Type of infection and route of infection
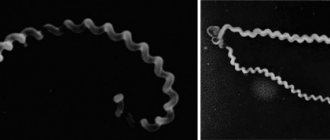
The causative agent of the disease is intestinal bacteria Enterobacteriaceae from the genus Yersinia. They are gram-negative rods up to 0.9 microns in size, growing on regular and depleted nutrient media. The most favorable temperature for them is in the range from +4 to +8 degrees, at which they are able to survive for a long time and actively reproduce on various foods. The mechanism of transmission of yersioniasis infection is close to pseudotuberculosis.
Some strains of bacteria are resistant to pasteurization, but boiling kills any of them within a few seconds. They are also sensitive to the effects of disinfectants. The peak incidence is usually observed in November and spring. People of any age are susceptible to the disease; yersiniosis is often found in children. Women are more resistant to pathogens than men.
Pathogens enter the human body through the fecal-oral or alimentary route, through a transfusion of contaminated blood, or directly under the skin through injury or injection. Transmission of intestinal yersiniosis infection can occur through contaminated foods that have not undergone heat treatment - meat, vegetables and milk, as well as water from open sources.
Symptoms of yersiniosis
The incubation period of yersiniosis pathogens lasts 1-6 days. Symptoms of yersiniosis are nonspecific. The disease is characterized by polymorphism of clinical manifestations:
- begins acutely, with the appearance of chills, headaches, weakness and malaise;
- possible pain in muscles and joints, sore throat, loss of appetite and insomnia;
- body temperature is subfebrile, can sometimes rise to 38-40 degrees;
- symptoms of general intoxication of the body are combined with signs of gastrointestinal damage - abdominal pain, nausea, diarrhea, vomiting;
- the skin becomes dry and a scaly, dotted or small-spotted rash may appear on it;
- Relative tachycardia and hypotension may occur;
- During the course of the disease, symptoms are possible that indicate damage to various internal organs - dark urine, heaviness or pain in the right hypochondrium, etc.;
- icteric staining of the sclera and skin indicates an enlarged liver; headaches may intensify over time, and focal and meningeal symptoms of central nervous system damage may appear;
- damage to the genitourinary system is accompanied by pain during urination and a decrease in daily diuresis up to complete anuria;
- as the disease progresses, pain in the abdominal area intensifies, signs of peritoneal irritation appear;
- in the second week, signs of acute arthritis may appear with damage to large joints, swelling of the face and elements of urticaria, hyperemia and pain in the eyes.
Forms of yersiniosis disease and their complications
The clinical classification of yersiniosis has not yet been fully developed. Taking into account the leading syndrome, it is customary to distinguish 2 groups of clinical forms:
- localized (gastroenterocolitic):
- generalized (icteric, septic, exanthem and arthralgic).
The clinical picture of yersiniosis of the localized form is limited primarily to damage to the gastrointestinal tract; generalized forms are accompanied by damage to other organs and systems.
- The gastroenterocolitic form of siniosis is the most common disease, accounting for almost 70% of all cases. The disease begins acutely, with an increase in temperature to 38-39 degrees, accompanied by headaches, anorexia, chills, malaise, abdominal pain and loose stools - up to 15 times a day. The duration of the disease is 2-14 days; severe forms are rare. It can occur in the form of enterocolitis, enteritis and gastroenterocolitis. In most cases, the syndrome of general intoxication is mild, abdominal pain is of low intensity, and the frequency of stools is 2-4 times per bowel movement.
- The icteric form is a complication of yersiniosis and can develop simultaneously with the gastroenterocolitic form or 2-4 days after the onset of intestinal dysfunction. Signs of liver damage come to the fore, and toxic hepatitis develops. Patients complain of pain and a feeling of heaviness in the right hypochondrium, sometimes itching of the skin appears. The disease is accompanied by yellowness of the sclera and skin, the size of the liver increases, pain appears on palpation, discoloration of feces and darkening of urine are observed. Hypertransaminasemia and hyperbilirubinemia are determined.
- The exanthema variety of the disease is manifested by exanthema and intoxication syndrome. With this form of yersiniosis, a rash appears on the skin on the 1st-6th day of illness; it can be dotted, large or small-spotted, with or without itching. After a few days, the rash usually disappears without a trace, and pityriasis-like peeling appears in its place.
- The arthralgic form occurs with intoxication, fever and severe pain in the joints, which, however, do not change externally. Arthralgia can cause immobility and insomnia.
- The septic type of the disease is quite rare and is the most dangerous, with mortality accounting for up to 30% of cases. It manifests itself as high fever with a daily range of up to 2 degrees, chills, enlarged liver and spleen. Damage to other organs is possible. The consequences of septic yersiniosis are endocarditis, nephritis with acute renal failure, pneumonia, hepatitis, meningitis, meningoencephalitis. Sometimes the result of a complication of yersiniosis is mocarditis - inflammation of the heart muscle. It is manifested by heart rhythm disturbances and tachycardia.
- The secondary focal form can occur independently or as a complication of other forms. In the second case, primary and secondary signs of the disease can be separated by a long period of well-being. Secondary manifestations are signs of damage to individual organs, causing concomitant diseases - the liver, thyroid gland (autoimmune thyroiditis), joints (arthritis), meninges (meningitis).
Complications of yersiniosis most often occur in the second or third week of the disease. Among them: exanthema (erythema nodosum, urticaria), arthritis of the joints (usually large ones), Quincke's edema, myocarditis, urethritis, appendicitis and conjunctivitis.
If you experience similar symptoms, consult your doctor
. It is easier to prevent a disease than to deal with the consequences.
Yersiniosis
Yersiniosis is an acute intestinal zoonotic infection of a bacterial nature with a fecal-oral transmission mechanism. These include intestinal yersiniosis and pseudotuberculosis (Far Eastern scarlet fever). The pathogens belong to the family Enterobacteriae of the genus Yersinia. There are two types of pathogen: Yersinia enterocolitica and Yersinia psevdotuberculosis.Etiology
The causative agents of yersiniosis belong to the family of intestinal bacteria Enterobacteriae of the genus Yersinia. There are two types of Yersinia: Yersinia enterocolitica and Yersinia psevdotuberculosis. These are gram-negative rods that grow well on regular and nutrient-depleted media. Pathogens contain O-somatic and N-flagellar antigens. Based on differences in the 0-antigen of pseudotuberculosis bacteria, 8 serological variants are distinguished (I-VIII). Diseases in humans are most often caused by serovar I, less often by III and occasionally by II, IV, V serovars. Some strains of serovars I and III are capable of producing exotoxins.
More than 50 serovars have been identified in the structure of 0-antigens of intestinal Yersinia. Most Y. enterocolitica strains of various serovars are characterized by adhesion, colonization on the surface of the intestinal epithelium, and enterotoxigenicity with the production of large amounts of heat-stable enterotoxin. Bacteria also have the ability to invade and reproduce intracellularly. The invasive and biochemical properties of pseudotuberculosis bacteria are more pronounced than those of intestinal Yersinia. Five biovars of Y. enterocolitica have been described. When cells are destroyed, both types of pathogens release endotoxin.
The optimal temperature for the reproduction of bacteria is 22-28 (C). One of the important properties of pathogens, which has epidemiological significance, is their ability to grow at low temperatures. Bacteria can multiply quickly at refrigerator temperatures (-4-8 (C). They are resistant to repeated freezing and thawing, can survive for a long time and multiply in soil, water, on various food products (vegetables, etc.). Pathogens are sensitive to drying and exposure to sunlight. When boiled, they die in 10-30 seconds. Disinfectant solutions of chloramine, hypochlorite calcium kills them within minutes.
Epidemiology
Sources of infection for yersiniosis are various types of mammals (pigs, cattle, dogs, cats), as well as birds. However, the main reservoir is synantrobic and wild rodents. A person with pseudotuberculosis does not pose an epidemiological danger. With intestinal yersiniosis, sick people or carriers can be a source of infection.
The mechanism of transmission is fecal-oral; transmission routes are mainly food, water, contact and household are possible. Transmission factors for the pathogen are usually vegetables contaminated with secretions in vegetable stores and used for preparing dishes that have not been subjected to heat treatment (cabbage salads, carrots, etc.), and dairy products. The accumulation and reproduction of the pathogen in products is facilitated by storing them in a refrigerator. The second place is occupied by the water transmission route. It is usually realized by drinking water from open reservoirs. The natural susceptibility of people to the causative agent of pseudotuberculosis is high, and intestinal yersiniosis is low. However, the manifest forms of both infections occur more often in people with a premorbid background, weakened people, and those with impaired immune status. More often, the infection is asymptomatic, causing an immune response.
Yersiniosis is widespread, but the incidence rate is higher in economically developed countries that have a centralized food supply. Most people who get sick are residents of cities and towns, where the population often uses public catering establishments. The analysis shows that the incidence of pseudotuberculosis is higher than that of intestinal yersiniosis, and children under 14 years of age are affected more often than adults. The seasonal rise in pseudotuberculosis is the spring months (March-May). However, outbreaks in summer children's health institutions shift seasonality to summer time.
With intestinal yersiniosis, the incidence is recorded more often in the cold season (October-November). Family and nosocomial outbreaks of the disease associated with infection from carriers and not seasonal are possible.
Yersinia of both species, according to the literature, along with pathogenic properties also have saprophytic properties. Based on this, diseases can be classified as saprozoonoses, and soil is an additional reservoir of bacteria.
Pathogenesis and pathomorphology
As with any intestinal infections, Yersinia enters the human body through the mouth with contaminated food or water. In the stomach, Yersinia partially die under the influence of an acidic environment. Having overcome the protective barrier of the stomach, bacteria penetrate into the mucous membrane of the ileum and become fixed in the intestinal lymphatic system, causing the development of the enteral phase of pathogenesis. Pathoanatomical changes at the site of fixation of the pathogen can be significant (such as terminal ileitis, appendicitis), sometimes the changes are weakly expressed or macroscopically absent.
Through the lymphatic vessels of the intestine, the pathogens reach the regional lymph nodes, the phase of lymphangitis and regional lymphadenitis begins, and mesadenitis develops. The appendix and cecum may be involved in the pathological process. In the lymph nodes, some microorganisms die, releasing endotoxin. Against the background of infectious and inflammatory changes, toxic and allergic processes associated with toxinemia develop. In this phase, the infectious process, acquiring the features of a localized form, can be completed.
