Leptospirosis is a bacterial disease of animals and humans that occurs with symptoms of fever, progressive anemia, jaundice, affects the kidneys, liver, central nervous system, and causes abortions.
The disease was thoroughly studied at the end of the 19th century by scientist N.P. Vasiliev. He described in detail several cases of the disease. Adolf Weil described the disease almost at the same time, so for a long time the disease was named after the scientists “Vasiliev-Weill disease”.
In 1915, Japanese scientists first isolated the Leptospira culture. Thanks to them, in subsequent years, various species of Leptospira were identified and studied in many parts of the world.
Pathogen
Leptospira are divided into two types - parasites and saprophytes. Under a microscope, leptospires are mobile, long, thin, silvery filaments with curved ends. Bacteria grow well on nutrient media of varying densities. They reproduce best at a temperature of +28°C. The pathogenicity of Leptospira is determined by enzymes, hemotoxins and endotoxins.
There is a species-specific sensitivity of animals to various serological variants of Leptospira. With all the diversity of these microorganisms, they are usually united into one species - Leptospira, among which there are various serovars belonging to pathogenic leptospira (interrogans) or saprophytic (biflexa). In total, there are currently about 200 pathogenic representatives of the species and about 60 non-pathogenic ones. In addition to hydrophilicity, a distinctive property of Leptospira is the need for oxygen to carry out vital processes; they are classified as strict aerobes.
The name of the species itself comes from the Latin words “small” and “spiral”, which very accurately characterize the appearance of the microorganism. Among other things, Leptospira have the ability to move.
Leptospira are quite stable. In the urine of leptospiron carriers they remain viable for up to a week, in the kidneys for up to two weeks, in an aborted embryo for several days, in muscles for up to 2 days, in milk for up to a day, and in deep-frozen sperm pellets of producers for several years.
In the environment, Leptospires remain in liquid for a long time, and therefore they are classified as hydrophilic microorganisms. Bacteria live in reservoirs for six months, in wastewater for more than a week, in manure for about a day, in moist soil for up to 280 days, but in dry conditions they die instantly. Leptospires also quickly die when exposed to disinfectant solutions containing chlorine, formaldehyde, and caustic soda.
Routes of infection
The pathogen enters the human body through water, food, and less commonly through direct contact with an infected animal. You can become infected with leptospirosis:
- during agricultural work;
- when bathing, washing and swallowing water - both fresh and sea;
- when eating foods that have been exposed to the urine of infected animals;
- upon contact with bacteria-carrying animals;
- when bitten by an infected animal.
A person who has recovered from leptospirosis develops a stable, but not specific, immunity. This means that there is a high probability of re-infection, but with leptospira of a different subspecies with a different antigenic structure.
Epizootological data
The disease is widespread in almost all countries of the world. It is believed that only the territories adjacent to the southern and northern poles of the planet are free from leptospira. The disease manifests itself in single outbreaks or in the form of mass infection. The peak of infection is autumn and spring. The disease affects mammals and birds, regardless of gender and age. However, it has been noted that young animals suffer the disease more severely. The source of infection is sick animals or those who have recovered from the disease - they excrete bacteria in urine, feces, sputum, and semen. Contribute to the development of the disease:
non-compliance with veterinary and sanitary standards; violation of the rules of disinfection and deratization; grazing of animals on undeveloped pastures; lack of safe watering places; violation of feeding standards. Dogs carry leptospirosis for several years, cats for up to 12 weeks, foxes for a year and a half, and rodents for their entire lives. Thus, the most dangerous carriers of the disease are canines and various rodents.
Susceptible animals are most often infected through nutritional means - with food and water, and less often through insect bites. In farm animals, the disease is detected, as a rule, after grazing in flooded meadows or in marshy areas, watering from water bodies unfavorable for leptospirosis. Predators become infected by eating rodent carriers, while fur-bearing animals become infected by eating contaminated offal.
Prevention
There are the following measures to prevent leptospirosis:
- Vaccination is carried out from 7 years of age. In adulthood, vaccinations are given to people who, due to their profession, often come into contact with animals. We are talking about veterinary and agricultural workers, as well as those who work in slaughterhouses or live in epidemic-prone areas and have close contact with homeless animals.
- Very careful adherence to personal hygiene rules.
- Refusal to swim in untested bodies of water.
- Compliance with safety measures when working with animals.
- Correct and timely treatment of damage to mucous membranes and skin - for this you need to use special products.
- Immediately contact a specialist when the first symptoms of leptospirosis appear.
