Urethritis is a disease of the genitourinary system that is diagnosed in both men and women. The disease is more often found in males due to the greater severity of symptoms. But the incidence rate is equally high among both sexes.
- What is urethritis?
- Causes of urethritis in women
- Symptoms
- Urogenital tuberculosis
- Diagnostics
- Complications
- Treatment of acute urethritis
- Diet for urethritis in women
- General recommendations for recovery
- Treatment of chronic urethritis
What is urethritis?
Symptoms of urethritis in women can be very mild, and a woman may not pay attention to them. Also, the disease often occurs in a latent form: when there is an infection in the body, but there are no signs of illness. Then the person does not even suspect about the pathology and does not seek medical help. In such cases, the prognosis is unfavorable, because lack of treatment leads to the process becoming chronic. And, it is logical that it carries certain complications and difficult therapy in the future.
Urethritis is a disease in which the walls of the urethra (urethra) become inflamed. The reasons may vary. Urethritis is widespread and is mainly associated with an inflammatory or infectious disease of the human genitourinary organs.
The female urethra is only 1-2 centimeters long, and the width is quite large. Pathogenic microbes easily enter this channel, and their ease of penetration into the bladder is noted. The outflow of urine is disrupted, even if the urethra is slightly swollen due to the pathological process taking place in it. Urethritis does not pose a threat to the patient’s life. But its symptoms worsen a person’s quality of life and negatively affect the state of the sexual sphere and reproductive function.
Doctors often discover urethritis in a woman, which develops along with cystitis. Moreover, the last named disease is a complication of the first, which happens in many cases. Therefore, it is important to treat inflammation of the urethra in a timely manner; it will not go away on its own. In cases of lack of treatment, an ascending process may begin, and this is already more difficult and expensive to cure.
How is nonspecific urethritis treated, in which there are no types of STIs?
An antibiotic is prescribed taking into account the culture results and the factors that caused inflammation of the urethra are eliminated. That is, they add therapy for urolithiasis, stop traumatic procedures on the urethra, recommend avoiding hypothermia, and so on.
Sometimes treatment of acute nonspecific urethritis is prescribed with injectable antibiotics before the culture is ready, if the symptoms are severe. Further, when obtaining data from a bacteriological study, the drug may change or remain the same. The dosage and duration of the course may also change.
Depending on the type of urethritis, control tests are carried out after treatment after 7–10 days, and for some STIs after 14–21 days.
Acute urethritis, treated correctly and on time, almost always ends with the patient’s recovery. If the treatment was prescribed inadequately, incompletely, or the patient self-medicated, the development of chronic urethritis in men is possible, which takes a long time to treat, is difficult and it is not always possible to completely get rid of this disease.
Causes of urethritis in women
The cause is infection. But sometimes the urethra is damaged by non-infectious agents. Therefore, the disease is divided into two types:
- infectious
- non-infectious (can be non-specific and specific)
Specific urethritis is a common inflammation with the discharge of pus. Symptoms depend on the causative agent of the pathology. Mainly:
- staphylococci
- streptococci
- coli
This type of urethritis occurs when a woman contracts sexually transmitted diseases (STDs) through unprotected sex.
Causative agents of infectious specific inflammation of the urethra:
- Trichomonas
- gonococci
- mycoplasma
- chlamydia
- Candida mushrooms
An infectious type of urethritis in women can be triggered by viruses, in most cases these are genital warts (causing HPV) or the herpes virus.
Causes of non-infectious inflammation of the urethra:
- first sexual intercourse
- venous congestion in the pelvic vessels
- diseases of the female sphere
- allergic diseases
- entry into the urethra of foreign objects that irritate the walls of the canal
- trauma to the canal when independently inserting various objects into it, during catheterization or during cystoscopy
- urethral cancer, which also causes inflammation
- urolithiasis (small stones enter the urethra and its layer is damaged)
A woman can become infected with infectious urethritis:
- during sexual intercourse
- through blood
If barrier contraception was not used during sexual intercourse, there is a very high risk of contracting urethritis. Through the blood (hematogenous route), pathogens enter the urethra through dishes, or from the zone of chronic inflammation. Such zones can be:
- tuberculosis
- tonsillitis
- chronic sinusitis
- teeth with caries
A high risk of urethritis occurs in those women who have one or more of the following factors:
- pregnancy (immunity is reduced, so the infection takes over the body faster and easier, and the balance of hormones changes, which also contributes to the development of the disease)
- significant psycho-emotional stress, constant stress
- constant consumption of alcoholic beverages
- excessive cooling of the body
- genital injury
- diseases of the genitourinary system of various types
- chronic inflammation in the body
- violation of personal hygiene rules
- reduced immunity as a result of a deficiency of vitamins in the body, strict diets, poor nutrition, serious illnesses in the past, etc.