When the lymphatic barrier breaks through, bacteremia, toxinemia and parenchymal dissemination develop with localization of the pathogen in the cells of the mononuclear phagocyte system. The liver and spleen are primarily affected; the development of polylymphadenitis, polyarthritis, osteitis, myositis, nephritis, urethritis, meningitis, etc. is possible.
All these pathogenetic factors determine the possibility of the development of generalized forms of the disease and explain the polymorphism of the clinical picture.
The pathological picture of pseudotuberculosis, described in those who died from severe forms of the disease and those who underwent surgery, indicates damage to all organs and systems. In organs rich in macrophage elements, pseudotuberculosis foci are identified - granulomas, and sometimes microabscesses; in other organs, nonspecific changes of a dystrophic nature are noted.
Pathomorphological changes in intestinal yersiniosis are accompanied by hyperemia and hyperplasia of the mesenteric lymph nodes with symptoms of abscessing reticulocytic lymphadenitis. There is compaction of the mesentery, clearly demarcated inflammation in the distal part of the small intestine with a length of 15-100 cm, sometimes there are ulcerative-necrotic changes in the mucous membrane of the appendix, as well as an inflammatory reaction of all its layers from catarrhal to phlegmonous forms.
In severe generalized forms, there is hemorrhagic edema and necrosis of the mucous membrane of the ileum, enlarged, hyperemic lymph nodes in the mesentery, and multiple small necrotic foci or abscesses in the liver and spleen.
A significant role in the pathogenesis of yersiniosis belongs to the sensitization of the body during prolonged presence of bacteria and their toxins in the blood and organs of patients. Yersiniosis in some patients can be an impetus for the formation of immunopathological reactions leading to the development of systemic diseases (such as collagenosis).
The final link in the pathogenesis of yersiniosis is the liberation of the body from the pathogen, leading to recovery. However, clinical manifestations indicate that immunity develops slowly and is not strong, resulting in exacerbations and relapses of the disease.
Pseudotuberculosis clinic
The clinical picture of pseudotuberculosis is characterized by polymorphism of symptoms and cyclical course.
The minimum incubation period is 3 days, the maximum is 18 days. The disease begins acutely. There is no prodromal period. The temperature rises to 38-40 (C. Weakness, malaise, headache, muscle and joint pain, insomnia, decreased or loss of appetite, runny nose, sore throat, sometimes sore throat when swallowing, and a slight cough appear. Symptoms of intoxication include nausea, vomiting, stool upset, moderate abdominal pain.
An objective examination reveals dry and hot skin, a puffy face, hyperemia of the face and neck (symptom of the “hood”), limited hyperemia of the hands and feet (symptoms of “gloves” and “socks”), hyperemia of the conjunctiva, injection of scleral vessels. A pale nasolabial triangle, diffuse hyperemia and swelling of the pharynx, on the mucous membrane of which there is enanthema, are often detected. The tongue is covered with a white coating. The duration of the initial period is 1-5 days.
The height of the disease is characterized by more pronounced symptoms of intoxication, signs of damage to internal organs, and persistent high fever. One of the cardinal symptoms of pseudotuberculosis is exanthema. It appears on the 1st-6th (usually 2-4th) day of illness. The rash is pinpoint, reminiscent of scarlet fever, its color ranges from pale pink to bright red. The skin background is not changed. Along with scarlatiniform elements, larger roseate or small-spotted rashes around large joints are often observed. The rash is localized symmetrically on the lateral surfaces of the body, in the axillary areas, on the skin of the lower and upper extremities, and more on the flexor surface. The rash thickens in the natural folds of the skin and around large joints. The face is usually free of rash. In severe cases, individual elements or the entire rash become hemorrhagic. The rash lasts 1-7 days and disappears without a trace.
During the peak period, patients exhibit white dermographism. The Konchalovsky-Rumpel-Leede, Moser, Pastia symptoms are positive. Hyperemia of the mucous membranes of the pharynx intensifies, and punctate enanthema is detected on the soft palate. Microlymphopolyadenitis develops. Most patients experience arthralgia, and from the 2nd week, some of them develop a picture of infectious-allergic polyarthritis. Sometimes erythema nodosum appears during this period. The height of the disease is accompanied by disturbances in the activity of various internal organs. From the cardiovascular system, tachycardia is noted, less often - relative bradycardia. Blood pressure is moderately reduced. During auscultation of the heart, muffled sounds and systolic murmur at the apex are heard.
Changes in the function of the digestive system are characterized during this period by anorexia, nausea, and vomiting. By the 5th day of illness, the tongue is cleared of plaque and becomes “crimson”. On palpation of the abdomen, pain and rumbling in the ileocecal region are noted. Sometimes enlarged and painful mesenteric lymph nodes, an enlarged liver and spleen can be palpated.
In the peripheral blood, leukocytosis of 10-30.10 9/l with band and neutrophil shift, increased ESR to 20-55, and eosinophilia are detected in a number of patients.
At the height of the clinic, a symptom complex of an infectious-toxic kidney develops: proteinuria, microhematuria, cylindruria, and sometimes leukocyturia. As intoxication decreases, renal symptoms also disappear.
In severe forms of the disease, the phenomena of meningism and sometimes symptoms of serous meningitis are determined.
The peak period lasts 5-7 days. In a third of patients, the course of the disease is complicated by exacerbations and relapses (usually single, less often two or three or more). Relapses and exacerbations are characterized by a repeated wave of fever and symptoms of local lesions. Abdominal pain and arthralgia develop. An allergic exanthema appears (maculopapular, urticarial, erythema nodosum type). The course of relapses is usually milder than the underlying disease.
During the period of convalescence, the temperature drops to normal, symptoms of intoxication disappear, and the functions of internal organs normalize. In most patients, in the 2-3rd week of the disease, pityriasis-like peeling of the skin of the trunk, face, neck and rough lamellar or leaf-like peeling appears on the palms and soles.
There is no single generally accepted clinical classification of pseudotuberculosis. Pathogenetically, it is proposed to distinguish localized and generalized forms of the disease.
The localized form includes gastroenteritis, enterocolitis (intestinal form), mesenteric lymphadenitis (mesadenitis), terminal ileitis, hepatitis.
The generalized form occurs as an acute febrile disease (scarlet fever-like form) or with the formation of secondary foci - septicemia (pseudotuberculous sepsis).
The most convenient for practice is the clinical classification of pseudotuberculosis with the identification of the leading symptom complex. The following clinical forms are distinguished: 1) abdominal, 2) scarlet-like (exanthema), 3) arthralgic, 4) icteric, 5) catarrhal, 6) mixed.
Erased and subclinical forms are detected, as a rule, in endemic foci of infection during examination of contact persons.
The abdominal form of pseudotuberculosis is characterized by symptoms of damage to the gastrointestinal tract (gastroenteritis, enterocolitis, gastroenterocolitis). This form is characterized by a pain syndrome with pain localized mainly in the right half of the abdomen, as well as diarrhea syndrome. The stool of most patients does not contain pathological impurities and does not exceed 5-7 times a day. Rarely, when the colon is involved in the pathological process, an admixture of mucus is found in the stool. The duration of the disease with this option does not exceed a week.
Sometimes the abdominal form of pseudotuberculosis manifests itself as acute terminal ileitis, mesadenitis, and appendicitis. In these cases, exacerbations and relapses often develop, and the disease takes on a protracted course. Often patients undergo surgery.
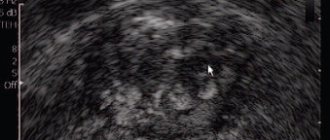
Acute terminal ileitis is manifested by symptoms of intoxication, an increase in temperature to 38-39 (C, intense, sometimes to the point of colic, pain in the ileocecal region and diarrhea. Characterized by the presence of two types of pain: cramping and in the intervals between them - a constant type. X-ray of the affected part of the ileum is determined over 10-20 cm of sharply narrowed and smoothed relief of the mucous membrane (“cord symptom”). It is assumed that this variant of pseudotuberculosis is associated with the development of chronic granulomatous-ulcerative lesions of the ileum - Crohn’s disease.
Pseudotuberculous mesadenitis is characterized by an acute onset, constant and cramping pain in the right iliac region lasting from several hours to several days. At the same time, the body temperature rises to 38 (C), nausea, vomiting, and loose stools appear up to 3-5 times a day. Subsequently, the majority experience a slow (within 3-4 days) development of peritoneal symptoms and the formation of an “infiltrate” in the ileocecal area, which is a group of enlarged mesenteric nodes. Upon examination, the following signs of mesadenitis are determined: pain on palpation of the mesentery (Sternberg's symptom), dullness of percussion sound in the iliac regions (Padalka's symptom), pain at the outer edge of the right rectus abdominis muscle 2-4 cm below the navel ( McFadden's sign).
The clinical picture of pseudotuberculous appendicitis does not differ from that of mesadenitis and is characterized by a faster rate of development of symptoms of peritoneal irritation.
All variants of the abdominal form are characterized by extra-abdominal symptoms. It is caused by a toxic-allergic syndrome (arthralgia, exanthema, injection of blood vessels of the sclera and conjunctiva, hyperemia of the soft palate, “crimson” tongue).
The arthralgic form is manifested by the development of arthralgia or polyarthritis against the background of intoxication and high fever. A rash and damage to the liver and intestines may occur, but symptoms of damage to the musculoskeletal system predominate.
The scarlet-like form is characterized by fever, a scarlet-like rash located symmetrically on the lateral surfaces of the body, in the axillary areas, on the skin of the lower and upper extremities, more on the flexor surfaces, thickening in the natural folds of the skin, as well as intoxication syndrome. Relapses are rare.
The icteric form manifests itself with clinical symptoms of reactive hepatitis. Jaundice, hyperbilirubinemia, acholia, and increased transaminases occur. Jaundice reaches a maximum at the height of the disease, then quickly fades away, biochemical parameters return to normal.
In the catarrhal form, the mucous membranes of the upper respiratory tract are predominantly affected. This is manifested by rhinitis, pharyngitis, tracheitis, bronchitis. Body temperature is low-grade, rash is rare. Diagnosis of this form is difficult.
Sometimes during the course of pseudotuberculosis infection, symptoms of two forms predominate, for example, abdominal and arthralgic, icteric and abdominal, etc. In these cases, it is customary to talk about a mixed form of pseudotuberculosis.
