Non-invasive diagnosis of prostate cancer is an extremely important task in modern medicine. Significant progress has been made in this area: a number of new markers have been developed (PSA3, prostate health index - PHI, telomerase), and the accuracy of imaging methods has increased, the main one being MRI. And yet, the cornerstone of diagnosing malignant diseases of the prostate gland is histological examination of prostate tissue. And the main method of obtaining tissue for this analysis is a prostate biopsy.
Prostate biopsies are taken with a special automatic long thin needle. Its thickness is approximately the same as the needle of a regular syringe, which is used to give injections or take blood from a vein. The difference lies in the special design: the needle consists of a cannula and a stylet, which can move relative to each other. This mechanism allows you to cut a thin “column” of prostate tissue and remove it inside the needle. This procedure is low-traumatic and easily tolerated.
If the patient has been properly prepared for the procedure, complications after prostate biopsy are extremely rare. Basically, this is a slight amount of blood in the urine after a biopsy within a few days, which goes away on its own. There may also be a small amount of blood in the semen, which is a normal consequence of damage to the prostate and seminal vesicles from the biopsy needle. This symptom also resolves spontaneously within a few days.
Why is a prostate biopsy done?
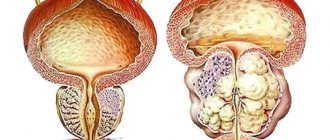
The prostate gland is an important organ of the male reproductive system, which produces a secretion that ensures the viability of sperm. Prostate cancer is the third most common cancer among men.
In the early stages of cancer, there are no obvious symptoms of pathology. Patients turn to a urologist with complaints that resemble an adenoma or inflammation of the prostate gland. The doctor performs a digital rectal examination to look for pathological nodes, lumps or swelling of the organ. The patient is referred for PSA (prostate-specific antigen), TRUS or MRI.
The results of a prostate biopsy help diagnose other diseases of the male reproductive system: fibrosis, adenosis, PIN, acute prostatitis, granulomatous inflammation.
What information does the examination of biopsy material provide?
The transcript is usually ready in 10 days.
In prostate cancer, the degree of development of tumor cells is revealed:
- If the value of the indicator is in the range of 2-4, then a low risk of tumor spread is diagnosed, because the cells differ slightly from normal;
- Values 5-7 correspond to an average risk of developing cancer;
- Values from 8 to 10 indicate a high degree of risk.
If a man's relatives have had prostate cancer, you should donate blood for PSA and consult a urologist every year, starting at the age of 45.
It is important to save the results of the examinations in order to observe changes in the PSA value, and if it increases, conduct additional studies.
Indications for prostate biopsy
The manipulation is carried out initially and repeatedly. A primary biopsy is prescribed by a urologist if there is a suspicion of cancer. Indications for the study:
- Elevated level of prostate specific antigen (PSA) in a blood test - from 4 ng/ml and above.
- A digital examination of the prostate reveals lumps, tumors or nodes.
- Ultrasound of the peripheral part identified heterogeneous, hypoechoic zones.
The urologist prescribes a repeat prostate biopsy in the following cases:
- The initial analysis showed a negative result, but the suspicion of cancer remained.
- The PSA level remains high or increases, the free antigen decreases in relation to the total.
- The primary survey material was insufficient.
During the primary and repeated procedures, biomaterial is taken from the peripheral and transitory zone of the prostate gland. This allows you to obtain the required number of biopsies (tissues) for examination.
Contraindications for biopsy
Performing a biopsy or other manipulations in the prostate gland is not always safe. If there is a risk of bleeding, severe inflammation or other pathologies, the urologist will refuse to conduct a diagnosis.
Contraindications for biopsy:
- Infections in the genitourinary system: inflammation of the urethra, pyelonephritis, acute prostatitis.
- A depressed state of the male body, which appeared due to an infectious process or others.
- Deviations in blood clotting parameters: a puncture with a biopsy gun leads to disruption of the integrity of blood vessels; if the blood does not clot well, complications will arise.