Preventive measures
Prevention is especially important in the presence of chronic inflammation of the genitourinary system. To avoid exacerbation or re-infection, follow these recommendations:
- observe the rules of personal hygiene, especially in intimate areas;
- avoid casual sex; as a last resort, be sure to use barrier protection;
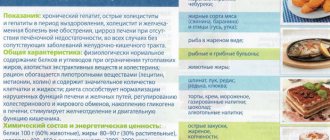
- balance your diet - exclude pickles, marinades, limit the amount of fried and smoked foods, spices, sweets; eat more alkaline foods - milk and its derivatives, fresh vegetables, nuts;
- give up bad habits - alcohol, smoking;
- take vitamin and mineral supplements in courses several times a year, drink herbal teas (consultation with a doctor is required!);
- try not to overcool the body; carry out hardening under the guidance of experienced specialists;
- avoid frequent physical and emotional stress;
- drink more clean still water;
- move more often; If you have a sedentary job, practice physical exercise or evening fitness - this will prevent congestion in the pelvic organs.
And, most importantly, treat any infectious processes of the genitourinary area in a timely manner and until complete recovery!
Symptoms
Only in rare cases does the disease make itself known with clear symptoms. In women, they are mainly manifested dimly, as noted above. The incubation period can last from minutes to 1-2 months. After this, there may be no noticeable symptoms, which occurs in 50% of cases of urethritis in women. Although the disease is latent, at this time a woman can infect her sexual partners.
Symptoms of specific and nonspecific types are different. But all types of urethritis have a common clinical picture:
- feeling that the duct is stuck together when you go to the toilet in the morning
- presence of blood in urine
- discharge from the urethra, including purulent ones
- occasional aching pain in the pubic area
- itching and other unpleasant sensations when urinating (squeezing or pulling, etc.)
These symptoms may not be fully noticeable. Only 1-2 of them may be present, or they will alternate. With urethritis there is no typical infectious clinical picture. The person does not feel weak, his body temperature can remain within normal limits.
Symptoms of urethritis in women, which occurs in a chronic form, are most often absent. But from time to time, under the influence of various factors, the disease can worsen, and then disturbing symptoms are likely to occur. The specific infectious type of disease manifests itself in different ways, which depends on the pathogen (to a certain extent helps the doctor in diagnosing the agent).
Gonorrheal urethritis
In the acute phase, a woman experiences pain and pain when she goes to the toilet “little by little.” The incubation period for this type of urethritis is 2-4 weeks. If you do not empty your bladder for a long time, then discomfort and pain appear in the urethra. This indicates specifically gonorrheal urethritis.
If you find these symptoms in yourself, immediately go to the doctor. It is at this stage that it is easiest to diagnose the disease and find the causative agent. After all, in the chronic phase it will seem to you that everything has passed, and there is no reason to see a doctor. And the process will actually progress.
Trichomonas urethritis
The incubation period is approximately the same as that of the type of urethritis described above. In 1/3 of cases there is no specific clinical picture. A typical symptom is burning and pain in the urethra and external genitalia. In the chronic form, symptoms disappear.
Candidal urethritis
Here the incubation period is shorter, ranging from only 10 to 20 days in different cases. Then a burning sensation, pain and other unpleasant sensations appear when going to the toilet to empty the bladder. There is also discharge from the urethra, which is white-pink in color. They are viscous in consistency, sometimes thick. Symptoms of candidal urethritis in women are moderate.
Mycoplasma urethritis
The onset of the disease is subacute, there are no severely disturbing symptoms. The disease begins with slight discomfort and mild itching when going “little by little” to the toilet. Today, this type of urethritis is found very rarely. If mycoplasmas are found in the urethra, in many cases this is normal and treatment is not required.