The generalized form is difficult. It combines high fever, severe symptoms of intoxication, exanthema and organ damage. The septic form is more often observed in people with reduced general reactivity of the body, often in the elderly, suffering from chronic liver diseases, diabetes mellitus, blood diseases, and alcoholism. The course of the septic form is long, recurrent, with the formation of multiple purulent lesions of internal organs, and it has a high mortality rate.
Based on the severity of the disease, mild, moderate and severe forms of the disease are distinguished. The severity of the course is determined by the severity of intoxication and the degree of involvement of internal organs in the pathological process.
Regardless of the form of pseudotuberculosis, the duration of the disease does not exceed 1.5 months. However, sometimes a protracted course of the disease occurs (1.5-3 months). Exacerbations of the process, repeated relapses significantly increase the duration of the disease (up to 6 months or more). Chronic diseases of the musculoskeletal system and gastrointestinal tract are described. Etiologically, they are associated with the pseudotuberculosis pathogen; they are regarded as clinical manifestations of the consequences of the disease or its residual phase.
Clinic of intestinal yersiniosis
The duration of the incubation period is shorter than with pseudotuberculosis, and is 1-6 days. Yersiniosis is characterized by polymorphism of clinical manifestations. The gastrointestinal tract is most often affected in combination with intoxication syndrome. The clinic progresses according to the type of gastroenteritis, enterocolitis, gastroenterocolitis.
The disease begins acutely: chills occur, body temperature rises to 38-39 (C, patients are worried about weakness, headache, arthralgia, myalgia, nausea, vomiting, abdominal pain of a cramping or constant nature. They are localized in the epigastrium, around the navel, in the right ileum region, sometimes in the right hypochondrium. The stool is liquid, viscous with a pungent odor. In some patients, when the colon is involved in the pathological process, an admixture of mucus is found in the stool, less often - blood. The frequency of stool is from 2-3 to 15 times a day. Duration of the disease 2-15 days Along with the benign course, there are severe forms of the disease with pronounced intoxication and dehydration of the body.
The clinical manifestations of acute terminal ileitis, mesadenitis and appendicitis do not differ significantly from the course of similar variants in pseudotuberculosis.
Along with gastrointestinal symptoms, toxicoallergic syndrome develops with yersiniosis.
On the 1st week of the disease, upon objective examination, the skin of patients is of normal color or somewhat pale. Some people develop a pinpoint or pinpoint rash on symmetrical areas of the skin of the torso and limbs. The rash disappears within a period of several hours to 3-4 days. Symptoms of “hood”, “gloves”, “socks” are not typical for intestinal yersiniosis. Conjunctival hyperemia and scleral vascular injection are often observed. The mucous membrane of the pharynx is intensely, diffusely hyperemic. Palpation reveals moderately enlarged and painful peripheral lymph nodes, lability and increased heart rate corresponding to body temperature. Blood pressure is reduced, heart sounds are muffled. With severe intoxication, a systolic murmur of functional origin is heard at the apex.
During the same period, the tongue is covered with a white coating; by the 5-7th day it clears and becomes “crimson”. Palpation of the abdomen is painful, rumbling is noted in the ileocecal region, sometimes in the epi- and mesogastrium. Positive symptoms of Padalka and Sternberg are revealed. In patients with low body weight, enlarged and painful mesenteric lymph nodes can be palpated. The liver and spleen are involved in the pathological process. They become accessible for palpation by the end of the 1st week of the disease. Damage to the liver parenchyma in a number of patients leads to the appearance of icterus in the sclera and skin, increased bilirubin in the blood, urobilin in the urine, and moderate transaminasemia.
With yersiniosis, symptoms of “infectious-toxic kidney” and serous meningitis often develop.
In the peripheral blood, leukocytosis, neutrophilia, band shift, accelerated ESR, and sometimes eosinophilia are observed.
At the 2-3rd week of the disease, symptoms appear that indicate an immunological restructuring in the body - these are urticarial, macular, maculopapular rashes, localized on the trunk and limbs, often in the area of large joints. Erythema nodosum occurs. Some patients develop infectious-allergic polyarthritis: there is an increase in temperature in the area of the affected joints, redness, swelling, and 2-4 joints are involved in the process.
During the same period of the disease, myocarditis, conjunctivitis, iridocyclitis, cystitis, urethritis, nephritis, Reiter's syndrome and other lesions of internal organs can develop.
A third of patients may develop exacerbations and relapses, which complicates the course of the disease. They are characterized by a repeated wave of fever and gastrointestinal symptoms, as well as extra-abdominal manifestations typical of the peak period.
By the end of the 3rd week, a period of convalescence begins. Body temperature drops to normal, symptoms of intoxication disappear, and the functions of internal organs are restored. Pityriasis-like peeling of the skin appears on the torso, face, neck and lamellar peeling on the palms and soles.
A clinical classification of yersiniosis has been developed. There are localized and generalized forms. Depending on the greatest severity of the pathological syndrome, gastrointestinal, abdominal (appendicular) forms, generalized (secondary focal, septic), and bacterial excretion are differentiated.
Taking into account the severity of the intoxication syndrome and the degree of involvement of internal organs in the pathological process, the severity of the course is divided into mild, moderate and severe. More often the disease occurs in a mild to moderate form.
The duration of manifest forms of yersiniosis is 1.5 months. However, a protracted course of the disease may occur (1.5-3 months) and in rare cases - more than 3-6 months (chronic). The development of chronic diseases of the gastrointestinal tract and connective tissue caused by previous intestinal yersiniosis is regarded as the clinical consequences of yersiniosis (residual phase).
In elderly people and young children with severe immunosuppression, yersiniosis can develop in a septic form with a severe course and unfavorable prognosis. The disease begins acutely. Body temperature reaches 39-40 (C. Headache, weakness, nausea, vomiting, diarrhea, adynamia appear. Fever of remitting or irregular type is accompanied by tremendous chills and sweat. Jaundice may appear. A roseolous, maculopapular or hemorrhagic rash is observed on the skin. With this form, hepatosplenomegaly is detected. Anemia, neutrophilic leukocytosis, and a significant increase in ESR are noted in the peripheral blood. The course of the disease often ends in an unfavorable outcome.
Bacterial excretion is characterized by the absence of clinical symptoms of the disease. In these individuals, Yersinia is excreted from the feces. Bacterial excretion can be either short-term (acute up to 3 months) or long-term (chronic) - more than 3 months. Bacterial excretors are actively detected during examination of employees of food enterprises and contacts in foci of infection.
The prognosis for pseudotuberculosis and intestinal yersiniosis is most often favorable. The exception is the septic form, in which the prognosis is always serious and often unfavorable.
Diagnostics
Clinical signs of the disease, a combination of abdominal, extra-abdominal, and toxicoallergic symptoms allow one to suspect a yersinia infection. Epidemiological history data are of great importance. However, specific research methods - bacteriological and serological - are decisive in establishing the final diagnosis.
The main materials for bacteriological research are blood, feces, vomit, cerebrospinal fluid, removed appendix and mesenteric lymph nodes. In case of catarrhal form, swabs from the throat can be used for bacteriological examination. The Peterson and Cook method is used, which is based on the ability of bacteria to grow at low temperatures. Serov's medium and standard buffer solution are elective. Serological diagnosis is of great importance for confirming not only the clinical diagnosis, but also the etiological role of the isolated Yersinia. RA and RNGA are used. Paired patient sera taken at the onset of the disease and at the 3rd week are examined. A titer of 1:200 is considered diagnostic in RA, and 1:160 and higher in RNGA. The most valuable is the increase in the titer of specific antibodies in the blood serum over time.
In express diagnostics, ELISA, NRIF, RCA (coagglutination reaction) can be used to detect antigen in blood, feces, urine, saliva in the first days of the disease, and antibody diagnostic kits can be used.
Histological examination of biopsy samples of lymph nodes and other organs is also of certain importance in diagnosis.
Yersiniosis often has to be differentiated from scarlet fever, intestinal infections, rheumatism, polyarthritis, viral hepatitis, infectious mononucleosis, leptospirosis, typhoparatyphoid diseases, sepsis of other etiologies, etc.
Treatment
Therapy should be comprehensive and include etiotropic, detoxification, and antihistamines.
Etiotropic drugs include antibiotics. The greatest clinical effect is provided by chloramphenicol (0.5 g 4 times a day) for 2 weeks. Tetracycline, gentamicin, streptomycin, rifampicin are also highly effective, and in severe forms and relapses - cephalosporins.
Of the sulfonamide drugs, biseptol is used. Chemotherapy drugs of the nitrofuran series are used (0.1 g 4 times a day). The duration of etiotropic therapy depends on the form of the disease and is 7-14 days, with generalized forms more than 14 days.
In case of severe intoxication, detoxification agents are used (polyionic solutions, reopolyglucin, hemodez, etc.)
In severe cases, corticosteroids are used. Taking into account the allergic component in the pathogenesis of the disease, all patients are prescribed antihistamines.
Since exacerbations and relapses can occur with yersiniosis, the use of pentoxyl, methyluracil, potassium orotate, multivitamins and immunomodulators is indicated. For severe arthralgia, nonsteroidal anti-inflammatory drugs (indomethacin, voltaren, brufen, etc.) are prescribed.
Particular attention is paid to surgical treatment. Patients with suspected appendicitis, mesadenitis, terminal ileitis, accompanied by a symptom complex of acute abdomen, should be observed by a surgeon, who will determine the indications for surgery. Before and after surgery, etiotropic and pathogenetic therapy is carried out in full.
Anti-epidemic measures
The medical institution submits an emergency notification about the identified patient to the territorial center of state sanitary and epidemiological supervision within 12 hours. If group diseases (25 people or more) occur in preschool, adolescent or medical institutions, an emergency report is sent to the State Committee for Sanitary and Epidemiological Supervision of the Russian Federation within 24 hours after receiving information from the field.
Hospitalization of the patient is carried out according to clinical indications. Convalescent drugs are prescribed no earlier than the 10th day after clinical recovery and normalization of blood and urine parameters. Workers of food and similar enterprises who have been ill are allowed to work after negative results of a three-time bacteriological examination of feces, carried out at intervals of 1-2 days.
