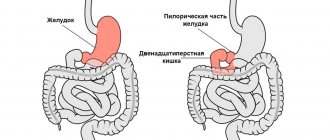
Bronchiolitis is a dangerous disease that affects the human respiratory system. Bronchiolitis provokes inflammation in the bronchioles, blocking the passage through these organs. Bronchioles differ from bronchi in that they do not have cartilaginous plates and their size does not exceed 2 mm. Unfortunately, this disease most often occurs in newborns under one year of age. Cases of the disease in adults are quite rare. The most dangerous is acute bronchiolitis in a child under 2 years of age.
Main types of disease
The types of bronchiolitis vary depending on the category of the pathogen:
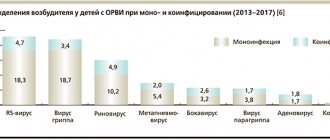
1. Respiratory type - most often appears in people who smoke, under 35 years of age and with a long history of smoking; 2. Medicinal type - may occur due to taking medications that contain cephalosporins, interferon, amiodarone; 3. Idiopathic - this type of disease can develop together with other diseases (pneumonia, colitis, lymphoma), or separately (cryptogenic variety); 4. Post-infectious - begins to develop due to an RS-type virus that penetrates the human body; 5. Obliterative - this type of bronchiolitis is caused by herpes viruses, HIV or pneumocystis
In newborn children, this disease can develop due to poor quality care or lack of normal living conditions.
Treatment of bronchiolitis in children
Most children, once diagnosed and a treatment plan developed, recover within a few days at home. Treatment of acute bronchiolitis in children at home includes:
- Taking bronchodilators. The dosage regimen and dosage are prescribed by the doctor.
- Using saline drops. If necessary, it is recommended to remove nasal mucus from the baby using an aspirator.
- Drink plenty of fluids.
- Indoor air humidificationSource: Baranov A.A., Namazova-Baranova L.S., Tatochenko V.K., Davydova I.V., Bakradze M.D., Kulichenko T.V., Vishneva I.V., Selimzyanova L.R., Polyakova A.S., Artyomova I.V. Modern approaches to the management of children with acute bronchiolitis. Pediatric Pharmacology, 2021, pp. 339-348.
However, if a child has difficulty breathing, bluish skin, dehydration and other complications, his hospitalization is required. A child can be placed in a hospital earlier if he has diseases of the lungs, heart, or immune system, since the risk of developing a severe form of the pathology is much higher.
Inpatient treatment includes:
- 24-hour monitoring of blood oxygen levels and timely oxygen therapy through a face mask, oxygen tent, and ventilator.
- Control of body hydration. If the baby does not drink enough fluid, it is administered intravenously.
- Taking bronchodilators, corticosteroids.
- Taking medications to reduce and alleviate the symptoms of the disease Source: Sukhorukova D.N., Kuznetsova T.A. Treatment of acute bronchiolitis in children in a pediatric setting Russian Pediatric Journal 20(6) 2021, pp. 329-333.
Symptoms and diagnosis
The first signs of the development of bronchiolitis are symptoms of ARVI (cough, runny nose, pharyngitis), which are combined with manifestations of bronchial obstruction.
Patients experience a characteristic “whistle” when inhaling, as well as dry or wet wheezing. As the disease progresses, severe symptoms begin to appear - pain in the chest area, shortness of breath, fever. The specialist begins to carry out diagnostics using an image of the lungs, which is taken using an X-ray or computed tomography. To establish the correct diagnosis, an arterial blood test is performed, as well as a cytogram of bronchoalveolar lavage.
Acute bronchiolitis against the background of exacerbation of chronic bronchitis. Clinical case
All recommendations were followed in full, but against the backdrop of smog in Moscow, the patient’s well-being worsened. On August 12, shortness of breath and weakness intensified, a short-term cessation of breathing occurred with loss of consciousness and a drop in blood pressure to 60/30. Resuscitated by her daughter. An ambulance team was called; there were no signs of acute coronary syndrome on the ECG. The patient was offered hospitalization in a hospital, which she refused. She continued treatment with the prescribed medications, but did not notice any improvement in her health. On August 19, I went to see a pulmonologist.