Pathogenesis
The development period ranges from 1–2 to 12 days. Bacteria enter the body through damaged skin or microtraumas on the mucous membranes and penetrate through the bloodstream into all parenchymal organs. There they actively multiply and enter the blood again, causing intoxication of the body.
Subsequently, antibodies begin to appear in the body, which, in addition to destroying the pathogenic bacteria, destroy blood cells and tissues of parenchymal organs. This fact enhances the destructive effect of toxins released during the death of Leptospira. As a result, the animal begins to become anemic and the functioning of internal organs is disrupted. In particular, impaired renal function leads to hematuria, and liver dysfunction and accumulation of bilirubin in the blood leads to jaundice.
In pregnant animals, leptospirosis penetrates the placenta, causing its destruction. Animals abort several weeks after infection. However, if the disease affects the female in the second half of pregnancy, the fetus often survives, thanks to the antibodies formed in its blood.
In the toxic stage of the disease, the risk of mortality of the animal is high. It is worth mentioning that the body's antibodies develop faster, which leads to the death of leptosyr in the entire body, except the kidneys. Bacteria are excreted in urine for a long time.
Classification
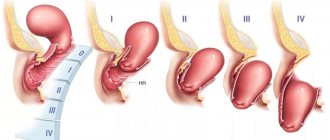
There are two forms of the disease - icteric and anicteric .
- Jaundice - the incubation period in this case lasts 1-2 weeks. It begins acutely, body temperature can rise to 40 degrees, and a pronounced feeling of weakness appears. Around day 2-3, the liver enlarges, and in some cases, the spleen. I am worried about pain in the calf muscles, icterus appears in the sclera and skin. Oliguria develops around day 4-5 , later anuria . Hemorrhagic syndrome appears. Tachycardia is a concern , infectious myocarditis . This form of the disease is sometimes called “infectious jaundice.”
- Anicteric - the incubation period lasts 4-10 days. The patient experiences weakness, body temperature, weakness, develops meningeal signs, disseminated intravascular coagulation syndrome, oliguria, and liver enlargement.
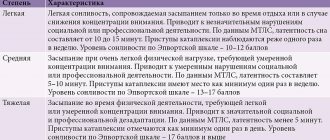
According to the severity of the disease, three degrees are distinguished:
- mild – mild intoxication, internal organs are not affected;
- moderate – severe intoxication, all the symptoms of leptospirosis are present;
- severe - damage to internal organs occurs.
Symptoms
The clinical picture of leptospirosis largely depends on the serogroup of the pathogen, its damaging ability, the amount of the pathogen that has entered the body and the susceptibility of the organism. The disease progresses:
1. Lightning fast.
2. Spicy.
3. Subacute.
4. Chronically.
5. Atypical.
The fulminant course is characterized by an increase in temperature, loss of strength and depression. Occasionally, animals become restless, turning violent. The pulse is frequent, thread-like. Breathing is also frequent. Sometimes jaundice appears and blood is found in the urine. Death occurs within 24 hours after the first onset of symptoms.
The acute course is often found in young animals and is accompanied by an increase in temperature, refusal of food, impaired chewing of the cud in livestock, depression, and apathy. After a few days, the mucous membranes turn yellow, the animal has difficulty defecating, and the urine is brown or red. When touching the liver area, pain is observed. The animals bend and groan. There is a disturbance in the functioning of the gastrointestinal tract. Pregnant animals abort, milk production in cows decreases, and the milk changes color to yellow. The fur becomes dull, hematomas appear, which subsequently become necrotic. Tachycardia and rapid breathing are noted. The duration of the acute course is up to 10 days. If there is no treatment, the animal dies. Convulsions occur before death. The animal dies from asphyxia.
The subacute course is accompanied by similar symptoms, but develops slowly. The illness lasts about a month and often ends with recovery.
The chronic form is more rare and is accompanied by exhaustion, anemia, tissue necrosis, hematuria, and rapid breathing. Temperature rises from time to time and urination is frequent. Animals hide in dark places. Cows have reduced milk production and milk fat content. Molting is disrupted and some areas become bald. Sick animals often become infertile or often abort in later stages. The offspring of such animals are weak and non-viable. In the postpartum period, an exacerbation of the disease is often observed.
The chronic form rarely ends in recovery. The death of animals occurs due to exhaustion or failure of parenchymal organs.
The atypical form proceeds unnoticed at first. Only temporary slight increases in body temperature, pallor, and slight weakness are noted. The symptoms disappear and the animals recover.