Measures regarding pathogen transmission are aimed at identifying the food product that served as a transmission factor. If an outbreak occurs in an organized team, all employees are surveyed about the products they consumed during the past week, the menu, a tasting log of ready-made dishes, a sanitary log, personal medical records of employees are studied, and suspicious material is taken for laboratory testing (food residues, washings from equipment, etc.). d.). When diseases occur in a hospital, an examination is carried out to identify the source of the pathogen - the patient or the carrier.
Persons who have been in contact with the patient are placed under medical observation for 10 days. Thermometry, periodic examinations, and bacteriological examination of children attending groups and in families are carried out.
Those who have recovered from yersiniosis are monitored by infectious disease specialists or therapists in local clinics for 3 months. Blood and feces are examined after 1 and 3 months; in case of liver damage, biochemical parameters are examined.
Prevention
Specific immunoprophylaxis has not been developed. Preventive measures are aimed at combating the source and reservoir of infection - rodents, preventing their penetration into vegetable stores, food warehouses, shops, etc. For this purpose, deratization measures are carried out in fields, food warehouses, vegetable stores, public catering establishments and food trade. It is necessary to carry out epidemiological surveillance of water supply, technological regime of processing and storage of food products, especially those not subject to heat treatment. To prevent nosocomial diseases, it is necessary to promptly identify carriers and patients with mild forms of yersiniosis.
Vladislav LUCHSHEV, head of the department of infectious diseases, tropical medicine and epidemiology, professor. Vera VOLODINA, associate professor. Lyubov SOKOLOVA, associate professor. Russian State Medical University.
Diagnosis of yersiniosis
Diagnosis of yersiniosis is carried out on the basis of the symptoms of the onset of the disease - fever, intoxication and signs of an acute form of gastroenterocolitis in combination with jaundice, exanthema and arthralgia. The most common are enteritis, terminal ileitis, enterocolitis and mesadenitis. Less common forms are sepsis, tonsillitis and secondary foci of infection.
Enteritis and enterocolitis are the most common, they manifest themselves in inflammation of the large and small intestines, accompanied by loose, foul-smelling stools up to 10-15 times a day, sometimes with mucus and blood. The duration of diarrhea, depending on the severity of the disease, ranges from 1 day to several months. In most cases, the temperature remains low-grade - about 37.5 degrees, sometimes it can rise to 39-40 degrees.
Almost all forms of the disease are accompanied by enlarged lymph nodes. Pathogens are able to concentrate in the lymph nodes with the formation of microabscesses - purulent inflammations. To confirm the diagnosis, tests for yersiniosis are performed.
Tests for yersiniosis
Diagnosis of yersiniosis is based on bacteriological and serological research methods. The culture technique is the same as for pseudotuberculosis. For the purpose of laboratory confirmation of the diagnosis, cultures of feces, cerebrospinal fluid and blood are performed on nutrient media. From a series of serological methods, agglutination reactions, latex agglutination, indirect hemagglutination with erythrocyte diagnostics and enzyme-linked immunosorbent assay are used.
In uncomplicated forms of the disease, laboratory data are not specific. The leukocyte level is normal or slightly increased. ESR in reactive arthritis can reach 100 mm/h, but antinuclear antibodies and rheumatoid factor are usually absent. Blood, lymph node tissue, cerebrospinal fluid, peritoneal fluid, and abscess contents are subjected to standard clinical microbiology techniques.
Differential diagnosis is carried out taking into account the clinical picture of the disease. Its primary goal is to exclude acute intestinal infections, various joint diseases, viral hepatitis, acute appendicitis and sepsis of other etiologies.
When X-ray studies of the intestinal area, a sharp narrowing of the affected part of the ileum is observed, the relief of the mucous membrane is often smoothed (the so-called “cord” symptom). At the following stages, it is possible to develop a granulomatous-ulcerative lesion in the ileum, which is morphologically indistinguishable from Crohn's disease.
The presence of yersiniosis is signaled by the accelerated positive dynamics of clinical signs and morphological changes in the terminal ileum during treatment with antibacterial drugs, while glucocorticoids and mesalazine are effective in Crohn's disease.
Difficulties may arise in the differential diagnosis of hepatitis of viral etiology and yersinia hepatitis. Yersiniosis hepatitis can manifest itself both as an independent variant and in a generalized form of yersiniosis. From the first stages of the disease, an increase in the blood bilirubin content and pronounced signs of intoxication are observed, while the activity of transaminases slightly increases.
Yersiniosis: expanding traditional ideas about diagnosis, treatment and medical examination of patients
Yersiniosis is widespread in the Russian Federation, and the consistently low level of officially registered incidence does not reflect the true state of the problem. Yersiniosis has now gone beyond the scope of a purely infectious pathology, becoming a therapeutic problem due to the “weak” laboratory base used in practical healthcare, problems in choosing treatment tactics and rehabilitation of patients. Clinicians are particularly concerned about the adverse consequences of yersiniosis, in particular, the chronicity of the infectious process and the formation of systemic autoimmune diseases as a result of the disease [1].
Although in recent years the clinical manifestations of the disease, including the chronic course, have been described in sufficient detail, and significant adjustments have been made to the understanding of the links of immunopathogenesis, practicing doctors know how difficult it is to make a diagnosis, and most importantly, to select treatment for patients that is adequate to the stage of the disease.
As our experience shows, patients with yersiniosis, due to the polymorphism of clinical manifestations of different periods of the disease, are often referred not to an infectious disease specialist, but to doctors of other specialties (gastroenterologists, rheumatologists, endocrinologists, hematologists, etc.), each of whom makes a diagnosis, in fact, being syndromic, and, as a result, prescribes only symptomatic treatment. This statement is based on data from long-term monitoring of yersiniosis survivors, according to which recurrent course among hospitalized patients is recorded extremely rarely (1.3%) and does not correspond to real data on the true frequency of relapses (from 15.8% to 44% in different years).
Apparently, such a rare hospitalization of these patients is associated with the lack of long-term outpatient follow-up of patients who have had yersiniosis, as a result of which, after discharge from the hospital, they fall out of the field of view of the infectious disease specialist, and developing relapses are mistakenly interpreted by other specialists. However, it is early diagnosis and timely treatment that is given the leading role in the prevention of post-yersinia immunopathological diseases, leading to a long-term decrease in performance and disability of patients.
Diagnostic drugs and test systems widely used in practical medicine have rather low sensitivity and efficiency [2, 3]. Long-term monitoring of the diagnosis of “yersiniosis” in patients hospitalized at ICH No. 2 in Moscow has shown that over the past ten years the number of erroneous diagnoses of “yersiniosis” has been steadily increasing, which leads to unnecessary antibiotic therapy and long-term disability of patients. Thus, at the prehospital stage, 57.6% (ranges from 50.9% to 66.3% in different years) of patients are mistakenly diagnosed with yersiniosis, and the patients do not receive adequate treatment in specialized departments of general clinical hospitals.
In the infectious diseases hospital, 42% of these patients had other infectious diseases as their final diagnosis (acute intestinal infections, ARVI, enteroviral diseases, infectious mononucleosis, hemorrhagic fever with renal syndrome, viral hepatitis, generalized chlamydia, leptospirosis, HIV, brucellosis, tularemia, etc. .) and 58% had non-infectious pathology. Of particular concern is yersiniosis, which is misdiagnosed at the prehospital stage in 5.7–15.2% of patients with acute surgical pathology requiring emergency surgical intervention [4, 5].
One cannot but agree with the opinion of V. A. Orlov et al. (1991) that “most diagnostic errors are due to an incorrect approach to the diagnostic process.” Apparently, only this can explain the fact that over the course of ten years, 2.9–9.1% of patients with suspected yersiniosis are eventually diagnosed with heart and vascular diseases, and 2.8–6.4% with intestinal tumors , lungs and pelvic organs, in 2.9–7.1% - Hodgkin lymphoma, lympho- and myeloid leukemia, in 2.8–6.1% - diseases of the endocrine system (toxic goiter, thyrotoxicosis, autoimmune thyroiditis), in 2 1–12.1% - inflammatory diseases of the genital organs.
In our opinion, one of the main reasons for diagnostic errors leading to both under- and overdiagnosis of yersiniosis is the low information content of insufficiently specific techniques and diagnostic tools, as well as non-compliance with existing recommendations for the diagnosis of yersiniosis. In the Russian Federation there are modern diagnostic drugs, methods and culture media for the indication and identification of Yersinia enterocolitica and antibodies to them, but the system of their use is not unified, and the assessment of specificity is imperfect.
Laboratory diagnosis of yersiniosis should include bacteriological, immunodiagnostic and serological methods. The main method is bacteriological - seeding the patient’s biological material (feces, urine, washings from the back of the throat, blood clot, sputum, bile, cerebrospinal fluid, surgical material, etc.), material from the external environment and from animals on nutrient media to detect Y growth enterocolitica followed by culture identification. At least four materials must be tested (for example, feces, urine, blood, pharyngeal wash). The optimal time for collecting material is the first 7–10 days of illness. It is extremely rare to obtain a culture of Y. enterocolitica from material from patients with prolonged course and secondary focal forms of yersiniosis.
The main disadvantages of the bacteriological method are the low frequency of obtaining culture growth - on average in the Russian Federation, Y. enterocolitica is isolated in 2-3% of samples, 0.81%, and retrospectiveness (the final result is on the 21-28th day of production) [2]. For more than ten years, in the bacteriological laboratory of the IKB No. 2 in Moscow, it was possible to isolate Y. enterocolitica in only 0.2% of the samples taken (only in the generalized form of yersiniosis), which is consistent with the data of the GSEN center in Moscow and is four times worse, than in the Russian Federation as a whole [2, 3].
Immunodiagnostic methods make it possible to detect Y. enterocolitica antigens in clinical material up to the 10th day from the onset of the disease (enzyme-linked immunosorbent assay (ELISA), coagglutination reaction (ICA), immunofluorescence reaction (RIF), indirect immunofluorescence reaction (IRIF), agglutination and lysis reaction ( RAL)). According to manufacturers, the sensitivity of test systems reaches 104–105 m cells/ml, and the efficiency of testing coprofiltrate and serum in the first five days of illness is 83–85%. Promising methods are methods for indicating and identifying pathogenic Y. enterocolitica by a set of phenotypic characteristics associated with its pathogenicity determinants (API test systems (sensitivity 79%) and genetic methods for diagnosing and typing Yersinia (polymerase chain reaction (PCR), multiprimer PCR) .The advantages of PCR include the speed of analysis (up to 6 hours), information content, high sensitivity and specificity. However, in practical medicine, the specificity of this reaction turned out to be the most vulnerable. The immunoblotting method, which makes it possible to detect and identify proteins (antigens) of Yersinia using antisera, in RF is used unreasonably rarely.