Upon examination on August 19, the patient’s condition was serious, tachypnea - respiratory rate - 32 per minute, body temperature - 36.8 C, pale skin. When percussing over the lungs, there is a boxed percussion sound, shortening of the percussion sound in the lower parts of the right lung. Auscultation of the lungs revealed harsh breathing, moist medium- and fine-bubble rales were heard in the middle-lower sections of the chest, more on the right. Heart sounds are rhythmic, muffled, heart rate is 76 per minute, blood pressure is 140/90.
The patient underwent a chest x-ray according to cito. On plain radiographs of the chest organs in direct and right lateral projections, the right pulmonary field is slightly reduced in volume and its transparency is reduced. There is an increase and deformation of the pulmonary pattern in the middle and lower lobes of the right lung and the presence of focal-like shadows with unclear outlines. Both roots are moderately expanded, the right one is displaced downward. On the left, isolated focal-like shadows are also visible above the diaphragm. CT scan of the lungs is recommended (differential range: pneumonia; hypoventilation of the right lung; pulmonary embolism (PE)
Due to progressive shortness of breath, changes in radiographs of the lungs, and the lack of positive dynamics from the therapy, the patient was urgently hospitalized at the Central Clinical Hospital No. 1 of JSC Russian Railways with a diagnosis of right-sided pneumonia against the background of exacerbation of chronic bronchitis. DN-3. Arterial hypertension. TELA?
During examination in the emergency department of the hospital, due to severe respiratory failure (blood saturation on admission 90%) and suspected pulmonary embolism, she was hospitalized in the intensive care unit (Oi).
Upon admission to Oy in the blood: Hb – 123, leukocytes – 11000, ESR – 47 mm/hour, CRP – 23.3 (normal up to 5.0), pCO2-35.4, pO2-86.7.
On ECHO-CG: the size of the heart cavities is not enlarged, moderate pulmonary hypertension, moderate concentric hypertrophy of the left ventricular (LV) myocardium, a small amount of fluid in the pericardium, the pumping function of the LV is not reduced.
ECG: sinus rhythm, heart rate - 84, moderate disturbances of the LV myocardium.
CT scan of the lungs from August 18, 2010: no infiltrative changes in the lung tissue were detected, no additional space-occupying formations were identified, the walls of the bronchi were thickened, signs of acute bronchiolitis in the lower lobe of the right lung.
As a result of the examination, the diagnosis of pulmonary embolism was not confirmed.
In Oi, treatment was carried out: resuscitation aid, oxygen therapy on site 3-5 l/min, fortum -1.0 x 3 times IV, aminophylline IV drip, prednisolone with 60 mg/day. After relief of the symptoms of acute respiratory failure and stabilization of her condition, the patient was transferred to the pulmonology department, where she continued antibacterial therapy, oxygen therapy, treatment with prednisolone - with a dose reduction until complete cancellation, Concor, Eutirox, Fluimucil, Erespal, inhalations with Berodual and Pulmicort were prescribed through nebulizer, performed by FTL.
As a result of the treatment, the patient’s well-being improved significantly, breathing was restored, but weakness and coughing persisted. She was discharged under the supervision of a pulmonologist with an open FN with a diagnosis of exacerbation of chronic bronchitis, acute bronchiolitis, DN-3 upon admission, DN-1 upon discharge. It is recommended to take erespal 160 mg per day for 4 months.
Upon discharge from the hospital in OA blood: Hb – 143, leukocytes – 7600, ESR – 22 mm/hour, blood saturation – 98%, CRP – 5.0.
From September 7 to September 17 she was in outpatient follow-up treatment. In October, the patient was vaccinated with an influenza vaccine and tolerated it well, without complications. The entire observation period felt satisfactory, there were no relapses of the disease, and she did not suffer respiratory viral infections. A control CT scan of the lungs dated March 17, 2011: a lesion in S5 of the right lung, most likely of a post-inflammatory nature, signs of chronic bronchitis. During the control study of FVD on March 22, 2011: the ventilation function of the lungs was normal, FEV1 was 84% of the required values.
Conclusions:
There is a case of long-term disability with exacerbation of chronic bronchitis, complicated by bronchiolitis with severe broncho-obstructive syndrome against the background of a previous respiratory viral infection. In a clinic setting, such diseases have certain difficulties in diagnosis, because acute respiratory and vascular failure with the development of collapse and loss of consciousness can be a manifestation of pulmonary embolism. In addition, the clinical manifestations and radiological picture of bronchiolitis are nonspecific. In all cases, when an exacerbation of chronic bronchitis with symptoms of bronchial obstruction cannot be corrected with antibacterial and bronchodilator drugs and manifestations of respiratory failure increase, it is necessary to urgently hospitalize the patient in a hospital.
