Endocrinologist
Tananakina
Natalia Vasilievna
Experience 26 years
Endocrinologist, Candidate of Medical Sciences
Make an appointment
Myxedema is one of the endocrine diseases. The pathology develops as the volume of thyroid hormones produced by the thyroid gland decreases. With a stable negative state of the organ, the disease quickly develops and reaches the level of myxedema - an extreme form of hormone deficiency. Modern medicine has enough experience in diagnosing this pathology and is ready to offer a course of treatment based on hormone replacement therapy, which allows stabilizing the patient’s condition.
Causes of myxedema and their classification
If hypothyroidism is detected in a patient in a timely manner and effective treatment is prescribed, the lack of hormones can be compensated without consequences for the body. Otherwise, the patient experiences a deterioration in his condition and the appearance of symptoms of myxoedema. The causes of myxedema are the following conditions:
- In the primary form of myxedema, the cause is primary hypothyroidism caused by disturbances in the functioning of the thyroid gland. The latter fact can be caused by radiation, surgery, iodine deficiency or excess.
- The secondary form of myxedema is caused by disorders of the pituitary gland or hypothalamus, which are involved in the production of thyroid hormones.
- Pretibial myxedema is caused by an excess of iodine-containing hormones, which are produced by an enlarged thyroid gland when a multinodular toxic goiter is diagnosed.
- The idiopathic form is a disease for which it is not possible to accurately determine the cause. At the same time, the thyroid gland and other elements of the body’s hormonal system work stably, and an excess or deficiency of thyroid hormones is not detected in the patient’s blood.
Pretibial myxedema
Separately, it is necessary to consider a disease such as pretibial myxedema, or thyroid dermopathy. Unlike classic myxedema, pretibial myxedema occurs not with decreased, but with excessively increased thyroid function, the so-called thyrotoxicosis. The cause of thyrotoxicosis is most often diffuse toxic goiter, more popularly known as Graves' disease.
Pretibial myxedema has local manifestations, in contrast to ordinary myxedema, which manifests itself diffusely. A symptom of pretibial myxedema is the appearance of modified areas of skin on the lower part of the anterior surfaces of the legs. The skin in these areas becomes rough, thickens, acquires a red or purple-red color, and increased keratinization is noted. Protruding hair follicles appear on the affected areas of the skin, and subsequently the hair falls out.
External symptoms of pretibial myxedema are sometimes accompanied by a feeling of severe itching. Treatment of pretibial myxedema is carried out in combination with the correction of thyroid disorders that caused the disease. Local treatment of myxedema, when the disease is accompanied by itching, consists of using ointments containing steroidal anti-inflammatory drugs. In most cases, patients with pretibial myxedema are only concerned about a cosmetic defect, and then special treatment for myxedema is not carried out, but the underlying disease is treated.
Symptoms
We can talk about the development of the consequences of a lack of thyroid hormones based on the following characteristic symptoms of myxedema:
- Severe swelling of the skin and subcutaneous tissue on the face and body without signs of redness and loosening of the structure.
- Puffiness of the face, resembling a mask.
- Simplification of facial expressions, immobility of features during conversation.
- Difficulty in nasal breathing due to swelling of the mucous membrane.
- Hoarseness, hoarse voice due to swelling of the larynx, cough.
- Shortness of breath even with slight exertion.
- Lethargy and drowsiness of the patient.
- Muscle weakness, lethargy, memory problems.
- Muscle pain and headaches.
- Decreased appetite, high likelihood of signs of constipation.
For children, a lack of thyroid hormones causes a slowdown in development and impaired tooth formation. The appearance takes on rough features: the eyes are deep-set, the tongue is enlarged, the nose is wide and flat. Speech and self-care skills may be partially or completely absent.
Pretibial myxedema, which develops against the background of an excess of thyroid hormones, is characterized by thickening of the skin of the legs, hair loss and severe itching. Tachycardia develops, pain in the heart area increases, muscle weakness and instability of the emotional state are noted. As the patient's appetite increases, the patient's body weight decreases.