To determine specific antibodies to Y. enterocolitica antigens, serological methods are used. The study must be carried out from the 2nd week of illness in paired sera with an interval of 10–14 days. A 2–4-fold dynamics of antibody titer in paired sera is desirable, which, however, is not always observed in practice. At the onset of the disease, the most informative reaction is ELISA with determination of IgA, IgM and IgG, ELISA; at 3–4 weeks - ELISA, ELISA, agglutination test (RA), RSC, A-BNM. For the qualitative determination of IgA and IgG class antibodies to the virulence factors of pathogenic strains of Y. enterocolitica, you can use the immunoblotting method, which is used for the differential and retrospective diagnosis of yersiniosis. In the chronic course of yersiniosis, ELISA with the determination of IgA and IgG and immunoblotting are informative.
Despite the large number of test systems offered and various companies guaranteeing a high frequency of detection of yersinia antigens or antibodies to them (up to 85%), in practical health care the indirect hemagglutination test (IRHA) and RA are more often used, which actually makes it possible to diagnose yersiniosis only in every fourth patient (25.3%): with the abdominal form - in 41.7% of patients, with the generalized form - in 21.1% of patients, with the secondary focal form - in 30.8% of patients. It is extremely rare that serological methods confirm the gastrointestinal form of yersiniosis (4.5%). There is no reliable relationship between the level of antibodies to Yersinia and the severity of yersiniosis.
Quite often (21.1% of cases), attending physicians interpret a single detection of specific antibodies to Y. enterocolitica in the blood of patients as laboratory confirmation of yersiniosis. However, in the majority of patients (54.1%), the titer does not exceed 1:200, which means it cannot be considered laboratory confirmation of the clinical diagnosis. The explanation for this lies in the intensive circulation of Yersinia in the environment and among the population. According to materials from the GSEN centers in the Russian Federation, when examining healthy individuals, specific antibodies to Y. enterocolitica are detected in 0.4–4.4% of samples [2]. However, the immune layer among the population is much higher - 18.2–19.6% [6, 7].
Antibody titers to Y. enterocolitica in the direct hemagglutination reaction (DHR) and RA above 1:200 are recorded only in 45.9% of patients. However, a one-time blood test using the mentioned methods, even with a high titer, cannot be unambiguously interpreted as yersiniosis. Thus, in our practice there was a patient with severe articular syndrome, during a dynamic blood test of which antibodies to Y. enterocolitica using the RA method were at a constant level of 1:102,400, which only indicated that she had suffered yersiniosis and was not an indication for prescribing antibacterial therapy.
Analyzing the general recommendations for laboratory diagnosis of yersiniosis and the current situation in practice, we can state that laboratory diagnosis of the disease remains at the level of the early 90s. The reasons lie not only in the use of insufficiently effective methods, but also in non-compliance with existing recommendations for diagnosing yersiniosis. Thus, in most cases, when making a diagnosis, practitioners rely on a single examination of material taken from the patient and the titer of antibodies to Y. enterocolitica. However, the serological criterion for the diagnosis of “yersiniosis” should be considered not so much the achievement of the “diagnostic” titer of specific antibodies, but rather its dynamics when studying paired sera with an interval of 10–14 days. To increase the efficiency of diagnosing yersiniosis, we recommend examining the blood serum of patients with yersiniosis using at least three methods (for example, RNGA, RSK and ELISA, etc.).
Pathogenesis of yersiniosis. The choice of management tactics and drug treatment for patients with yersiniosis directly depends on the pathogenesis of different stages of the disease. It is known that the nature of the interaction of Y. enterocolitica with the macroorganism depends on the set of pathogenicity factors of the strain, the dose of the infection, the route of administration and the immunological reactivity of the macroorganism. Taking into account the available experimental data, the pathogenesis of yersiniosis in humans can be presented as follows. Y. enterocolitica enters the human body orally, and the disease develops after a fairly short incubation period - from 15 hours to 6 days (on average 2-3 days). The bulk of Yersinia overcomes the protective barrier of the stomach. In the stomach and duodenum, catarrhal-erosive, less commonly, catarrhal-ulcerative gastroduodenitis develops. Then the development of the pathological process can go in two directions: either local inflammatory changes will occur in the intestine, or a generalized process will develop with lympho- and hematogenous dissemination of Y. enterocolitica.
If the disease is caused by serotypes of Y. enterocolitica, which have pronounced enterotoxigenicity and low invasiveness, then, as a rule, processes localized in the intestine develop, the manifestations of which will be damage to the gastrointestinal tract (catarrhal-desquamative, catarrhal-ulcerative enteritis and enterocolitis) and intoxication.
If Y. enterocolitica penetrates the mesenteric nodes, the abdominal form develops. The pathomorphology of yersinia lymphadenitis is a combination of infectious, inflammatory and immunological processes. In the appendix, the inflammatory process is often catarrhal in nature, but the development of a phlegmonous process with subsequent destruction of the appendix and the development of peritonitis is possible. Gastrointestinal and abdominal forms of yersiniosis can be either independent or one of the phases of the generalized form.
There are two known ways of generalization of the yersinia process - invasive and non-invasive. The invasive route of entry of Y. enterocolitica through the intestinal epithelium is the classic and best studied. If the infection is caused by a highly virulent strain of Y. enterocolitica, then a non-invasive route of penetration through the intestinal mucosa inside the phagocyte is possible.
During the period of convalescence, the body should be freed from yersinia and the impaired functions of organs and systems should be restored, resulting in clinical and laboratory recovery. However, such a favorable development of events is possible only with an adequate immune response and the absence of immunogenetic and epigenetic markers of an unfavorable outcome. Dispensary observation of convalescents for five years after acute yersiniosis showed that the outcomes of yersiniosis can be:
1) clinical and laboratory recovery (55.2%);
2) unfavorable outcomes (29.2%):
a) with the formation of a chronic course (57%);
b) with the formation of pathological conditions and diseases of an autoimmune nature (43%);
3) relatively unfavorable outcomes with a predominance of the infectious and inflammatory component (10.5%):
a) with exacerbation of chronic inflammatory diseases (35.5%);
b) with the formation of new diseases with a predominance of the infectious-inflammatory component (64.5%);
4) residual effects (short-term low-grade fever, periodic myalgia and arthralgia, neurological symptoms involving nerve plexuses and roots, autonomic reactions, asthenic and hypochondriacal syndromes, the phenomenon of interoception, etc.) (5.1%).
The best prognosis is for patients aged 19–25 years. Among them, 71% recover. At the same time, 45% of survivors aged 26–45 years develop pathological conditions of various origins that are included in the category of unfavorable outcomes of yersiniosis.
According to our data, doctors diagnose secondary focal forms of yersiniosis more often than they actually form. This is due to the absence of pathognomonic clinical manifestations of secondary focal forms of yersiniosis and their systemic nature. The group of patients with the so-called secondary focal form of yersiniosis is not homogeneous. This group often unreasonably includes both patients with a pathological process of yersiniosis etiology (for example, the chronic course of yersiniosis), and patients with a chronic course of post-yersiniosis infection, with emerging new acute processes of non-yersinia etiology and patients with autoimmune pathology. This state of affairs requires special attention and analysis of clinical and laboratory parameters from the practicing physician, since further treatment tactics, and therefore the outcome of the entire pathological process, depend on their understanding.
In patients with chronic yersiniosis, Y. enterocolitica continues to circulate in the body for a long time. According to our data, the chronic course of yersiniosis develops in 16.6% of patients and is more often observed in people over 25 years of age. The “shelter” of pathogens is the lymph nodes, small intestine and cells of the macrophage-monocyte series. Activation of foci of infection can clinically manifest itself in the form of urethritis, nephritis, enteritis, meningitis, etc. From the foci, Yersinia antigens enter the blood as part of immune complexes, causing reactive arthritis, damage to the kidneys, intestines, organs of vision, etc. Slowing the speed of blood flow in the tissues - targets creates favorable conditions for the deposition of Y. enterocolitica antigens. A criterion for the persistence of the pathogen can be considered long-term (more than 6 months) circulation of specific IgA to Yersinia lipopolysaccharide.
Among the diseases that are of an autoimmune nature and are the outcome of yersiniosis, seronegative spondyloarthropathy (usually reactive arthritis and Reiter's syndrome), rheumatoid arthritis, autoimmune thyroiditis and Crohn's disease predominate.
Treatment of patients with yersiniosis and pseudotuberculosis should be comprehensive, pathogenetically substantiated and carried out taking into account the clinical form and severity of the disease (
), (
). The most important task is to relieve symptoms of the acute period and prevent adverse outcomes of the disease. Hospitalization of patients with yersiniosis is carried out according to clinical and epidemiological indications. For mild and uncomplicated moderate cases, treatment at home is allowed. According to epidemiological indications, patients belonging to the decreed group (military personnel, workers of water utilities, catering departments, etc.) are hospitalized.
For dietary nutrition, tables No. 4, 2 and 13 are used. Antibacterial therapy is prescribed for 10–14 days (for the gastrointestinal form it can be limited to seven days) to all patients, regardless of the form of the disease, as early as possible (preferably before the third day of illness) [8] .
The choice of drug depends on the antibiotic sensitivity of Yersinia strains circulating in a given area (determined twice a year). Currently, preference is given to fluoroquinolones and third-generation cephalosporins [9, 10].
The main direction of pathogenetic therapy for the gastrointestinal form of yersinia infection is oral (parenteral) rehydration and detoxification with polyionic solutions.
The treatment tactics for patients with the abdominal form are agreed with the surgeon. The surgeon decides whether surgical intervention is necessary. Before and after surgery, etiotropic and pathogenetic treatment is carried out in full.
