Unpleasant in appearance and bitter in taste, bile was perceived by many peoples in the past as the cause of a person’s bad character. There is indeed some truth in this: diseases of the gallbladder may well poison the life of a person and everyone around him at the same time. But under normal conditions, bile performs a number of important functions in the body, most of which are related to digestion.
It is this that creates an environment in the intestine that is favorable for pancreatic enzymes. With its help, cholesterol, bilirubin and a number of other substances that are not filtered by the kidneys are removed from the body. It activates enzymes necessary for the digestion of proteins. The acids it contains break down fats...
Bile is produced in the liver, some of it accumulates in the gallbladder. When a person eats, bile from the liver and gallbladder flows through the ducts into the small intestine. But sometimes problems arise with the evacuation of bile - it stagnates in the gallbladder. As a result, an inflammatory process develops in this organ - cholecystitis.
The causes of inflammation can be different, but the most common is the presence of stones in the gallbladder. Doctors call this form of the disease calculous cholecystitis. This is one of the types of gallstone disease.
Causes
Doctors identify several main risk factors for the incidence of chronic calculous cholecystitis:
- middle and old age;
- pregnancy and childbirth;
- overweight and obesity;
- too sudden loss of body weight;
- starvation;
- total parenteral nutrition;
- family history, heredity;
- taking a number of medications (fibrate derivatives, contraceptive steroids, estrogens during the postmenopausal period, progesterone, octreotide and its analogues, ceftriaxone);
- Crohn's disease, diabetes mellitus, liver cirrhosis, biliary system infections, choledochal and duodenal diverticula.
Diet therapy
Diet and nutrition directly affect the functioning of the biliary system. For diseases of the gallbladder and liver, therapeutic diet No. 5 is prescribed. The basic rules of such nutrition are fractionalization and rationality. The energy value of the diet must meet the individual needs of the body. The difference between therapeutic nutrition is the absence of choleretic products and difficult-to-digest foods. Fats are not completely excluded; it is preferable to consume them in the form of vegetable oils and butter. Simple carbohydrates are eliminated and the amount of fiber increases.
It is important to eat every two and a half hours and before bed. Hunger for more than 4 hours negatively affects the condition of the gallbladder. Portion sizes must correspond to the physiological needs of a person. It is important to avoid overeating. Errors in nutrition during cholelithiasis and chronic cholecystitis can cause exacerbation.
- fatty meat and fish, offal, rich broths;
- alcohol;
- strong coffee and tea, carbonated drinks, undiluted sour juices;
- vegetables with a high content of oxalic acid and essential oils: fresh garlic and onions, radishes, turnips, sorrel, spinach, white cabbage;
- sour fruits, berries;
- rye bread, baked goods, desserts with cream;
- chocolate, cocoa, snacks, nuts, mushrooms;
- legumes, corn, millet cereals.
Cooking methods are limited: fried and sautéed foods are excluded, preference is given to boiled and steamed food. If cholelithiasis occurs without symptoms, stewing and baking can be allowed.
During the period of exacerbation of cholecystitis, the diet becomes more strict. During an attack, the patient is advised to fast for one to two days. After stopping the attack, diet No. 5a is prescribed. Food is crushed and ground; porridges and vegetarian pureed soups are preferred. Dishes are served warm; cold and hot foods, which can cause spasm of the sphincter of Oddi, are excluded. In addition to the prohibitions of diet No. 5, fresh vegetables and fruits are excluded from the diet. Only boiling and steaming are allowed. Salt and sugar are limited as much as possible. Two weeks after the attack subsides, the patient can switch to a basic diet.
Mineral water therapy
Drinking treatment for cholecystitis has a beneficial effect on the functioning of the liver, effectively improves the composition of bile, helps normalize gallbladder motility, and cleanses the biliary system of inflammatory fluid. You can be treated in this way in a sanatorium or at home.
Waters of low and medium mineralization containing magnesium, sodium, chlorine ions and organic substances are beneficial. The choice depends on the state of the digestive system. For cholecystitis, it is recommended to take warm and hot water up to 45 degrees.
Typically, treatment begins with a serving of 50–100 ml three times a day 1–1.5 hours before meals. During the first week, the single dose is gradually increased to 250 ml. The course of therapy is 35–40 days. The break between treatment with mineral waters should be long, at least 4 months.
In case of impaired motility of the gallbladder and stagnation of bile, drinking tubes quickly help. The patient drinks a glass of warm mineral water in the morning on an empty stomach, then performs a set of physical therapy exercises. After this, he drinks another 200 ml of water and lies down with a heating pad on his right side. When the procedure is carried out correctly, pain, nausea, and bitterness in the mouth quickly decrease. At home, tubing is carried out 1–3 times a month, under the supervision of doctors – 1–2 times a week. This treatment is contraindicated for cholelithiasis.