Hypothyroidism (myxedema)
Signs
The manifestations of hypothyroidism are varied, but in its expressed form it is characterized by clearly defined complaints and objective indicators.
Primary hypothyroidism mainly occurs in women. If you characterize their state in one word, then it is “lethargy,” and if in one phrase, then “for some reason you don’t want anything.” All the time, no matter how they dress, they are cold, chilly, no matter how much they sleep, they still get tired quickly. My memory is out of my hands, my tongue is a little slurred. With hypothyroidism, the face and limbs swell, but in a peculiar way - when you press with a finger in the area of the front surface of the lower leg, there is no hole left. The skin is dry, pale, with a yellowish tint. Elbows and heels are generally like sandpaper. This change in the skin is associated with decreased function of the sweat and sebaceous glands. The nails are no good - they peel, bend, even tear across. The voice is always hoarse or hoarse at the slightest excitement, because the vocal cords are swollen. The hair on the head, on the lower third of the eyebrows and pubic area is brittle, fragile, and falls out in large quantities. Body temperature is lowered, as is blood pressure, although 10-20% have hypertension. Bradycardia is observed (a decrease in heart rate to less than 55 beats per minute), and in advanced conditions, tachycardia occurs (an increase in heart rate to more than 90 beats per minute). The limbs are thickened. The fingers are thick and give the impression of being short. The body of people with hypothyroidism usually does not sweat, but only the hands may sweat. Hard-to-treat acne and acne-like rashes often appear on the face and back. There is also a disturbance in the sense of smell and taste. Due to the swelling of the nasal mucosa, nasal breathing is difficult, which contributes to the development of inflammatory processes in the upper respiratory tract. By the way, infectious diseases in people suffering from hypothyroidism often occur with a low temperature, which is associated with a slow metabolic rate.
If hypothyroidism is not adequately treated, a puffy face, slow speech may appear (the tongue, which has begun to “occupy” most of the oral cavity), “bags” under the eyes, a narrow palpebral fissure, and expressionless gaze (which is explained by myxematous edema, which cannot be treated even with diuretics).
It should be remembered that at first the increased load on hormone production is compensated and does not cause changes in the thyroid gland and does not manifest any signs. But later, to perform the task of producing hormones in the gland, its tissue is transformed, a general and/or local increase in follicles develops, thereby forming a diffuse and/or nodular goiter.
Patients with these changes are usually found to be in a euthyroid state, i.e. normal amount of hormones. A decrease in the level of thyroid hormones in combination with additional symptoms may indicate a transition to a state of subcompensation (i.e., a greater deficiency of the functional capabilities of the gland). At the same time, an increase in the amount of pituitary hormone (thyroid-stimulating hormone - TSH) is natural, since it controls the activity of the thyroid gland. When the activity of the gland is restored, the TSH level returns to normal. Doctors call this condition (normal levels of T4 (thyroid hormone) and high TSH) subclinical hypothyroidism, meaning that the body copes with the load of hypothyroidism itself, i.e. low levels of thyroid hormones, not yet. If the T4 level is below normal and TSH is higher, then doctors talk about manifest (manifest) hypothyroidism. This is true hypothyroidism, and it must be treated.
Description
Hypothyroidism is a condition characterized by a persistent decrease in thyroid function associated with low levels of thyroid hormones and leading to metabolic and clinical disorders. A lack of thyroid hormones in the body causes a slowdown in all its functions. The exception is the thyroid-stimulating function of the pituitary gland, which increases compensatoryly.
Most people suffering from hypothyroidism develop anemia (anemia). In some cases, it precedes the clinical manifestations of thyroid insufficiency. Anemia occurs as a result of decreased absorption of iron in the intestines.
Disturbances in the activity of the nervous system in hypothyroidism are manifested by headaches and pain in the limbs. Lower back pain occurs as radiculitis. Women experience disturbances in sexual function and the menstrual cycle, menopause may occur prematurely, and in men, potency sharply decreases.