Chlamydia urethritis
The incubation period is two or three weeks. The symptoms are very mild. There may be slight pain or itching when urinating. Discharge from the urethra is also typical, it can be different. In some cases, the discharge is purulent.
Cystitis and sex
If you had prolonged or too intense sexual contact, then after it you may experience a frequent urge to urinate and pain during it; these symptoms do not always indicate an infection. They often arise due to the fact that the bladder, and in particular the neck and urethra, become “irritated” due to mechanical stress.
If these symptoms do not subside within 24 hours, then you should collect a urine test, an average sample, and contact a specialized doctor for cystitis (urogynecologist, gynecologist, urologist) as a matter of urgency.
Urogenital tuberculosis
A similar clinical picture occurs in women with tuberculosis. This disease affects not only the lungs. There are many types of tuberculosis, the process can even affect the urethra, kidneys or genitals. Typical symptoms are:
- increased sweating
- weakness
- low-grade fever that does not go away for a long time
Tuberculous urethritis often develops only when there is tuberculous kidney damage. In such cases, the process also affects the human bladder. In some cases, tuberculosis of the genital organs is also found.
The incidence of tuberculosis today is growing, and extrapulmonary forms are often recorded. With them, x-rays do not show the lesion, but in fact, the causative agent of the disease is actively operating in the human body.
Do not delay going to the doctor if you notice any disturbing symptoms, even mild or periodically disappearing. There are many diseases that you cannot distinguish, judging only by how you feel and the symptoms that arise. Only an experienced doctor can make the correct differential diagnosis and prescribe adequate treatment.
The first signs of cystitis after sex
Cystitis after sex has several differences from acute cystitis. First of all, symptoms of the disease occur either in the first few hours or 1-2 days after intimacy.
The first symptoms are a frequent urge to urinate, which is accompanied by pain, burning, stinging, a feeling of incomplete emptying of the bladder, urine changes color and smell, and becomes cloudy. Body temperature may rise to subfebrile levels, pain or discomfort may appear in the lower abdomen and lumbar region. Some symptoms may be less severe or not appear at all.
Make an appointment
Make an appointment with a gynecologist by calling 8(812)952-99-95 or filling out the online form - the administrator will contact you to confirm your appointment
guarantees complete confidentiality
Diagnostics
Examination reveals hyperemia (increased temperature) of the external opening of the urethra and nearby tissues. During palpation (an examination method by probing certain areas), painful sensations occur. The patient may complain of discharge from the urethra. It is important to send the woman to donate blood and urine - general examinations are carried out. Urine is also given for analysis according to Nechiporenko.
A bacteriological examination of urine is needed to identify the pathogen and the medications that can be used to destroy it (antibioticogram). A scraping is made from the urethra to examine it using the PCR method. The patient's urine is also analyzed for Mycobacterium tuberculosis.
Instrumental diagnostic methods:
- urethroscopy (possibly with biopsy sampling)
- urethrocystoscopy
- ultrasound diagnostics
Complications
As already noted, complications are very likely if urethritis is left untreated for a long time. Basically, the first thing that happens to women with untreated inflammation of the urethra is cystitis. Also, in many cases, complications include vaginitis and vulvovaginitis.
With an ascending infection, the following (more health-threatening) complications arise in women:
- endometritis
- adnexitis
- colpitis
- infertility
Treatment of acute urethritis
Therapy is carried out at home if there are no dangerous complications. It is important to adhere to the treatment regimen prescribed by the doctor, as well as exercise control (the doctor will also tell you about this). As for medications, antibiotics are prescribed, unless, of course, it is a fungal or viral infection. In such cases, the treatment will be slightly different.
It is important to choose the right antibiotic based on the patient’s test results. All pathogens have high and low sensitivity to certain antibacterial drugs.
If a nonspecific type of disease is detected, then broad-spectrum antibiotics are used (affecting most pathogens):
- sulfonamides
- cephalosporins
- fluoroquinolones
- macrolides
If urethritis is caused by the causative agent of gonorrhea, the following medications are used:
- cefacor
- rifampicin
- cefuroxime
- ceftriaxone
- oletethrine
- spectinomycin
- erythromycin
Treatment will be different in each case. That is why self-medication is strictly prohibited. If you don’t get tested, you won’t know what pathogen you have and how exactly you can “kill” it.