For the calculous form of cholecystitis, tubages and mineral waters that have a pronounced choleretic effect or with a high level of mineralization are not recommended. After cholecystectomy, you can be treated in this way after 3-4 months at home, but under the supervision of a doctor.
Symptoms and complications
Pain syndrome. Chronic calculous cholecystitis is characterized by various types of abdominal pain. As a rule, it has a pulling, dull or aching character; in the vast majority of cases, its localization is in the area of the right hypochondrium. 20−30% of patients complain of epigastric pain; in some cases, the pain syndrome is not characterized by a clear localization. The pain radiates to the lumbar region on the right, under the shoulder blade, to the shoulder and the side of the neck.
Hepatic colic. This symptom is a distinctive feature of calculous cholecystitis. This is a sudden onset of acute cramping pain under the right rib. Such cholecystitis often occurs latently, and its first sign is hepatic colic.
Bile intoxication and jaundice. Calculous cholecystitis is characterized by signs of jaundice and intoxication of the patient’s body with bile acids. The sclera, skin, and mucous membranes acquire a yellowish tint. Patients often complain of itchy skin, and upon examination, marks of scratching can be seen on the skin. If the flow of bile is significantly impaired, the urine becomes dark and the feces become discolored. Manifestations of bile intoxication are: low blood pressure, irritability, decreased heart rate, headache, sleep disturbances.
Dyspeptic symptoms. Unstable stools, nausea, belching, metallic or bitter taste, and dry mouth are noted. When the gallbladder suddenly empties, heartburn and vomiting of bile are possible.
The most significant complications of calculous cholecystitis are:
- choledocholithiasis (blockage of the common bile duct with stones);
- stenosis of the papilla of Vater;
- chronic or acute pancreatitis;
- hepatitis, reactive cholangitis;
- subphrenic abscess;
- empyema and perforation of the gallbladder;
- peritonitis.
Signs of cholecystitis
Symptoms of cholecystitis depend on the form of the disease, the presence or absence of stones. In inflammation complicated by cholelithiasis (cholelithiasis), the manifestation of hepatic colic often occurs. Its symptoms include the following:
- sharp pain on the right. The attack occurs suddenly, the pain increases over a short period of time, lasting from several minutes to several days. As the pain subsides, it becomes aching and persists for a long time;
- bitter taste in the mouth;
- nausea, vomiting, after which there is no relief;
- yellowing of the sclera and skin;
- bloating;
- bowel dysfunction (constipation);
- elevated body temperature: up to 37.5–38 ˚С in simple forms and up to 39 ˚С in purulent forms of acute cholecystitis.
Chronic cholecystitis does not manifest itself so clearly, and there may be no stones in the gallbladder. A prolonged inflammatory process can manifest itself with the following symptoms:
- heaviness in the right hypochondrium, weak aching pain;
- pain radiating to the right collarbone, shoulder blade, arm, to the left side of the abdomen after eating fatty, smoked foods, marinades, alcohol, soda, undergoing intense exercise, stress;
- appetite disorders;
- bitter belching;
- nausea;
- bloating, heaviness in the abdomen;
- alternating diarrhea and constipation.
When diagnosing and treating acalculous cholecystitis, it is important to tell the doctor about all symptoms, including those that occur at rest, outside of exacerbations.
Diagnostics
Diagnosis of cholelithiasis is based on the clinical picture, as well as data obtained during an instrumental examination. To make a diagnosis with sufficient accuracy, it is enough to perform an ultrasound of the upper abdominal cavity. With its help, you can identify stones in the ducts, gall bladder, determine the size of the bladder, its walls, the condition of the pancreas and liver. Gastroduodenoscopy is also performed to determine the condition of the mucous membrane of the stomach, esophagus and duodenum. If there are complications, retrograde cholangiography or transgastric ultrasound of the bile ducts is prescribed to detect choledocholithiasis.
Percutaneous cholecystostomy
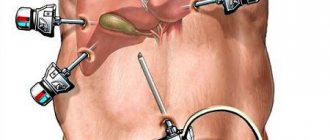
In addition to laparoscopy, there are alternative minimally invasive operations that allow you to preserve the existing bladder. Percutaneous cholecystostomy is indicated for patients with contraindications to laparoscopy. Sometimes the procedure becomes preparation for organ removal.
Under ultrasound guidance, the doctor inserts a thin catheter into the bladder through a puncture in the abdomen. Inflammatory fluid, bile and pus are pumped out of the organ. The catheter allows you to deliver medications directly to the area of inflammation. In emergency cases, the procedure avoids emergency surgery and gives time to prepare for a planned cholecystectomy.