Insufficiency of thyroid hormones in the body also contributes to the deposition of cholesterol on the walls of blood vessels, primarily heart ones, which leads not only to their hardening, but also to a narrowing of the lumen. At the same time, compressive pain (like angina pectoris) appears in the area of the heart, colloquially called angina pectoris. True, despite serious changes in the heart (both in the vessels and in the muscles - the myocardium), complaints of pain in the heart area are rare. And only with too pronounced changes, with a sharp narrowing of the lumen of the coronary (i.e., heart) vessels, patients notice angina pain.
If there are disturbances in the activity of the gastrointestinal tract, which is often observed with reduced thyroid function, patients often complain of decreased appetite, flatulence, and constipation. A change in the process of fat metabolism leads to slow absorption of fats by tissues and increased deposition of cholesterol plaques on the walls of blood vessels.
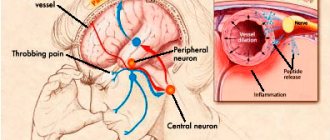
With hypothyroidism, the function of the central and peripheral nervous systems is impaired, which manifests itself in changes in neuropsychic functions, cranial innervation, and motor sphere. As a result, a person becomes slow, apathetic, with slow speech and unexpressive facial expressions, and many reflexes are reduced.
Hypothyroidism is characterized by memory disorders and intellectual disability. These disorders, the depth of which depends on the duration of the disease, determine different degrees of severity of dementia, which can vary in these cases from mild debility to idiocy. The latter is observed only if hypothyroid deficiency was congenital or acquired from early childhood, was not diagnosed in a timely manner and was not treated properly. But, fortunately, cretinism and idiocy of endocrine origin are practically never encountered today, at least in our country. Nowadays, hypothyroidism is widespread, occurring in a mild form, when the psyche only shows slowness of thinking and speech, memory loss, mental and, of course, physical fatigue, which is manifested in a somewhat retarded facial expression, its puffiness and roundness, and a slightly open mouth.
With severe hypothyroidism (moderate severity of the disease), indifference and apathy are noted; such people rarely laugh or cry. Sometimes irritability, grouchy, depressed mood and depression may occur. But if this is not actively treated, then the disease passes into a more severe stage, which is characterized by emotional dullness, indifference to the environment, or monotonous good nature. People suffering from hypothyroidism can also be angry and unfriendly, so much so that their uncontrollable fits of rage can frighten even close people who are aware of the disease. Electrocardiography (ECG) can record dystrophic changes in the heart muscle. In more severe, advanced cases, heart failure develops. The liver may be enlarged.
With hypothyroidism, degenerative lesions of the heart and blood vessels are possible, which is fraught with myocardial infarction, as well as neuropsychiatric disorders. But the most dangerous complication is hypothyroid coma, which develops in patients with thyroid insufficiency and is provoked by cooling, infection (influenza, pneumonia), surgery, taking sleeping pills, sedatives, and narcotic drugs. They can become trigger factors in the development of complications of hypothyroidism, since they have been proven to reduce the activity of metabolic processes (including heat generation), which in patients are already in a state of minimal activity.
When a precomatous state occurs, the symptoms of hypothyroidism worsen: breathing becomes rare, heart failure increases, and brain hypoxia develops (anemia accompanied by oxygen starvation).
With the development of hypothyroid coma, the low body temperature decreases even more (below 35°C), and therefore the hypothyroid coma is called hypothermic.
Hypothyroid coma has two phases: precoma and coma. In the first phase, confusion of consciousness is noted, sometimes convulsions and a stuporous state appear (numbness, immobility, depression of mental activity, lack of verbal communication with others, decrease in all types of sensitivity). In the second phase, a deep loss of consciousness or coma occurs, which in most cases ends in death. This means that at the first symptoms of a developing hypothyroid coma or even at the appearance of the first signs of a precomatous state, urgent hospitalization is necessary. But it is much wiser not to wait for such a condition, and if the condition is noticeable, and especially worsening, you need to contact an endocrinologist on the same, or, in extreme cases, the next day for timely help. Then such a dangerous condition can be avoided.