If the disease is caused by Trichomonas, then use any of the following drugs:
- metronidazole (trichopolum)
- iodovidone suppositories
- chlorhexidine
- ornidazole
- imorazole
- benzydamine
If symptoms of urethritis in women are caused by Candida, the doctor will prescribe medications that can kill the fungus. This:
- amphoglucamine
- clotrimazole
- natamycin
- nystatin
- levorin
Mycoplasma urethritis requires the prescription of antibacterial drugs, mainly tetracyclines. The drugs of choice are tetracycline itself and doxycycline. Urethritis caused by chlamydia in female patients is treated with tetracycline antibiotics, as well as the type described above. Other drugs that are suitable include clinafloxacin, azithromycin, clarithromycin and erythromycin.
Viral urethritis is treated with appropriate medications:
- penciclovir
- famciclovir
- ribavirin
- acyclovir
- ganciclovir
If a doctor finds urethritis in a woman, he first prescribes her antibiotics, which can destroy most of the known causative agents of the disease. They are called broad-spectrum drugs. This is important so that the process does not become chronic while the doctor and patient wait for test results, which will indicate the pathogen and its sensitivity to individual antibiotics.
Forms in which antibiotics are available to treat inflammation of the urethra:
- tablets (swallow)
- IV or IM solutions
- installations for infusing medication directly into the canal
- suppositories that are inserted into the vagina
In approximately 40 cases out of 100, treatment with one antibiotic is recommended, which in the language of doctors is called monotherapy. Also, in 40 cases out of 100, a combination of two antibacterial drugs is required. And only in a minority of cases are three or even 4 medications treated simultaneously.
Cystitis at any age
An acute attack of cystitis after sexual intercourse can occur at any age. Decades ago, when women maintained their virginity until marriage, cystitis that occurred after sexual intercourse was called the “honeymoon disease.”
At the present time, the fact is that no matter what your age, if the contact took place after a long break, the meeting was too active or sex happened with a new partner, you are not immune from the development of acute cystitis.
Treatment of chronic urethritis
Treatment should be comprehensive:
- taking vitamins and minerals
- washing the urinary canal with antiseptics
- taking antibiotics
An antibiotic is installed into the patient's urethra. If granulations are present, collargol and silver solution are installed in the urethra, as well as bougienage and cauterization of the urethra with a 10% - 20% silver nitrate solution (if there is significant narrowing).
If a chronic disease is caused by trichomonas, then it is necessary to install a 1% solution of trichomonacid into the urinary canal. The disease caused by chlamydia requires not only the use of antibiotics, but also probiotics, interferon preparations, immunomodulators, hepatoprotectors, vitamin complexes, antioxidants, and enzyme therapy.
Over the course of their lives, more than 50% of women suffer from urethritis one or more times. Therefore, you should be attentive to your health and do not postpone visits to the doctor if you notice disturbing symptoms of the genitourinary system.
Complications and consequences of postcoital cystitis
Cystitis after sex is dangerous due to its complications, like any other inflammation.
If you ignore the first signs, the disease may develop into a more severe form that is more difficult to treat. Infection from the bladder can spread higher and provoke inflammatory kidney disease - pyelonephritis. In addition, if cystitis after sex occurs every time, a woman will eventually lose the desire to have sexual intercourse due to the fear of getting cystitis again, and this in turn leads to uncertainty, stress, disagreements between partners, etc.
Recently, self-medication has become widespread, and women who already know their problem can take a course of antibiotics immediately after sexual intercourse, but regular use of such drugs can cause other, more serious problems (in particular, uncontrolled use leads to drug resistance, i.e. e. antibiotics become powerless in the fight against pathogenic microorganisms).
In addition, antibiotic treatment is contraindicated during pregnancy, and cystitis in this situation can lead to miscarriage, premature birth, and cessation of fetal development. All experts agree that cystitis requires professional and complete treatment, otherwise not only physical problems are possible, but also psychological ones, both on the part of the woman and the family as a whole.
In response to inflammation, an admixture of blood may appear in the urine - hemorrhagic cystitis, and frequent episodes of inflammation lead to a chronic process with the involvement of deeper layers of the bladder wall in the inflammatory process, partial or complete destruction of the GAG layer (glycosaminoglycan layer) - a protective or barrier layer , which prevents the adhesion of bacteria to the bladder mucosa.