In the generalized form, etiotropic drugs, in most cases, are prescribed parenterally. In generalized forms with symptoms of pyelonephritis, pefloxacin has proven itself well - 0.8 g/day. Levomycetin succinate is used for the development of meningitis of yersinia etiology (7–100 mg/kg per day). In severe cases of the generalized form, several courses of parenteral antibiotic therapy are carried out. Start with gentamicin - for 2-3 days at 2.4-3.2 mg/kg per day, then 0.8-1.2 mg/kg per day. In the absence of a therapeutic effect or drug intolerance, streptomycin sulfate is used at a dose of 1 g/day. If hepatitis develops, you should avoid prescribing medications that have a hepatotropic effect. For patients with a septic form of the disease, it is advisable to administer two or three antibiotics of different groups (fluoroquinolones, aminoglycosides, cephalosporins) intravenously. If antibacterial therapy is ineffective, L. A. Galkina, L. V. Feklisova (2000) recommend using polyvalent yersinia bacteriophage (50.0–60.0 ml 3 times a day, No. 5–7) as monoetiotherapy or in combination with antibiotics [eleven].
In addition to etiotropic treatment, pathogenetic therapy is indicated (detoxification, restorative, desensitizing drugs, stimulants). In complex therapy, agents for the treatment of dysbiotic disorders must be used.
Most patients with severe asthenic, vegetative and neurotic manifestations require taking nootropic drugs, tranquilizers, bromides, peony infusion, motherwort tincture, valerian root decoction, etc. The selection of therapy in such cases is coordinated with a neuropsychiatrist and a vegetarian.
Treatment of patients with a secondary focal form of yersiniosis is carried out according to an individual scheme for each patient. Antibacterial drugs have no independent significance, but should be prescribed when clinical and laboratory signs of intensification of the infectious process appear and there is no history of taking antibiotics. Treatment of patients is coordinated with a rheumatologist, gastroenterologist, endocrinologist, psychoneurologist and other specialists (as indicated). Immunocorrectors should be prescribed to patients strictly according to indications in the absence of laboratory signs of an autoimmune process based on the results of a study of the immune status and autoantibodies in the patient’s blood.
Dispensary observation of convalescents. There is still no consensus on the duration and tactics of dispensary observation of convalescents of yersiniosis and pseudotuberculosis. In accordance with the orders and guidelines of the Ministry of Health (Order No. 408 of 1989; Appendix 6 to the Order of the Ministry of Health of the Russian Federation of September 17, 1993 No. 220 “Regulations on the office (department) of infectious diseases”, etc.), monitoring of convalescents of yersinia infection is carried out in depending on the nosology and severity of the disease for 1–6 months after discharge from the hospital (for mild forms - one month, for moderate forms - three months, for severe forms - six months).
Some researchers recommend using the following indicators to predict unfavorable outcomes of yersiniosis: unfavorable premorbid background (chronic diseases, grade 3-4 dysbiosis, burdened allergic history, etc.), long-lasting decrease in albumin, alpha proteins, urea-ammonia ratio, dysproteinemia, increased concentration blood ammonia, fibrinogen, neutrophilia, monocytosis, lymphocytosis, eosinophilia, low activity of the complement system, decreased levels of T- and B-lymphocytes in the period of convalescence and nonspecific resistance factors, high levels of circulating immune complexes (CIC), the presence of HLA B7, B18 and B27 , O (I) blood group.
However, dynamic observation of patients who have had yersiniosis and the use of modern methods of statistical processing of clinical and laboratory parameters allow us to express the opinion that the clinical manifestations of yersiniosis and pseudotuberculosis, their severity and duration are not objective criteria for prognosis, and therefore cannot be used for prognosis course and outcome of the disease. The immunoprognostic testing algorithm we created (
) patients in the acute period of the disease and the developed set of criteria for assessing immunograms for yersiniosis enable doctors to predict an unfavorable course and outcome already in the first 2–4 weeks from the onset of the disease [12, 13].
In our opinion, if the patient does not have criteria for adverse outcomes of yersiniosis infection, dispensary observation of convalescents is recommended for one year after discharge from the hospital. If there are indicators of possible adverse outcomes of yersiniosis, dispensary observation should be carried out for five years after discharge from the hospital - the first year every 2-3 months, then once every six months in the absence of complaints and deviations in health. In the presence of clinical and laboratory problems - more often, as necessary. According to indications, patients should undergo clinical, laboratory and instrumental examination by a rheumatologist, endocrinologist, cardiologist, ophthalmologist, dermatologist, etc.
The tactics of medical examination of patients with yersiniosis are not regulated at all by orders of the Ministry of Health of the Russian Federation. Based on our own results of long-term observation of patients with yersiniosis, we recommend the following tactics for their clinical examination. After discharge from the hospital, the duration of clinical observation for survivors of yersiniosis and pseudotuberculosis in the absence of genetic and immunological prognostic criteria for adverse outcomes should be one year, and if they are present, at least three years. To monitor the completeness of recovery, it is recommended to use the following scheme: during the first year after the acute period, patients must be examined comprehensively (clinical, laboratory, immunological methods) every 2–3 months, then once every six months in the absence of complaints and deviations in health. In the presence of clinical and laboratory problems - more often, as necessary. According to indications, during clinical examination, patients should be consulted with other specialists (rheumatologist, gastroenterologist, endocrinologist, cardiologist, ophthalmologist, dermatologist, gynecologist and gynecologist-endocrinologist) with the necessary laboratory and instrumental studies.
Literature
- Shestakova I.V., Yushchuk N.D., Andreev I.V., Shepeleva G.K., Popova T.I. On the issue of the formation of immunopathology in patients with yersiniosis // Ter. archive. 2005; 11:7–10.
- Opochinsky E. F., Mokhov Yu. V., Lukina Z. A., Yasinsky A. A. Analysis of the activities of the centers of the State Sanitary and Epidemiological Supervision of the Russian Federation for laboratory diagnosis of yersiniosis. In the book: Infections caused by Yersinia (yersiniosis, pseudotuberculosis), and other current infections. St. Petersburg, 2000: 42–43.
- Filatov N. N., Salova N. Ya., Golovanova V. P., Shesteperova T. I. Current state of laboratory diagnosis of yersiniosis in Moscow. In the book: Infections caused by Yersinia (yersiniosis, pseudotuberculosis), and other current infections. St. Petersburg, 2000: 59–60.
- Shestakova I.V., Yushchuk N.D., Popova T.I. Yersiniosis: diagnostic errors // Doctor. 2007; No. 7: 71–74.
- Yushchuk N.D., Shestakova I.V. Problems of laboratory diagnosis of yersiniosis and ways to solve them // ZhMEI. 2007; No. 3: 61–66.
- Ghukasyan G. B., Khachatryan T. S., Aleksanyan Yu. T., Khanjyan G. Zh. Epidemiological patterns of yersiniosis in Armenia. In the book: Infections caused by Yersinia (yersiniosis, pseudotuberculosis), and other current infections. St. Petersburg, 2000: 13.
- Belaya Yu. A. Yersinia in “healthy” people. Results of long-term prospective studies. In the book: Infections caused by Yersinia (yersiniosis, pseudotuberculosis), and other current infections. St. Petersburg, 2000: 5.
- Karetkina G. N. Yersiniosis. In the book: Yushchuk N. D., Vengerov Yu. Ya. (ed.) Lectures on infectious diseases. M.: VUNMC; 1999: 339–354.
- Luchshev V.I., Andreevskaya S.G., Mikhailova L.M. et al. Treatment of patients with yersiniosis with fluoroquinolone drugs // Epidem. and infectious Diseases. 1997; 3:41–44.
- Dmitrovsky A. M., Karabekov A. Zh., Merker V. A. et al. Clinical aspects of yersiniosis in Almaty. In the book: Infections caused by Yersinia (yersiniosis, pseudotuberculosis), and other current infections. St. Petersburg, 2000: 17–18.
- Galkina L. A., Feklisova L. V. Results of the use of polyvalent yersiniosis bacteriophage in the treatment of yersiniosis in children. In the book: Infections caused by Yersinia (yersiniosis, pseudotuberculosis), and other current infections. St. Petersburg, 2000: 11.
- Shestakova I.V., Yushchuk N.D., Balmasova I.P. Clinical and prognostic criteria for various forms and variants of the course of yersinia infection // Ter. archive. 2009, vol. 81,11: 24–32.
- Shestakova I.V., Yushchuk N.D. Chronic yersiniosis as a therapeutic problem // Ter. archive. 2010, vol. 82, 3: 71–77.
I. V. Shestakova , Doctor of Medical Sciences, Associate Professor N. D. Yushchuk , Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Medical Sciences MGMSU , Moscow
Contact information for authors for correspondence
Treatment of yersiniosis
How to treat yersiniosis is determined for each patient by the doctor individually. Treatment of yersiniosis is prescribed depending on the form of the disease and its clinical picture. Uncomplicated forms of intestinal yersiniosis require treatment with etiotropic drugs and detoxification therapy for 7-10 days, depending on the severity of the patient’s condition, orally or parenterally.
Yersiniosis is also treated with antibiotics. The septic form of yersiniosis, secondary foci of infection and intestinal forms of the disease against a background of weakened immunity are treated with 2-3 types of antibacterial agents for 12-14 days, with detoxification therapy and the prescription of drugs that promote rehydration. If necessary, probiotics and multienzyme preparations can be used.
A comprehensive study to identify the causative agent of yersinia (Yersinia enterocolitica) and pseudotuberculosis (Yersinia pseudotuberculosis), including serological tests and polymerase chain reaction (PCR).
Synonyms Russian
Tests for yersiniosis and pseudotuberculosis.
English synonyms
Laboratory Diagnostics of Yersiniosis, Enteropathogenic Yersiniae Lab Panel.
What biomaterial can be used for research?
Venous blood, feces.
How to properly prepare for research?
- The study is recommended to be carried out before starting antibiotics and other antibacterial chemotherapy drugs.
- Avoid taking laxatives, administering rectal suppositories, oils, limit (in consultation with your doctor) taking medications that affect intestinal motility (belladonna, pilocarpine, etc.) and drugs that affect the color of stool (iron, bismuth, barium sulfate), within 72 hours before stool collection.
- Do not smoke for 30 minutes before the test.
General information about the study
Yersinia are gram-negative, facultative anaerobic rods belonging to the family Enterobacteriaceae. There are 11 known species of Yersinia, three of which are causative agents of human diseases: Yersinia pestis is the causative agent of plague, Yersinia enterocolitica (Y. enterocolitica) and Yersinia pseudotuberculosis (Y. pseudotuberculosis) are intestinal pathogens. Although Y. enterocolitica and Y. pseudotuberculosis are different species, they have many similarities, especially in terms of clinical presentation and diagnosis.