The cause of the development of primary hypothyroidism is direct damage to the thyroid gland due to congenital anomalies, inflammatory processes (with chronic infections) or an autoimmune nature, damage to the thyroid gland after the administration of radioactive iodine, surgery on the thyroid gland, due to a lack of iodine entering the body. The causes of secondary hypothyroidism are infectious, tumor or traumatic lesions of the hypothalamic-pituitary system. An overdose of the drug Mercazolil can lead to the functional form of primary hypothyroidism.
Peripheral hypothyroidism may be associated with disturbances in the peripheral metabolism of thyroid hormones or with a decrease in the sensitivity of organs and tissues to thyroid hormones. Hypothyroidism can also occur due to congenital underdevelopment or absence of the thyroid gland. This disease is also considered as a postoperative complication, since during operations on the thyroid gland, especially if they were performed by unskilled surgeons, several months after the removal of a certain part of the organ, a certain percentage of those operated on develop hypothyroidism, which becomes lifelong.
Often the development of hypothyroidism is facilitated by diseases of internal organs and living in a region with a predominantly cold climate. Since the main function of the thyroid gland is the regulation of energy metabolism in various cells and organs, also called calorigenic (this is the side of metabolism that refers to the area of kilocalories received by the body from food products and its own reserves, and used by organ cells in the process of life), then In diseases of internal organs and conditions with energy deficiency, the need for thyroid hormones increases.
But endocrinologists, including great ones, admit that in many cases the cause of the development of hypothyroidism cannot be established. Sometimes low thyroid function is caused by a disorder of the central nervous system, such as encephalitis (inflammation of the brain). In rare cases, hypofunction of this endocrine organ develops due to a decrease in the hormonal activity of the pituitary gland (which is possible in the postpartum period in women) due to insufficient production of thyroid-stimulating hormone (TSH). There are known cases of the disease developing during menopause and after childbirth (in this case, there is often a simultaneous decrease in the functions of other endocrine glands - the adrenal and reproductive glands).
Diagnostics
Hypothyroidism is determined laboratory by a decrease in the hormonal-forming function of the thyroid gland, or rather, by a decrease in all biochemical indicators: the level of protein-bound iodine (BPI), butanol-extractable iodine (BEI), T4, T3. In this case, the thyroid-stimulating function of the pituitary gland turns out to be increased, which is laboratory confirmed by determining the content of thyroid-stimulating hormone (TSH) in the blood. This is understandable if we remember that the pituitary gland and thyroid gland work on the principle of feedback: the endocrine gland secretes few hormones - they are released more by the pituitary gland, which stimulates the reduced function of one or another organ. And vice versa. The same applies to hypothalamic releasing factors (peptide hormones of the hypothalamus).
Radioisotope research determines the reduced uptake ability of endocrine cells of the thyroid gland.
Usually, with hypothyroidism, the thyroid gland cannot be palpated, but it can be enlarged, which is observed with sporadic or endemic goiter, and also (and in recent years this has been very common) with autoimmune thyroiditis.
Hypothyroidism has a huge number of signs, this is taken advantage of by lazy doctors who, with any patient complaint, be it bleeding gums or pain in the joints, refer him to an endocrinologist. But don't panic. If you are angry for no apparent reason and throw yourself at the first person you come across, or, on the contrary, your favorite comedy plunges you into depression, and a won luxury tour to the Canary Islands makes you despondent, this does not mean at all that you have hypothyroidism. This only means that you need to see a good doctor, take a blood test for hormones, not paying attention to its high cost (and it is often carried out for a fee, although it is included in the program of state guarantees of medical care), and then carefully follow the doctor’s recommendations, without fear of the phrase “hormone therapy”. It's really only for the good. If the tests turn out to be normal, you just need to see a psychotherapist or continue to ruin the lives of those around you with your bad character. But a visit to an endocrinologist is mandatory, because hypothyroidism is not as dangerous as its complications.