In pigs, leptospirosis is asymptomatic. Only rarely does temporary fever, conjunctivitis, rash, jaundice, anemia of the mucous membranes, indigestion, paresis or paralysis, abortion occur.
In horses, the symptoms of leptospirosis are identical to ruminants. In addition, trembling, lameness, and muscle pain are noted.
In predators, leptospirosis occurs with an increase in temperature to 41°C, lethargy, lack of appetite, vomiting, thirst, and falling on the hind limbs. Digestive disorders are observed with bloody stools. Jaundice always occurs in fur-bearing animals, unlike dogs. The urine is dark, urination is frequent and in small volumes. The mucous membranes of the mouth and eyes become inflamed. The disease lasts from two to twelve days, mortality is up to 90%.
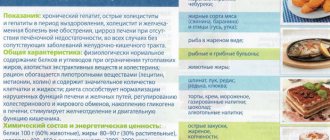
Diet
Diet 5th table
- Efficacy: therapeutic effect after 14 days
- Duration: from 3 months or more
- Cost of products: 1200 - 1350 rubles per week
Diet 7 table
- Efficacy: therapeutic effect after a week
- Terms: 1 month or more
- Cost of products: 1200-1300 rubles per week
In order for the treatment to be as effective as possible, the patient is recommended to adhere to the Table No. 5 , which has a beneficial effect on the liver. In case of kidney damage, it is recommended to follow the diet Table No. 7 .
The patient's diet should contain the following products:
- Fresh vegetable and fruit juices, compotes, rosehip decoction.
- Pumpkin, carrots.
- Oatmeal, buckwheat.
- Honey.
- Lean meat and fish.
- Vegetable soups.
- Egg white, one egg per day is allowed.
- Low-fat cottage cheese, yogurt
- Stale bread, oatmeal cookies.
The following should be excluded from the diet:
- Meat of young animals, fatty meat.
- Mushrooms.
- Fatty fish.
- Legumes.
- Salty foods.
- Alcohol.
- Canned food, smoked meats.
- Soda.
Pathological changes
The mucous membranes of corpses are jaundiced, and necrotic areas are noted on the skin and mucous membranes. The corpse is dry, emaciated, the coat is dull, and there are often bald patches. At autopsy, all organs have a pronounced icteric tint. The liver is enlarged, flabby, brick, ocher or clay in color, the tissues are flabby, brittle. The gall bladder is filled with viscous dark green or brown contents.
The kidneys are swollen, flabby, and there are signs of pyelonephritis. The boundaries of the renal layers are smoothed, pale, with hemorrhages. In the renal pelvis, gelatinous red contents are often observed. The bladder is inflamed, with areas of necrosis, filled with brown, less often cherry-colored urine.
Diagnostics
The diagnosis of Weil's disease is based on the following symptoms: acute febrile onset with pain in the occipital muscles and calves, conjunctivitis with photophobia, nosebleeds, hemorrhagic herpes, icterus of the sclera, with the appearance of jaundice and albuminuria towards the end of the febrile period.
Other symptoms, such as vomiting, frequent mucous stools, dry mouth, coated dry tongue, hyperemia of the pharynx and larynx, apathy, insomnia, can occur with a number of other diseases and especially with food infections and poisoning. The blood picture makes it possible to easily distinguish the disease in the first days from typhoid fever; further differentiation can be made by the absence of a diazoreaction, and subsequently by the absence of the Widal reaction and typhoid blood culture.
Diagnosis and treatment
A lifetime diagnosis is made taking into account the epidemiological situation in the region and symptoms. Laboratory tests of blood and urine are done to confirm. Leptospirosis is differentiated from canine distemper, hepatitis of various etiologies, poisoning and toxic infections.
A post-mortem diagnosis is confirmed after examining the heart, liver, kidneys, bladder (possibly a fetus with placenta) of the deceased animal. The corpses of small animals are sent in their entirety; from large animals, the corpses are collected and sent in sealed containers. Pathological material is studied within 6 hours after the death of the animal.
Sick animals are quarantined in an isolated room and treated. A specific measure is the use of hyperimmune serum. In addition, animals undergo a course of antibiotic therapy (bicillin, streptomycin, ditetracycline), if necessary, symptomatic therapy is prescribed - droppers with glucose solution, treatment of necrotic areas, drugs to normalize digestion, etc.
