rare.
Content:
- Etiology.
- Pathogenetic mechanisms of liver intoxication.
- Clinical picture of alcoholic liver intoxication: 3.1. Steatosis. 3.2. Alcoholic hepatitis. 3.3. Cirrhosis.
- Diagnostics.
- Principles of treatment: 5.1. Nutrition correction. 5.2. Drug treatment.
Alcoholic liver intoxication refers to the sequential development or combination of several diseases: steatosis (fatty degeneration), hepatitis and cirrhosis. In this case, the pathology can be asymptomatic (or with a “blurred”, non-specific clinical picture) until the development of irreversible changes. According to WHO, alcoholic liver poisoning is the most common disease in hepatology.
Fatty liver hepatosis, treatment
Fatty liver
without the presence of fibrosis is not a precirrhotic condition. When you stop drinking alcohol, the organ structure is usually restored within 4-6 weeks.
With fatty liver hepatosis
a diet with a sufficient amount of protein, polyunsaturated fatty acids (vegetable oils, fish), preparations containing silymarin (hepatoprotectors-antioxidants), multivitamin pills containing microelements is prescribed, zinc is especially important, since it is a component of the enzymes alcohol dehydrogenase, superoxide dismutase (antioxidant body system), enzymes that stimulate the immune system.
In addition to the diet for the treatment of fatty liver disease
vitamins are needed. You should definitely prescribe alpha-tocopherol either with vitamin preparations, or increase the consumption of vitamin E-containing products: mainly unrefined vegetable oils, yolk, nuts, buckwheat, parsley, sprouted wheat seeds.
License and certificates:
Liver decomposition from alcohol
Due to the effects of alcohol, cell scarring occurs. Scar tissue replaces healthy cells, and the “filtration” functions of the gland disappear. Inflammation and cell death lead to complex intoxication of the body: bilirubin increases, waste products, toxins and other dangerous substances circulate freely through the blood vessels. Encephalopathy and other diseases are observed, as a result of which a person dies within 5-6 months.
Etiology
The most obvious reason for the development is long-term abuse of alcoholic beverages. In this case, not only the amount of alcohol matters, but also the frequency of drinking episodes and the specific type of strong drinks. For most people, the critical dose of ethanol is 80–160 g per day over 10–20 years of regular drinking.
But in women, the disease develops when drinking much smaller doses of alcohol (20–40 g per day) and over a shorter period. This is explained by the smaller number of enzymes involved in the breakdown of ethanol. And if therapy is started too late, in 50% of women the pathology progresses to hepatocellular carcinoma, even if they get rid of addiction.
According to experts, one-time alcoholic excesses (even with significant alcohol abuse) are safer, since a rare intake of alcohol gives the liver the opportunity to “recover”, which cannot be said about daily drunkenness.
In addition, the risk of alcoholic liver toxicosis is increased if:
- genetic characteristics due to which the mechanisms for the production of enzymes that affect the metabolism of alcohol are disrupted;
- being overweight, which provokes the accumulation of visceral fat;
- concomitant viral and infectious liver diseases;
- taking hepatotropic medications (antifungals, antibiotics, immunosuppressants), antiulcer medications that reduce the activity of alcohol dehydrogenase;
- autoimmune diseases.
Treatment of alcoholism in Moscow
The drug treatment clinic “AlkoZdrav” provides professional treatment for alcohol addiction in Moscow. We use certified medications, resort to modern psychotherapeutic programs and are guided by the principles of an individual approach to each person. It is important to note that treatment at AlkoZdrav is carried out strictly anonymously.
Diagnostics
Diagnosis is the first link in the chain of treatment of liver pathologies. To determine the condition of the gland, it is necessary to take a general blood and urine test, undergo an ultrasound, and take markers (cytolysis, cholestasis). In severe cases, a biopsy is necessary. After a visual examination and medical history, the doctor determines the current diagnostic method.
Alcohol detoxification
The most common methods of detoxification from ethyl alcohol include:
- Placement of IVs to cleanse the bloodstream;
- Taking enterosorbents;
- Carrying out injections;
- Resorting to the help of specialized devices (plasmapheresis, UBOD, etc.).
Detoxification is necessary to remove waste and toxins from the body. The procedure must be carried out with the participation of medical personnel.
Drug therapy
Pharmacotherapy is carried out with the aim of accelerating detoxification processes, relieving symptoms of the disease and restoring the functions of organs and systems. The current group of drugs is determined only by a narcologist. Self-medication may lead to adverse reactions.
Alcohol rehabilitation
Rehabilitation in a specialized center is necessary to restore the body and psychological state of a person.
During the rehabilitation process, the clinic resident undergoes intensive individual and group psychotherapy and struggles with psychological dependence on psychoactive substances. Together with a specialist, a person works through psychological problems, learns the principles of social adaptation, shows an active social position, and learns to live in sobriety.
What does the liver of an alcoholic and a healthy person look like?
Photo 1: On the left you can see the so-called “nutmeg liver”, the cells of which are completely destroyed
The photo shows a comparison of gland preparations from an alcohol-dependent person and a healthy liver. Ethyl alcohol causes the destruction of hepatocytes (liver cells), an increase in the volume of the gland due to fat and severe malaise.