Treatment
About forty years ago there were no effective drugs for the treatment of thyroid diseases, including hypothyroidism, and as a result it acquired a severe, lifelong course. Such forms of hypothyroidism were previously called myxedema. In advanced cases, especially when the disease began during the fetal development of the child or in the first months and years of his life, myxedema turned into cretinism or even idiocy, which, fortunately, practically never occurs now. Today, various types of thyroid disorders are promptly diagnosed and promptly corrected with the help of drug therapy.
The main thing in drug treatment is the prescription of replacement (hormonal) therapy. Each patient needs to select the optimal dose of one or another thyroid drug (L-thyroxine, T-reocomb, thyroidome or their analogues). Treatment begins with minimal doses to protect the heart). At the same time, the older the patient, the lower doses of medication they begin treatment with - from 1/6, 1/4 tablets. As the patient's condition improves and the drug is well tolerated, the dose of the hormone is increased, adding 1/4 tablet to the previous one every 3-4 weeks. Typically, the daily dose of thyroid medication is 1 - 1.5 tablets. The main principle of hormone treatment is to prescribe the maximum tolerated dose. Only this makes it possible to achieve a compensated course of the disease, which after a few months allows many patients to feel practically healthy. Contrary to popular belief, you cannot gain weight from hormonal medications used to treat hypothyroidism. These drugs improve metabolism. On the contrary, some take them without indications in order NOT to gain weight, and this, of course, is in vain, because in this way you can disrupt your metabolism and thereby greatly harm your body.
With timely, ongoing replacement therapy, patients remain able to work. During therapy with thyroid drugs, even the tendency to hypotension, as a rule, decreases or disappears altogether.
There is operational (surgical) hypothyroidism, which is caused by the removal of a critical part of the thyroid gland, which surgically provokes a load on the organ and a subsequent lack of hormones. In case of surgical hypothyroidism, constant (lifelong) use of drugs containing hormones is necessary.
Iodine deficiency hypothyroidism occurs due to insufficient intake of iodine in the body, which does not allow the normally functioning thyroid gland to produce the required amount of hormones, since the chemical formula of hormones (T3 and T4) includes iodine. The main direction in the treatment of iodine deficiency hypothyroidism is the introduction of the necessary iodine.
When anemia develops, patients are prescribed easily digestible iron supplements and vitamin B12 (an anti-anemic vitamin).
Lifestyle
You should adhere to a balanced diet intended for patients with hypothyroidism. Food should be easily digestible, enriched with vitamins B, A and especially C, as well as micro- and macroelements, which can improve the function of the thyroid gland (if, of course, it has reserves). In addition, such nutrition can restore impaired metabolic processes. In case of obesity (in patients with hypothyroidism it often happens, because nutrients are difficult to process completely due to a decrease in metabolic processes), the calorie content of the daily diet should be limited to animal fats and easily digestible carbohydrates, which are contained in sweet and flour products.
© Dr. Peter
Complications
The main danger of a long-term course of severe myxedema in the absence of treatment is the onset of myxedema coma. At risk are elderly patients and people with a weakened immune system due to acute infections, hypothermia, long-term hypothyroidism and chronic diseases. The list of symptoms of coma includes a drop in body temperature, intestinal obstruction, slowing of the pulse and breathing, heart failure, confusion. The probability of death for patients in this condition reaches 80%.
Treatment of mucous edema
Treatment of myxedema is based on hormone replacement therapy and is selected individually in each specific case. Additionally, a diet may be prescribed. Usually the patient feels relief within 2-3 weeks after starting medication.
It is possible to draw conclusions about the effectiveness of treatment and choose a further strategy only after several months of taking hormonal medications. Many years or lifelong treatment is often required, but such measures are well tolerated by most patients and do not cause side effects.
Diagnostics
A specialist can make a primary diagnosis already at the stage of collecting an anamnesis. Warning factors are the patient's drowsiness, decreased performance, headaches, noticeable dry skin, shortness of breath, and impaired nasal breathing. The following measures for diagnosing myxedema can confirm the endocrinologist’s assumptions:
- General and biochemical blood test to clarify the content of proteins, cholesterol and iodine in the body, hemoglobin level and ESR.