List of sources
- Avdeeva M.G. Leptospirosis as a disease with a prolonged complicated course (immunopathogenesis, diagnosis, prognosis, treatment, rehabilitation): abstract of thesis. Dr. med. Sci. - M., 1997. - 32 p.
- Avdeeva M.G. Causes of lethal outcomes of leptospirosis / M.G. Avdeeva // Epidemiology and infectious patients. – 2003. – No. 6. – P. 30–33.
- Leptospirosis / [V.I. Luchshev, V.V. Lebedev, S.N. Zharov, S.V. Burova] // Russian Medical Journal. – 2009. – No. 4. – P. 47–49.
- Stoyanova N.A. Current problems of leptospirosis in infectious pathology of people // Sat. report/Biol. scientific-practical .-SPb., 1996.-Issue 2.-P.5-10.
Complications of leptospirosis
In addition to leptospirosis meningitis, which is benign, the following may be observed: tracheobronchitis, bronchopneumonia, pyelitis, pyelonephritis, endocarditis, myocarditis, as well as eye damage in the form of uveitis, iritis, iridocyclitis. In Vasiliev-Weil disease, a rare complication may include bilateral inflammation of the optic nerves, as well as arterial thrombosis and myelitis, which can result in paraplegia. Ictero-hemorrhagic leptospirosis can activate a dormant salmonella infection. The most common complication determined pathologically is pneumonia, predominantly of a hemorrhagic nature.
In severe water fever, early and late eye complications are often observed. The first group (complications during the febrile period and in the next 2 months) includes: conjunctivitis without bacterial flora in the mucosal discharge, acute, favorable iritis and iridocyclitis, anterior exudative choroiditis, accompanied by opacification of the vitreous body. Late complications that occur in the period from 2 months to 1 year or more after recovery include iridocyclitis with intense opacities in the vitreous body and, less commonly, damage to the optic nerve, choroid and retina, as well as choroidal cataracts that form with severe iridocyclitis.
Historical reference
Infectious jaundice (later called leptospirosis) was first described by the German scientist A. Weil in 1886 and S.P. Botkin’s student N.P. Vasiliev in 1888, which served to distinguish the disease into an independent nosological form. The causative agent of the infection was discovered in 1914 - 1915 by Japanese researchers R. Inado and U. Ido. In subsequent years, various serotypes of Leptospira were isolated and studied.
Rice. 2. View of Leptospira under dark-field microscopy.
Epidemiology
The characteristics of leptospirosis as epidemic forms are determined by the following reasons: infection of various synanthropic and field rodents with leptospira; their ability to excrete these microorganisms in the urine for a long time; the predominant infection of various types of rodents with certain types of pathogenic leptospira, the possibility of the formation of powerful additional (but often independent) sources of infection in the form of farm and domestic animals that receive infectious origin from rodents; the duration of release of the pathogen into the external environment by infected animals; preservation of Leptospira viability in water and moist soil for a number of weeks; non-contagiousness of people with leptospirosis.
A. Natural reservoirs and sources of infection
The main reservoir of the causative agent of Vasiliev-Weil disease is rats. These rodents find themselves infected with ictero-hemorrhagic Leptospira everywhere.
In rats of both sexes, no significant fluctuations in Leptospira infection have been established depending on the seasons of the year, and therefore there is a constant reservoir of pathogenic Leptospira in populated areas.
Synanthropic rodents are infected, as a rule, with ictero-hemorrhagic leptospira, but individual objects can be found (barnyards, pigsties, slaughterhouses, bone processing plants, etc.) in which they are infected predominantly and even exclusively with other types of leptospira.
Such microfociality of leptospirosis infection is associated with the relative constancy of the habitats of certain species of rodents. It is regulated by the number (“density”) of the latter at a given stage and the unequal ability of individual types of Leptospira to adapt to the body of various representatives of the order of rodents.
The main reservoir of the causative agent of water fever are wild mouse-like rodents, as well as some insectivores. This determines the predominantly rural nature of outbreaks of water fever and the summer-autumn seasonality of the latter.
The epidemiological significance of different rodents and other small mammals varies. It is associated with the biological characteristics of individual species (the rate of reproduction and possible population density, the degree of adaptation to the external environment, the ability to migrate, susceptibility to pathogens, etc.), and is also determined by the frequency of contact of these animals with humans and the natural features of their habitats . The connection of pathogenic Leptospira with water bodies and wetlands determines the special role of moisture-loving species of rodents, in particular voles.