In recent years, cases of protracted exacerbations of chronic nonspecific pulmonary diseases (CNLD) with various complications have been more frequently identified. This is most likely due to an increase in the number of mixed infections, the presence of a large number of stressful situations, the ecological state of the environment, and in 2010 this situation was aggravated by smog.
It has been established that the immune system of the respiratory organs is one of the most active, therefore, exposure to environmentally unfavorable factors contributes to the development of secondary immunosuppression and a significant increase in the degree of sensitization to industrial allergens.
In this regard, it is necessary to carry out measures for the early identification of patients with COPD, take them for clinical observation, and carry out immunomodulatory therapy with bacterial lysates, which stimulates the body’s natural defense mechanisms against respiratory tract infections. Of great importance is preventive vaccination with the influenza vaccine and vaccination with the polysaccharide polyvalent pneumococcal vaccine Pneumo 23, which reduce the frequency and severity of infectious diseases of the respiratory system and reduce the number of their complications.
Bibliography:
1. Interstitial lung diseases: a practical guide edited by N.A. Mukhina 2007
2. Handbook of Pulmonology, edited by Academician of the Russian Academy of Medical Sciences A.G. Chuchalina, prof. MM. Ilkovich 2009
3. Journal “Health” 11-2008, article “Medical, social and psychological aspects of the population’s incidence of chronic bronchitis in modern conditions”
Causes of acute bronchitis
The cause of acute bronchitis in adults in the vast majority of cases is an infection: most often viral, less often bacterial, and occasionally fungal. In addition, the disease can be of an allergic nature (due to a high concentration of allergen in the air), develop in the presence of inflammation of the adenoids or chronic foci of infection in the paranasal sinuses, against the background of tonsillitis.
It is worth considering factors that reduce local immunity and contribute to the occurrence of the disease:
- hypothermia;
- smoking;
- alcohol abuse;
- hereditary diseases;
- chronic pathology of the nasopharynx;
- unfavorable climate (dampness, cold);
- air polluted with dust or toxic impurities.
Causes and pathogenesis
Doctors consider the following to be the main causes of the disease:
- Complex heart and lung or bone marrow transplant.
- Various types of viral infections.
- Infection caused by mycoplasmas.
- Inhalation of toxic substances.
- Connective tissue collagenosis.
- Exposure to certain medications.
- Inflammatory and pathogenic phenomena in the intestines.
- Previous exposure to radiation, including radiation treatment.
- IgA nephropathy.
- Steven-Johnson syndrome is exudative erythema multiforme, which is characterized by a very severe course.
The forms of the disease that develop as a complication of lung transplantation are best described in modern medicine. If a diagnosis of bronchiolitis obliterans is made, the cause, in most cases, is known. Otherwise, we are talking about the idiopathic nature of the disease. With this disease, inflammation occurs inside the bronchioles, and later this can lead to fibrosis.
The most important pathogenetic factors include:
- Excessive production of cytokines, the most important of which are interferon gamma, as well as interleukin 1-0. In the case of bronchiolitis obliterans, the gene expression of these intercellular mediators increases. Interleukin 1-beta is responsible for normalizing the growth, differentiation of lymphocytes and their ability to cause pathological changes in cells. Interferon gamma induces the expression of HLA class II antigens on bronchiole epithelial cells and also controls the production of immunoglobulins.
- Increased expression of class II HLA system antigens on bronchiole epithelial cells. This is important mostly in such forms of the disease as autoimmune or drug-induced post-transplantation.
- Strengthening T-lymphocytes that cause cell pathology.
- Increased activity of PDGF, which enhances fibroblast proliferation.
- Enhanced production and release of fibronectin by bronchiole epithelial cells, a chemoagent for fibroblasts.
- Enhanced activity of transmembrane heterodimeric cellular receptors that engage fibroblasts, endothelial cells with fibronectin and fibrinogen. Cell adhesion with fibronectin is impossible without the presence of alpha-5-beta-1-integrin, and with fibrinogen - without the assistance of alpha-5-beta-3-integrin. These phenomena enhance the formation of fibroids in the bronchioles.
The most important symptoms of pathological changes
- Different densities of phlogistic bronchiolar and peribronchiolar tissue areas with cellular elements not characteristic of them.