- Hormonal blood test to determine the content of thyroxine and triiodothyronine. When hormone levels increase, experts talk about the primary form of the disease; when hormone levels decrease, they speak about secondary hypothyroidism.
- Scintigraphy of the thyroid gland, which allows you to determine the activity of glandular tissues. When the absorption of radioactive iodine decreases, the thyroid gland produces less hormones, and nodules form in its structure.
- Ultrasound of the thyroid gland to exclude malignant formations in its structure, calcifications and nodes. With hypothyroidism, there is often a decrease in the volume of the organ relative to its normal size.
Diagnostics and clinical research
Diagnosis of myxedema (as well as any other forms of hypothyroidism) is carried out by an endocrinologist. The conclusion is made based on an examination of the patient, a study of the medical history and the results of clinical studies.
A laboratory blood test helps determine the levels of TSH, thyroxine (T4) and triiodothyronine (T3). In addition, persistently elevated cholesterol levels may indicate mucosal edema.
With myxedema, the uptake of radioactive iodine by the thyroid gland and general metabolism are also reduced. In some cases, hypochromic or B12-deficiency anemia occurs.
A course of treatment
The most effective treatment for myxedema is complex treatment, which includes:
- Hormone replacement therapy, thanks to which it is possible to compensate for the lack of thyroid hormones in the body.
- A diet based on foods high in iodine. Salt and animal fats are kept to a minimum.
- Symptomatic treatment aimed at reducing swelling. The patient is prescribed diuretics, diuretic herbs, and wearing compression garments. They can eliminate disturbances in the functioning of the heart, and nootropic substances are used to stabilize the functioning of the nervous system.
- Glucocorticoid anti-inflammatory drugs that simultaneously suppress the negative effects of antibodies on the thyroid gland.
Strict adherence to the doctor’s prescriptions guarantees the preservation of the patient’s stable condition and high quality of life. For the congenital form of the disease, the prognosis depends on concomitant factors, measures taken to prevent myxedema and the severity of hormone deficiency.
Treatment of myxedema
Treatment of myxedema consists of correcting hormonal deficiency by supplying thyroid hormones from the outside. The dosage is calculated individually; the drug containing hormones is taken once a day.
If iodine deficiency is established, iodine preparations and a diet rich in iodine-containing foods (seaweed, sea fish and other seafood, walnuts, iodized salt) are prescribed.
Lost thyroid function is not restored, so treatment for myxedema must be lifelong.
Diagnosis and treatment of myxedema at the clinic of JSC "Medicine"
The first symptoms of myxedema and disturbances in the functioning of the thyroid gland are a good reason for the observation of a specialist. The clinic of JSC "Medicine" invites for consultation and treatment those who care about their health and intend to receive recommendations for the treatment of pathology. Diagnostic activities are carried out at the clinic, which speeds up the receipt of results and allows several specialized specialists to be involved in their interpretation. Each client is guaranteed attentive attention, the development of an individual treatment plan with its timely adjustment as necessary, if the process produces lasting positive results. You can make an appointment through the clinic’s website or by calling the numbers provided.
Myxedema prognosis
The disease is characterized by a slow increase in symptoms, so if it is possible to diagnose myxedema in time and begin adequate treatment of myxedema, the disease will proceed benignly, although it will have to be treated for life. As for myxedema in childhood, the earliest possible recognition of the disease is of great importance, which is difficult in practice. With congenital myxedema, the prognosis is unfavorable; if it is early, it is possible to significantly improve the patient’s condition with hormone replacement therapy, but, as a rule, it is not possible to achieve complete elimination of the symptoms of myxedema.
What is required to examine the body for myxedema?
If you notice similar symptoms, the patient should urgently visit the office of a specialist in the field of endocrinology. The doctor will be able to identify the form of the disease and prescribe a course of certain procedures:
- General and biochemical blood sampling.