Additional sources of Leptospira are farm animals, as well as commercial (foxes, arctic foxes) and domestic (dogs, cats) animals. The epidemiological significance of farm animals is especially great, since the emergence of secondary (but later independent) foci of leptospirosis infection may be associated with them.
In contrast to rodents, in which leptospirosis occurs as an asymptomatic infection, in agricultural, commercial and domestic animals, along with this form of the course, severe diseases often occur, characterized by a short febrile period, jaundice, and the release of bloody urine. Milk from cows may acquire a yellowish color, and an admixture of blood can be detected in it. There is a fulminant course of the disease (especially in young animals), ending in the death of animals after 1-2 days, as well as acute, subacute and chronic forms. During epizootics, deaths in animals (mainly among young animals) reach tens of percent.
Infection of farm animals most often occurs through water, on pastures or during the movement of livestock. Infection is also possible when kept in stalls. New foci of infection can arise in previously prosperous farms, even when several heads of sick or sick animals are introduced into them - leptospira excretors. Infection of commercial animals kept in nurseries usually occurs when eating meat from patients with leptospirosis and slaughtered or dead animals.
The particular epidemiological significance of farm animals is associated with close and everyday human contact with them. It is also due to the duration and massiveness of excretion in the urine of animals that are sick or have had leptospirosis infection.
B. Leptospira transmission factors
The main factor in the transmission of leptospirosis pathogens is water into which the secretions of sick animals have entered. When released into water sources, pathogenic Leptospira remain viable for about a month. The direct cause of human infection is the consumption of raw water from household water sources such as ponds and wells, swimming in small, stagnant or weakly flowing bodies of water, for example, in rivers with a quiet flow, muddy bottom and marshy banks, or wading them.
Various food products, both contaminated with rodent secretions and those originating from sick farm animals (milk, meat), may have a certain role in the transmission of leptospirosis infection. When artificially infecting a number of food products with ictero-hemorrhagic leptospira, it was found that these microorganisms remain viable from 30 minutes to 13 days, with the longest period of time in liquid and semi-liquid food with a slightly alkaline reaction at a temperature of 4-5°C.
Animal carcasses that have a pH above 6.0 24 hours after slaughter may still contain viable Leptospira.
Sporadic diseases of ictero-hemorrhagic leptospirosis occur all year round, which corresponds to the constant infection of rats. Despite this, Weil's disease does not normally become epidemic. The latter arise only with a sharp deterioration in sanitary and hygienic conditions, as a result of which the possibility of contact with rodents increases and additional factors for the transmission of Leptospira are created.
Epidemic outbreaks of leptospirosis occur mostly in the summer-autumn period (August-October). This is due to an increase in the number of rats in these months and to meteorological conditions that are most favorable for the preservation of Leptospira in the external environment.
Water fever (anicteric leptospirosis) is a disease predominantly found in rural areas. It is characterized by a particularly pronounced summer-autumn seasonality. Its epidemiological uniqueness is largely determined by the ecological and biological characteristics of natural reservoirs of infections (small mammals, mainly wild mouse-like rodents). The main transmission factors are water and moist soil. Therefore, epidemic outbreaks of water fever are usually associated with certain landscapes (wetlands, water meadows, banks of rivers and lakes). Group diseases caused by contamination of ponds, wells, water-filled excavations, and open tanks were observed.
Individual cases of water fever can be recorded throughout the year, but the highest number of diseases is observed in warm seasons. This is due to the greatest number and activity of mouse-like rodents in the summer-autumn period, the presence of farm animals on pastures, and increased contact of people with sources and factors of transmission of infection during field harvesting work.
The seasonal distribution of diseases can vary to a certain extent depending on local climatic conditions and the biological properties of animals - sources of infections.
The age composition of patients during individual outbreaks of water fever is different, which is associated with the characteristics (type) of these outbreaks.
The direct cause of infection for the most part is: swimming, hunting in wetlands, fishing, haymaking barefoot in low-lying areas and flooded meadows, working in artificially irrigated fields, such as rice fields, contact with infected farm animals (cows, calves, pigs, horses) ) etc.
Water fever can also occur in urban settlements (for example, among workers in suburban livestock farms), as well as among workers in slaughterhouses and primary processing workshops at meat processing plants. Under these conditions, the diseases are of a pronounced occupational nature and are characterized by a peculiar microfocality. In addition to rodents and farm animals, dogs may also be involved in the epizootological chain.
The significant adaptive ability of Leptospira makes it possible to widely exchange various types of these microorganisms between field and synanthropic rodents, wild, agricultural and domestic animals.