The main “reservoir” of Yersinia is wild and domestic animals (pigs, rodents, sheep, goats, cows, dogs, cats and birds). It is believed that humans do not participate in the natural life cycle of these pathogens either as an intermediate or definitive host and that their infection is thus accidental. As a rule, infection with intestinal Yersinia occurs through the fecal-oral route through consumption of contaminated food (dairy products, raw or undercooked meat, especially pork). Both Y. enterocolitica and Y. pseudotuberculosis remain viable at low temperatures. Cases of transmission of infection from person to person or through transfusion of infected blood have been described, but are very rare.
It should be noted that not all intestinal Yersinia are pathogens. Thus, serotypes Y. enterocolitica O:3, O:8, O:9 and O:5,27 and Y. pseudotuberculosis O:1 and O:2 lead to the development of the disease in humans. Only the indicated serotypes are truly entropathogenic Yersinia.
A feature of enteropathogenic Yersinia is their affinity for lymphatic tissue. Penetrating through the intestinal mucosa, these microorganisms enter the mesenteric lymph nodes. The developing inflammatory response is accompanied by abdominal pain and diarrhea, as well as mesenteric lymphadenitis. In immunocompetent individuals, infection with enteropathogenic Yersinia is more often limited to gastroenteritis and regional lymphadenitis. If the causative agent of the disease is Y. enterocolitica, they speak of yersiniosis, if Y. pseudotuberculosis, they speak of pseudotuberculosis. Yersiniosis is more common than pseudotuberculosis. Both with yersiniosis and pseudotuberculosis, immunopathological phenomena in the form of reactive arthritis and erythema nodosum can be observed. In persons with immunodeficiency, as well as young children, severe forms of yersiniosis and pseudotuberculosis with bacterial dissemination and sepsis may be observed.
Diagnosis of yersiniosis and pseudotuberculosis is quite difficult. Although bacteriological culture of stool (blood or other biological materials) is considered the “gold standard” for diagnosis, it is difficult to implement. This is due to the fact that enteropathogenic Yersinia is difficult to distinguish from other intestinal microorganisms that normally predominate in the intestinal flora. After identifying the growth of Yersinia, additional biochemical tests are carried out to determine their enteropathogenicity. In addition, the bacteriological culture method is characterized by rather low sensitivity (103-106 CFU per gram of biomaterial sample is required to obtain a result). Taking these features into account, the diagnosis of yersiniosis and pseudotuberculosis is complex and includes the following additional tests:
- Polymerase chain reaction (PCR) is one of the molecular diagnostic methods, during which the genetic material (DNA) of a microorganism is determined in a sample of biomaterial (in feces). The main advantages of PCR are the speed of obtaining results, high sensitivity and specificity. This comprehensive study includes PCR analysis for Y. pseudotuberculosis.
- Serological tests. Antibodies to enteropathogenic Yersinia can usually be detected in the first 2-4 weeks of illness (IgM antibodies). It should be noted that due to a certain antigenic similarity of Yersinia to bacteria of other genera (Salmonella, Morganella, Brucella), serological tests may give false positive results. Another disadvantage of serological tests is that antibodies to Yersinia (IgG antibodies) persist for several years after infection, which can interfere with interpretation of the result. It should be remembered that the result of serological tests depends on the immune status of the body.
The accuracy of PCR and serological tests is less affected by antibacterial drugs than the bacteriological method. However, the most accurate test result will be obtained by analyzing the biomaterial obtained before the start of treatment.
Gastroenteritis that occurs when infected with enteropathogenic Yersinia is difficult to distinguish from salmonellosis, campylobacteriosis and other intestinal infections. For this reason, additional laboratory tests are often required.
What is the research used for?
- For the diagnosis of yersiniosis and pseudotuberculosis.
When is the study scheduled?
- If yersiniosis or pseudotuberculosis is suspected: fever, nausea, abdominal pain (pain may be localized in the right groin area), diarrhea, as well as erythema nodosum or reactive arthritis;
- in some cases, if acute appendicitis is suspected.
What do the results mean?
Reference values
For each indicator included in the complex:
- [07-115] Yersinia pseudotuberculosis, Yersinia enterocolitica, IgM, semi-quantitative
- [07-116] Yersinia pseudotuberculosis, Yersinia enterocolitica, IgG, semi-quantitative
- [09-101] Yersinia pseudotuberculosis, DNA [real-time PCR]
| Analysis | Positive result | Negative result |
| Yersinia pseudotuberculosis, Yersinia enterocolitica, IgM | Yersiniosis or pseudotuberculosis, current infection | Norm |
| Yersinia pseudotuberculosis, Yersinia enterocolitica, IgG | History of yersiniosis or pseudotuberculosis | Norm |
| Yersinia pseudotuberculosis, DNA [PCR] | Pseudotuberculosis | Norm |
What can influence the result?
- Time elapsed since infection;
- state of the body's immune system;
- use of antibacterial drugs (aminoglycosides, co-trimoxazole, cephalosporins, tetracyclines, fluoroquinolones).
Prevention of yersiniosis
Specific prevention of yersiniosis has not yet been developed. All preventive measures are based on the epidemiological characteristics of the infection. They come down to the fight against rodents as the main carriers of infectious diseases. In vegetable stores, warehouses and stores, rodents are periodically exterminated. In order to timely identify individuals with yersiniosis among domestic animals and birds, scheduled and extraordinary veterinary examinations are periodically carried out on farms. Dairy plants establish control over the processing of dairy products.
When storing fruits and vegetables, attention is paid to the quality of preventive measures for disinfection and deratization of vegetable stores when a new crop arrives. Current disinfection and deratization is carried out in winter and autumn. Places for storing any products that are not subject to heat treatment are subject to careful control; catering establishments monitor compliance with the technological and sanitary regime during storage and preparation of food. In the event of a separate disease or outbreak, the food enterprise from which the product that caused the infection came is identified.
In medical institutions, the prevention of yersiniosis is based on compliance with the anti-epidemic and sanitary regime adopted for intestinal infections. Along with sanitary measures, timely identification of relatives and medical personnel infected while caring for sick people is important.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Antibodies to the causative agent of yersiniosis IgG, Yersinia enterocolitica Ig G, quantity.
Antibodies to the causative agent of yersiniosis Ig G, Yersinia enterocolitica, Ig G, quantity.
— identification of antibodies that are produced by the immune system in response to infection with the causative agent of yersiniosis.
Yersinia enterocolitica
is the causative agent of yersiniosis. These are gram-negative rod-shaped bacteria.
The route of transmission is fecal-oral, that is, through contaminated food and water that contain bacteria.
The reservoir of infection is animals (pigs, rats, mice and other rodents, domestic animals and birds).
Yersiniosis
- an acute bacterial infectious disease that mainly affects the gastrointestinal tract. This disease has nothing to do with tuberculosis (the original name is associated with the external resemblance to tuberculosis granulomas identified in the tissues of sick animals).
The duration of the incubation period is 1–2 days. The minimum period is 15 hours, the maximum is 4 days.
Clinical picture of yersiniosis
The main clinical symptoms of the disease: acute onset, fever up to 38–40 ºС, fever, abdominal pain, mainly in the right iliac region, nausea, vomiting, loose stools without pathological impurities, pain in muscles and joints, enlargement of the liver, spleen and peripheral lymph nodes, joint pain, in many patients - a rash, often small-spotted, facial flushing, swelling and redness of the hands and feet. Lymphadenitis and polyadenitis, arthralgia, arthritis and polyarthritis are common manifestations.
Antibodies to Yersinia enterocolitica
The detection of specific antibodies to the pathogen can be observed by the end of the first week of the disease with a rapid increase in their concentration over 2 weeks and, subsequently, a decrease after 2–6 months. The study of antibodies should be carried out dynamically - in paired sera taken at the onset of the disease and then after 7-10 days. A 4-fold (or more) increase in Ig M antibody titer is considered a diagnostically reliable serological indicator. In the absence of pronounced dynamics of titers or the need to evaluate single results, the epidemiological situation and timing of the disease should be taken into account, and it is permissible to use a minimum conditional diagnostic titer of 1:100– 1:200.
Indications:
- examination of patients with clinical signs of acute intestinal infection;
- to confirm a clinical diagnosis upon receipt of a negative result of a bacteriological examination;
- for the purpose of retrospective confirmation of diagnosis;
- in case of late presentation of the patient, prescription of antibacterial therapy.
Preparation
It is recommended to donate blood in the morning, between 8 and 11 am. Blood is drawn on an empty stomach, after 4–6 hours of fasting. It is allowed to drink water without gas and sugar. On the eve of the examination, food overload should be avoided.
Interpretation of results
Units: U/ml
The result is given in the form of “negative” or “positive”. In the latter case, the antibody titer is indicated - the last dilution of the serum that gives a positive result.
An increase in antibodies by 4 or more times in 7–10 days is considered diagnostically reliable.
Positively:
- current or past infection. It is recommended to examine the patient at least twice - at the onset of the disease and with an interval of 7-10 days. A 4-fold or more increase in antibody titers is considered diagnostically reliable.
Negative:
- absence of infection;
- low concentration or absence of antibodies in the early period of infection.
Yersiniosis in children: relevance of the problem, clinical case
Incidence of yersiniosis in the Russian Federation during 2010–2015. consistently high with uneven distribution across individual territories. Higher incidence rates from 50 to 150 or more per 100,000 children are recorded in the northern regions of Russia. Indicators in the south of Russia are much lower - from 6 to 10 per 100,000 children [1].
The causative agent of the disease, Yersinia enterocolitica, persists in the environment for a long time (up to several months), which determines its epidemic significance.
The main source of infection is animals, people with yersiniosis and bacteria-shedding agents, which is confirmed by the growth of infected individuals during the complication of the epidemic situation and the possibility of nosocomial infection with yersiniosis.
Under natural conditions, the causative agents of yersiniosis exist as parasites of rodents and are released into the external environment with feces and urine. The most contaminated by Yersinia are long-term stored vegetables, in which the detection of the pathogen can be 10–20% or more [2].
Clinical diagnosis of yersiniosis is difficult due to the polymorphism of symptoms, which can be mistaken for various diseases of an infectious and non-infectious nature. The following clinical forms of yersiniosis are distinguished: gastroenterocolitic, icteric, arthralgic, eczematous, meningeal, catarrhal, mixed and septic.