- Testing blood cells using enzyme immunoassay.
- Ultrasound diagnostics.
- Biopsy.
- Scintigraphic examination.
List of sources
- Dedov I.I., Melnichenko G.A., Fadeev V.V. Endocrinology / Textbook for students. honey. universities M.: Medicine, 2000;
- Fadeev V.V., Melnichenko G.A. Hypothyroidism / Guide for doctors. M.: RKI “Severo-press”, 2002;
- Thyroid diseases. Edited by L.I. Braverman. M.: Medicine, 2000;
- Clinical endocrinology: manual / ed. N. T. Starkova. — 3rd ed. -SPb. : Peter, 2002;
- Cattail V.M., Arki R.F. Pathophysiology of the endocrine system. / Per. from English - St. Petersburg. - M.: Nevsky Dialect - Publishing House "Binom", 2001.
General information
Hypothyroidism is not a disease, but a condition in which the human body has very low levels thyroid hormones . In this case, we are talking about insufficient functions of the gland, or about the development in the body of certain pathological processes that affect hormonal metabolism. The disease is defined exclusively by the external manifestations of hypothyroidism. Its symptoms were first described back in 1873. A little later, in 1878, the definition of “ myxedema ” appeared, denoting the presence of mucous edema of the skin in severe forms of hypothyroidism. Hypothyroidism most often affects women (the disease is diagnosed in approximately 1 in 50 women and 1 in 1,000 men). In most cases, the disease is detected in adult women, and its prevalence increases with age.
Clinical picture
Generalized M. to. (syn. generalized mucinosis) develops against the background of general disorders characteristic of hypothyroidism (see) - mental retardation (mental retardation, decreased intelligence) and physical development, disorders of the cardiovascular system (bradycardia, decreased blood pressure, expansion of the boundaries of the heart, muffled tones), weakened intestinal motor function, disorders of the nervous system, decreased all types of metabolism. The skin is pale, sometimes with a yellowish tint, dry, flaky, and dense. Severe mucous swelling of the subcutaneous tissue, especially on the face, shoulders and legs. Hair is dry, thin, brittle; There is loss of eyebrows, eyelashes from the outer edges of the eyelids, as well as hair loss in the armpits and pubic area. Characterized by rashes of painless nodules and nodes of various sizes, hemispherical in shape, the color of normal skin or waxy-yellow, less often pink-red, mobile, dense, located symmetrically, randomly or grouped (in rows) on the face, neck, arms, upper chest and back ; the skin over the nodules is smooth, tense, and does not fold. A variation of this form is nodular M. k., described by D. D. Levchenkov (1910) and Dessecker (W. Doessecker, 1916), occurring without noticeable signs of delayed development of the body and disorders of the neuropsychic sphere.
Localized M. to. (syn. pretibial M. to.) is characterized by symmetrical dense swelling of the skin of the anterior surface of the legs, hard, elevated nodular formations, isolated or merging, bluish-pink or yellowish in color, the mouths of the hair follicles are expanded, the skin resembles an orange peel.
Papular (nodular) M. k. (syn.: papular mucinosis, M. k. papular-lichenoid, lichen myxedematous, scleromyxedema) is characterized by symmetrical rashes, localized mainly on the skin of the extensor surface of the arms, less often on the body in the form of numerous small, shiny waxy flat, slightly raised nodules against a background of dense swelling of the skin.
Follicular mucinosis of the skin is characterized by the appearance on the skin of the scalp, face, and trunk of pasty plaques of a pale pink color, leaving behind skin atrophy.
How to detect myxedema?
According to established standards, the presented disease manifests itself in the following symptoms:
- The occurrence of edema in the facial and oral area, on the eyelids, upper and lower extremities.
- The presence of pain in the muscles.
- General weakness and lethargy.
- Drowsiness.
- The skin becomes dry.
- Hair loss.
- Difficulties in conducting a conversation.
- Decreased audibility.
- Memory problems.
- Hoarseness.
- The appearance of constipation.
- Pain in the head and so on.