- High blood pressure that cannot be controlled with medication.
Diagnosis in case of contraindications is postponed until they are eliminated. The exception is that the threat to life due to cancer is higher than the risk of complications.
Possible complications
Typically, the consequences of prostate biopsy in men are minimal. In rare cases, infection of the urethra and trauma to the mucous membrane are possible, and even less often bleeding occurs.
You can undergo the examination quickly and painlessly at the Dr. AkNer. Modern equipment allows all stages of the intervention to be carried out under close supervision, and safe, effective anesthesia is used. Qualified and attentive doctors will help you properly prepare for diagnosis and prescribe further treatment.
Urologist, andrologist Akopyan Nerses Grigorievich.
Back to list of articles
Types of prostate biopsy
There are several methods of prostate biopsy - transrectal, saturation and fusion. Transrectal is considered the gold standard. But to accurately detect suspicious areas, an MRI of the pelvic organs with contrast is performed. Based on the results obtained, more modern and informative techniques are used. Only a few clinics in Moscow perform fusion biopsy of the prostate, which gives comprehensive results.
Transrectal prostate biopsy (TRUS) is the gold standard and a common test technique for elevated PSA levels. For diagnosis, a biopsy manipulator and thin needles with cutting edges are used. Biomaterial is collected from 12 points to obtain a complete description of the histological structure.
The procedure is performed through the rectum under local anesthesia under the control of an ultrasound scanner. This allows the urologist to accurately determine the location of the area of the prostate suspicious for tumor. After receiving the materials, the tissues are preserved in solution and sent to the laboratory for examination.
Saturation technique
Saturation prostate biopsy is an advanced research method. It is carried out to verify the diagnosis when, after a biopsy, histology shows no evidence of cancer, but PSA continues to grow. Material is collected from 24 points or more, depending on the volume of the prostate.
The method reduces the need for a repeat biopsy and does not lead to an increase in complications. Diagnostics is used for secondary research, but is also prescribed for primary testing if the patient’s age is less than 65 years, PSA is below 10 ng/ml.
Fusion
Fusion prostate biopsy is a diagnostic method that is performed using combined MRI-ultrasound control and provides a complete picture due to a three-dimensional image of the gland. The resulting images are superimposed on each other - this helps the urologist to examine the exact localization of the site where the material was taken. This is important because it becomes possible (if cancer is detected) to carry out a local treatment method: cryo and brachytherapy.
With fusion, 3-4 targeted punctures are performed in the suspicious area, taking into account MRI data. The technique is complemented by the saturation method to obtain a more accurate result.
If cancer is suspected, an MRI of the prostate with contrast is performed. If the diagnosis shows pronounced suspicious areas, a fusion technique is prescribed. The method is especially relevant when several transrectal studies have shown a negative result.
Suspicious areas are classified according to the Pirads scale:
- 2 points – low probability of cancer. If PSA levels are elevated or there are palpable masses, a repeat biopsy may be ordered.
- 3-4 points – signs of altered cells. To exclude a negative result, a saturation or fusion biopsy is performed.
- 5 points – high probability of prostate cancer.
Methods
The procedure is carried out in 3 ways.
- The method is transrectal. Taking a biopsy sample with a needle through the rectum. When the needle reaches the level of the prostate, a puncture is made in the intestinal wall adjacent to it and a biopsy is removed.
- Transurethral method. An endoscopic probe is inserted into the urethra. Having reached the prostate, having punctured the wall of the urethra, they enter the gland tissue and extract a biopsy sample.
- The method is transperineal. The biopsy sample is taken with a needle through the perineum. The procedure is performed under ultrasound guidance.
Kidney biopsy
Rules for preparing for a prostate biopsy
The accuracy of the result depends on proper preparation for the procedure, so it is recommended:
- 24 hours before the procedure, switch to easily digestible food.
- Start taking antibiotics 3-5 days in advance to prevent inflammatory processes after the biopsy.
- For 7 days, do not take blood thinning drugs that affect the blood coagulation system.