- Increased dilation of bronchioles with secretion stasis, increased number of macrophages, mucus plugs.
- Fragmentary or total blockage of bronchioles by an increasing amount of connective tissue.
Obliterating bronchiolitis, in some cases, leads to pathology of the terminal bronchioles. In this case, the inflammation does not spread to the respiratory bronchioles, alveolar ducts, alveolar sacs, or the alveoli themselves. In addition to MDP, during the disease, large bronchi become inflamed, where cylindrical bronchiolectasis, mucus plugs, purulent exudate, and chronic inflammatory infiltrate are often found.
If post-transplant bronchiolitis obliterans is diagnosed, then it is characterized by pulmonary vascular pathology.
Advantages of treatment at SM-Clinic
Our clinics provide treatment for bronchiolitis and other pulmonary pathologies in children of any age. Therapy in our medical centers has a number of important advantages:
- the child is treated by qualified pulmonologists, doctors of the highest category with scientific titles, whose experience is at least 5 years;
- The clinic’s staff includes experienced pediatric doctors of all specialties, who, if necessary, are involved in the treatment process;
- the examination is carried out on the basis of a modern diagnostic center, which is equipped with modern high-precision equipment of the European standard;
- The clinic’s inpatient facility provides the most comfortable conditions for effective therapy under the round-the-clock supervision of doctors and medical staff.
At SM-Clinic you don’t have to wait your turn in the corridors. All consultations and examinations take place at a clearly designated time by appointment. To make an appointment with a pulmonologist, call us by phone or fill out the feedback form.
Sources:
- Delyagin V.M. Acute bronchiolitis in children. Medical Council No. 1 2013, pp. 64-68
- Boytsova E.V., Ovsyannikov D.Yu. Post-infectious obliterating bronchiolitis in children. Children's infections No. 2 2014, pp. 24-28
- Sterkhova E.V., Simanova T.V., Tyulkina R.R. Chronic obliterating bronchiolitis in children. Russian Bulletin of Perinatology and Pediatrics 62:(4), 2021, p. 211
- Sukhorukova D.N., Kuznetsova T.A. Epidemiology of acute bronchitis and bronchiolitis in children. Eurasian Union of Scientists2016.
- Baranov A.A., Namazova-Baranova L.S., Tatochenko V.K., Davydova I.V., Bakradze M.D., Kulichenko T.V., Vishneva I.V., Selimzyanova L.R., Polyakova A.S., Artyomova I.V. Modern approaches to the management of children with acute bronchiolitis. Pediatric Pharmacology, 2021, pp. 339-348
- Baranov A.A., Namazova-Baranova L.S., Tatochenko V.K., Davydova I.V., Bakradze M.D., Vishneva E.A., Selimzyanova L.R., Polyakova A.S. Acute bronchiolitis in children. Modern approaches to diagnosis and therapy. Pediatric Pharmacology 2015, pp. 441-446
- Sukhorukova D.N., Kuznetsova T.A. Treatment of acute bronchiolitis in children in a pediatric setting. Russian Pediatric Journal 20(6) 2021, pp. 329-333
Use of probiotics
Probiotics provide good assistance in the complex treatment of bronchiolitis. Liquid probiotics Bifidum BAG and Trilact combine the possibility of antimicrobial, antiviral and immunostimulating therapy. The preparations contain physiological bifidobacteria and lactobacilli and their metabolic products: vitamins, amino acids, lysozyme, bacteriocins. The composition of the nutrient medium of the drug Bifidum BAG is as close as possible to the composition of mother's milk (amino acids, lysozyme, vitamins). Bifidobacteria and lactobacilli strengthen the immune system, act against viruses, bacteria, fungi and help cope with various infectious diseases. The drugs have a pleasant taste and smell, and children really like them.
Treatment for bronchitis
Uncomplicated acute bronchitis does not require hospital treatment. The patient is prescribed:
- bed or semi-bed rest;
- plenty of warm drinks (herbal tea, alkaline water);
- dairy-vegetable diet;
- to give up smoking;
- maintaining high humidity in the room.
Your doctor may recommend antiviral medications, antibiotics for bacterial infections, and phlegm thinners to make coughing easier. For a dry, debilitating cough, drugs that suppress the cough reflex are used. Physiotherapeutic methods are also used: vibration massage, therapeutic and breathing exercises, inhalations, UHF, electrophoresis.