Cholecystostomy can be used as the main method of treatment in patients with contraindications to surgery and people who refuse surgery. The catheter is left in place for the entire duration of treatment. In combination with drug therapy, the method allows you to completely cure cholecystitis.
Treatment
Non-surgical treatment. It is based on diet and medication. Patients with calculous cholecystitis refuse foods that lead to excessive secretion of bile and cause an exacerbation of the disease. Alcohol and carbonated water are completely excluded. The doctor prescribes hepatoprotectors, antispasmodics, enzymes, herbal medicines, antibiotics (if there is an infection). Treatment of chronic calculous cholecystitis is possible with small stones (up to 15 mm), consisting of cholesterol, and normal motor activity of the gallbladder.
Surgical treatment. Treatment is often carried out surgically. As a rule, the entire gallbladder is removed along with the stones. Depending on the indications, access can be carried out either laparoscopically or laparotomically. The operations are performed under general anesthesia.
To make an appointment at the ABC-Medicine clinic to clarify symptoms and treat chronic cholecystitis, call +7.
Therapeutic measures for acute cholecystitis
Exacerbation of cholecystitis requires urgent measures. If surgery is not required, the specialist may recommend the following treatment regimen:
- following a strict diet, avoiding fatty, smoked, spicy foods, alcohol, heavy foods, etc.;
- drug therapy: antibacterial drugs, anti-inflammatory drugs, antispasmodics, medications to normalize the process of secretion and excretion of bile;
- restorative therapy;
- symptomatic treatment: medications to normalize stool, painkillers, etc.
Classification
There are acute and chronic forms, and the course of each of them can be smooth or complicated.
- In the chronic form of calculous cholecystitis, inflammation develops slowly and manifests itself during periods of exacerbation, while the infectious factor no longer plays such a significant role. In the development of calculous cholecystitis, the leading factors are disturbances in the composition of bile, its thickening and stagnation, and irritation of the walls of the bladder. This usually occurs due to errors in nutrition, obesity, diabetes, endocrine changes and frequent infectious diseases. Predisposing factors are biliary dyskinesia, liver disease, chronic gastritis and duodenitis.
- The acute form of calculous cholecystitis occurs rarely; it usually manifests itself as a result of long-term asymptomatic cholelithiasis, in which the walls of the bladder become inflamed due to blockage of the common bile duct by a stone. This happens when infection penetrates into the area of the bladder from surrounding organs due to a violation of the antiseptic properties of bile. As a result, thickening of the walls and their destruction (destruction) quickly develops, which can lead to the accumulation of pus inside the bladder and the formation of biliary peritonitis.
Types of gallstones
Homogeneous (uniform) stones. This group includes cholesterol stones formed due to metabolic disorders. These radioactive formations, which do not cause inflammatory changes in the gallbladder, are most often found in obese patients.
Bilirubin (pigment) stones, which arise as a result of increased breakdown of red blood cells, are characteristic of patients suffering from congenital hemolytic anemia, thalassemia, and sickle anemia. They are also formed in an aseptic environment. Calcareous stones (very rare formations) arise as a result of complications of acute inflammatory processes in the bile ducts.
Mixed stones (this group makes up 80% of the total number of gallstones). The core of such a stone is presented in the form of an organic substance, around which cholesterol, bilirubin and calcium salts are located in layers.
Complex stones (10% of the total). They are a combination of both forms. The core consists of cholesterol, and the shell is a mixture of bilirubin, cholesterol and calcium. As a rule, complex stones are observed with inflammation in the gallbladder and biliary tract.
Forecast
Prognosis for curing the disease largely depends on how it progresses.
Thus, an uncomplicated course of cholecystitis, as a rule, has a favorable prognosis. Complicated forms of the disease, as well as the presence of severe concomitant diseases, lead to a significant deterioration in the prognosis for cure - the mortality rate of patients with these pathologies is 50-60%.
This is explained by the fact that complicated forms of the disease are accompanied by the rapid development of empyema and gangrene of the organ, liver abscesses, fistulas, and peritonitis.
Diet after cholecystectomy
Patients operated on for calculous cholecystitis are prescribed a diet after surgery. In the absence of the gallbladder, which serves as a physiological reservoir, frequent unloading of the biliary tract is necessary. Therefore, the patient is forced to follow fractional meals throughout his entire life. Otherwise, stones may form again in the bubble stump or in the passages themselves. Meals should be at least 5-6 times a day.
After cholecystectomy, there is a deficiency of bile acids responsible for the digestion of fats. Therefore, it is necessary to exclude lard, lamb and beef fat from the menu. The consumption of fatty dairy products and butter should be limited. To compensate for the lack of lipids, more vegetable oil is included in the diet. It can be used to season porridges, salads, and vegetable purees.