The clinical picture of yersiniosis is characterized by an acute onset, toxicosis, an increase in body temperature to 39–40 °C, symptoms of damage to the gastrointestinal tract (nausea, vomiting, cramping or constant abdominal pain, loose stools). From the first day of the disease, patients may experience muscle and joint pain, injection of blood vessels in the sclera and conjunctiva, catarrhal phenomena in the oropharynx, exanthema, etc. With the development of the icteric form of yersiniosis, symptoms of liver damage come to the fore: pain in the right hypochondrium, an increase in the size of the liver and its pain on palpation, icterus of the skin and sclera, darkening of urine, discolored feces [3, 4]. The general clinical picture of the icteric form of yersiniosis bears little resemblance to viral hepatitis, but among the diagnostic errors of yersiniosis occurring with jaundice, this form of the disease is most often interpreted as viral hepatitis.
It should be noted that with the icteric form of yersiniosis and viral hepatitis, there are many common symptoms: icterus of the skin and sclera, enlargement of the liver and its pain, change in color of the skin and stool. At the same time, there are differences in the clinical picture of these diseases that are crucial for the diagnosis of yersiniosis even at the stages of anamnestic and clinical examination.
We observed three children aged 4 to 10 years who were admitted to the clinic with a referral diagnosis of viral hepatitis. In all cases, the leading clinical signs were toxicosis and jaundice.
Here is one of our observations.
Andrey K., 10 years old. A child from unfavorable living conditions. Got acutely ill. Body temperature increased to 38 °C, headache, weakness, nausea appeared, and appetite worsened. The next day, the patient’s health remained poor, the temperature remained at 38–38.5 °C, icterus of the skin and sclera, and dark urine appeared. Hospitalized on the second day of illness with a diagnosis of viral hepatitis.
When examined in the emergency department, the patient’s condition was serious, temperature 38 °C. Pronounced icterus of the skin and sclera. Pulse 90 per minute, rhythmic, satisfactory filling and tension, blood pressure 90/60 mm Hg. Art. Heart sounds are muffled and clear. Above the lungs, the percussion tone is clear, vesicular breathing. The abdomen is soft, not swollen, painless on palpation. The lower edge of the liver is palpated 6 cm below the costal arch, its surface is smooth, elastic, palpation is painless. The spleen was not palpable. The feces are colored, the urine is saturated. From the epidemic history it turned out that the patient had no contact with patients with jaundice, and had not received any injections over the past 6 months. All family members are healthy.
Blood test on admission: erythrocytes - 3.5 × 1012/l, hemoglobin - 122 g/l, leukocytes - 5.9 × 109/l, eosinophils - 2%, band leukocytes - 3%, segmented leukocytes - 46%, lymphocytes - 43%, monocytes - 2%, ESR - 6 mm/hour. Total blood bilirubin is 68 µmol/l with a predominance of the direct fraction. Alanine aminotransferase level (ALT > 31 µmol/l). Prothrombin index - 70%.
Despite the ongoing detoxification and antibacterial therapy (Cefotaxime in a daily dose of 2 g), followed by its replacement with amikacin in a daily dose of 10 mg/kg body weight, febrile fever persisted. Jaundice increased, and by the 11th day of the disease, total blood bilirubin increased to 129 µmol/l, direct - 97 µmol/l, indirect 32 µmol/l, fermentemia remained: ALT - 24.8 µmol/l, cholesterol - 5.14 µmol/l, alkaline phosphatase - 0.60 µmol/l. In the general blood test, with a normal number of leukocytes, neutrophilia with a band shift and ESR up to 60 mm/hour appeared. The liver increased to 8 cm below the edge of the costal arch and became more dense. The urine remained dark, the feces became discolored. Changing antibacterial therapy to Levomycetin sodium succinate at the rate of 50 mg/kg body weight (daily dose) made it possible to achieve relief of fever during the first 3 days of using this drug to low-grade levels and its normalization on the 10th day of treatment with Levomycetin (21st day of illness ). At the same time, there was a decrease in the icterus of the skin and sclera. By the 22nd day of the disease, total bilirubin was 47 µmol/l, ALT - 16.5 µmol/l, cholesterol - 1.7 µmol/l, alkaline phosphatase - 0.60 µmol/l. By the 30th day of the disease, the levels of total bilirubin and its fractions were completely normalized. The ALT level decreased to 2.38 µmol/l, the hemogram values were normal. The size of the liver has decreased. Complete normalization of ALT was achieved on the 37th day of the disease.
An additional blood examination for markers of viral hepatitis, blood culture, determination of antibody titer in paired blood sera using RNGA with yersinia antigen, examination for leptospirosis, pseudotuberculosis gave a negative result. Enzyme immunoassay blood test for yersiniosis is positive (IgM). On the 17th day of the disease, Yersinia enterocolitica serovar 03, biotype 4 was isolated from the patient’s blood. On the 19th day of the disease, this pathogen was isolated from the feces. On the 24th day of the disease, the antibody titer in the indirect hemagglutination reaction (IRHA) was 1:50, followed by a 3-fold increase in the antibody titer to the yersinia antigen. The isolated pathogen turned out to be sensitive to Levomycetin.
Final clinical diagnosis: yersiniosis, icteric form.
The peculiarity of this clinical observation is the high activity of hepatocellular enzymes, which is considered not typical for yersinia hepatitis.
A complex of anamnestic, clinical and laboratory data obtained during the examination of the patient allowed us to assume yersiniosis with a greater degree of certainty. Specific examination methods only confirmed the established diagnosis.
Analyzing the given clinical example, a convincing and simple argument can be made to reject viral hepatitis.
As we have seen, the patient noticed jaundice of the skin and darkening of the urine on the day when the body temperature rose to its maximum, but his health remained poor. With viral hepatitis, in the vast majority of cases, with the appearance of jaundice, the well-being and condition of the patients improve noticeably: the temperature normalizes (if it was elevated), appetite appears, weakness decreases, i.e., many symptoms of the pre-icteric period weaken or disappear completely. Only in the most severe course of viral hepatitis the appearance of jaundice is not accompanied by an improvement in the well-being of patients; on the contrary, the symptoms of intoxication may increase, but against the background of normal or, less often, low-grade fever.
Recognition of the icteric form of yersiniosis with a severe course of the disease can be simple or, on the contrary, not easy, and at the stage of outpatient examination, impossible. The diagnosis is simple during an outbreak of yersiniosis and very difficult in sporadic cases of infection, as in our example.
Differentiation of yersiniosis from typhoparatyphoid diseases, leptospirosis, viral hepatitis, pseudotuberculosis, etc. in an infectious diseases hospital is not difficult and is based on studying the dynamics of the main manifestations of infection, differences in hematological changes and, most importantly, on the isolation of the pathogen and the results of a serological examination . It should be remembered that negative results of serological testing for yersiniosis do not exclude the diagnosis. To increase the reliability of the diagnosis, it is necessary to use bacteriological and serological methods.
The bacteriological method makes it possible to determine the pathogen in sick people, animals, and also on environmental objects. The materials for the study are: swabs from the nasopharynx, blood, joint fluid, cerebrospinal fluid, surgical material, feces, urine. It is advisable to conduct a bacteriological study before starting antibacterial therapy, in the first week of the disease, three times. The results of this study are obtained in 2–3 weeks.
For early diagnosis, immunological methods for identifying pathogen antigens are used: enzyme immunoassay, indirect immunofluorescence reaction, latex agglutination reaction, etc. The materials for these studies are saliva, blood, coprofiltrates, animal organs, swabs from environmental objects. It is better to conduct research in the first 10 days of the disease, using at least 2 types of materials from patients.
For serological diagnostics in order to identify specific antibodies, the agglutination reaction (diagnostic titer 1:160) and RNGA are used. Available for most infectious disease hospital laboratories is the determination of antibodies to Yersinia enterocolitica 03 and 09 by the RNGA method. A titer of 1:400 is considered diagnostic. Studies are carried out from the 5th–7th day of illness in paired blood sera taken at an interval of 10–14 days. In recent years, genetic diagnostics—polymerase chain reaction—have become more frequently used [5].
The drugs of choice for the treatment of yersiniosis are antibacterial drugs: III generation cephalosporins, II–III generation aminoglycosides, doxycycline (from 8 years of age), chloramphenicol (Levomycetin), carbapenems (for generalized forms of yersiniosis). The duration of treatment is 10–14 days or more according to indications. Pathogenetic therapy includes detoxification, antihistamines, immunocorrection for severe forms using immunoglobulins for intravenous administration. According to indications, sorbents, enzymes, antispasmodics, hepatoprotectors, antipyretics, etc. are prescribed [3, 5, 6].
Literature
- Karbysheva N.V., Bobrovsky E.A. Activity of natural foci and morbidity in yersinia infection // Journal of Infectology. 2016. T. 8 (2). P. 52.
- Ogoshkova N.V., Kashuba T.G., Drozdova O.O., Lyubimtseva N.N. Clinical and epidemiological characteristics of yersiniosis / Current issues of infectious pathology and vaccine prevention. Materials of the XII Congress of Children's Infectious Diseases of Russia. M., 2013. P. 52.
- Yushchuk N. D., Vengerov Yu. Ya. Kryazheva S. S. Infectious human diseases M.: OJSC Publishing House "Medicine", 2009. P. 78–79.
- Serova Yu. S., Kuimova I. V., Vasyunin A. V., Krasnova E. I. Frequency and severity of articular syndrome in pseudotuberculosis in children / Current issues of infectious pathology and vaccine prevention. Materials of the XII Congress of Children's Infectious Diseases of Russia. M., 2013. pp. 60–61.
- Children's infections / Ed. L. N. Mazankova. M.: MEDpress, 2009. pp. 76–81.
- Kharchenko G. A., Oganesyan Yu. V., Maruseva I. A. Infectious diseases in children: diagnostic and treatment protocols. Textbook allowance. Rostov-on-Don: Phoenix, 2007. pp. 48–49.
G. A. Kharchenko1, Doctor of Medical Sciences, Professor O. G. Kimirilova, Candidate of Medical Sciences
Federal State Budgetary Educational Institution of Higher Astana State Medical University, Ministry of Health of the Russian Federation, Astrakhan
1 Contact information