- Give up alcoholic drinks for a week.
Before performing saturation and fusion biopsies, it is necessary to consult an anesthesiologist to ensure there are no contraindications, since they are performed under spinal anesthesia.
How to prepare
- A week before the examination, it is recommended to stop taking medications that reduce blood clotting (Aspirin, Warfarin, Syncumar, etc.).
- 3 days before the examination, you must stop taking non-steroidal anti-inflammatory drugs (Ibuprofen, Diclofenac, Meloxicam, etc.) and hormones.
- On the eve of the examination, a cleansing enema is given in the evening and in the morning. The procedure is carried out on an empty stomach.
How is a prostate biopsy performed?
When performing a prostate biopsy, several people are present: a urologist, a nurse and a radiologist in the case of fusion. Before the test, a urine test is performed to look for signs of infection. If there are inflammatory processes, the examination is postponed.
During a transrectal biopsy, the area around the rectum is treated with an antiseptic. Lidocaine is injected into the intestinal wall, after which an ultrasound probe (sensor) is placed into it to obtain an image of the gland.
Thin spring-loaded needles are inserted into the prostate to obtain biomaterial. After the procedure is completed, the ultrasonic probe (sensor) is removed and the samples are sent to the laboratory.
Fusion biopsy is performed under spinal anesthesia in the lithomic position (the lower part is immobilized). An ultrasound probe is inserted into the rectum. The resulting image is synchronized online with MRI data to accurately match contours on a special biopsy grid.
The degree of pain of the procedure
During the test, the patient feels a slight prick and slight discomfort when the biopsy needle is inserted. When using the transrectal technique, pressure is felt during insertion of the ultrasound probe. The insertion of the needle may be accompanied by slight pain.
When the analysis is completed, the patient should not physically work for several hours.
The patient may feel slight pain in the pelvic area, there is often blood in the urine after the procedure, and the semen changes color. All changes usually take place within a month.
If the biopsy is taken transrectally, the rectum may bleed.
In cases where general anesthesia is used, the patient remains in the hospital for several hours after the end of the analysis, and the feeling of fatigue will be observed all day.
Biopsy analysis results
Laboratory analysis is carried out within 10-14 days, after which the patient receives a report indicating the number of tissues taken, the nature of the samples and the presence of cancer.
A negative biopsy shows no signs of changes in suspicious cells in the area examined.
The result may indicate the presence of benign changes:
- Atrophy: focal or diffuse. Occurs in men who have undergone hormonal therapy.
- Inflammation: chronic or acute prostatitis.
- Adenosis: atypical adenomatous hyperplasia.
Histological examination readings can detect cells that fall between normal and cancer. Reasons for a suspicious biopsy:
- PIN (prostatic intraepithelial neoplasia).
- Atypical proliferation of acinar cells.
- Proliferative inflammatory atrophy.
Features of the postoperative period for men
In most cases, patients tolerate the procedure well. After a transrectal biopsy, the person goes home independently (just not while driving).
Since saturation and fusion biopsies are performed under general anesthesia (spinal anesthesia), the patient remains in the clinic for a day for observation. The man is fitted with a urinary catheter, which is removed after a day - this is necessary to prevent disturbances in the outflow of urine and its normal excretion. After recovery, he is discharged.
Recommendations after biopsy
After the biopsy is completed, the doctor may insert a gauze pad containing an anesthetic gel into the rectum, which will release on its own during bowel movements. It is advisable that when traveling home there are accompanying persons who will take you by car. The next day after the procedure, you can return to your normal life and continue taking the medications prescribed earlier.
After receiving the report, it is important to contact the doctor to discuss the need for treatment depending on the results. If you experience an increase in body temperature over time or problems with spontaneous urination, you should immediately call your doctor.
The price of a prostate biopsy depends on the method chosen. Fusion is considered expensive, but it gives more accurate results without requiring repeated studies. Fusion biopsy is performed in just a few Moscow clinics by an experienced urologist using modern equipment.