It is customary to talk about lipid metabolism disorders in the body if there is an imbalance between the levels of high- and low-density lipoprotein cholesterol, as well as triglycerides. This causes many health problems and leads to the development of serious diseases, including cardiovascular disasters - myocardial infarction and stroke.
The head of the Department of Cardiology and Rheumatology of BelMAPO, Doctor of Medical Sciences, Professor Andrey Pristrom told the journalist of the information portal “Healthy People” about the causes of lipid metabolism disorders, what it entails and how to diagnose the pathology .
Why is cholesterol needed?
Cholesterol is necessary for our body for the functioning of organs and systems. It is part of cell membranes, ensures their strength, participates in the synthesis of sex hormones (androgens and estrogens), as well as those hormones produced by the adrenal glands (cortisol) and in the ovaries (estradiol). Cholesterol plays an important role in the metabolism of fat-soluble vitamins (A, D, E and K). Approximately three-quarters of cholesterol is synthesized in the body and only a quarter comes from food.
Lipoproteins, which are divided into:
- Very low-density lipoproteins (VLDL), which are produced in the liver, contain lipids (triglycerides and cholesterol). They are transported through the blood to the tissues;
- low-density lipoproteins (LDL) are formed from VLDL due to the release of triglycerides from them, contain mainly cholesterol, which is delivered from the liver to the body tissues;
- High-density lipoproteins (HDL) transport unused cholesterol from tissues to the liver, where it is synthesized into bile acids.
Andrey Pristrom: “Lipid metabolism disorders occur due to a breakdown in the mechanism for regulating cholesterol levels. What does it mean? When cholesterol rises, mechanisms must be activated that reduce its formation, and vice versa. There are many reasons that can lead to such an “imbalance.” It’s almost impossible to say unequivocally what exactly triggered the failure.”
Publications in the media
The term atherosclerosis (A) comes from the Greek words athere - gruel, skleros - hard. Atherosclerosis is a chronic disease characterized by fatty infiltration in the intima (inner lining of the arteries) and accompanied by changes in the media (middle layer of the vascular wall).
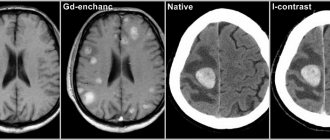
In this case, the arterial wall thickens: due to hyperplasia of smooth muscle cells (an increase in their number), the appearance of fibrous plaques, the formation of a parietal thrombus and platelet adhesion, and the elasticity of the arterial wall decreases and turbulent blood flow occurs in this area of the arteries. Atheromatous plaques protruding into the lumen of blood vessels consist of 25% cholesterol and have a lipid base. Vascular disease, with its effects on the brain, heart, kidneys, and other vital organs, remains a leading cause of morbidity and mortality in many industrialized countries.
The main risk factors causing the occurrence of atherosclerosis are: 1. arterial hypertension; 2. abnormal levels of lipids in the blood serum, as a rule, these are increased levels of low-density lipoproteins (LDL) and low levels of high-density lipoproteins (HDL); 3.diabetes mellitus; 4. burdened heredity, genetically determined, for example, by a deficiency of necessary enzymes - lipoprotein lipase (LPL), lecithin cholesterol acyltransferase and other disorders; 5.age, gender (male predisposition), lifestyle and bad habits: smoking; alcohol consumption; eating fatty foods rich in cholesterol; obesity (due to physical inactivity and excess nutrition).
Atherosclerosis is characterized by an unsystematic course until the development of a critical degree - when the cap of the atheromatous plaque ruptures and a thrombus forms in the damaged area, and occlusion of the lumen of the arteries by the thrombus leads to ischemia, infarction or embolism. The danger of arteriosclerosis increases significantly when the level of cholesterol in the blood plasma is about 7.8 mmol/l (300 mg/100 ml). When the concentration of cholesterol in plasma increases, it is necessary to take into account which transport protein (lipoprotein) it is associated with. Its connection with LDL is considered critical (atherogenic), because LDL transports cholesterol from the liver to the periphery. It is considered harmless when cholesterol binds to HDL, because the latter, on the contrary, transport cholesterol from the periphery to the liver and thereby contribute to its removal not only from the walls of the arteries, but also from the entire body. The regulation of the content of most lipoproteins in the blood plasma is largely regulated by LP receptors, especially LDL receptors of the liver and other tissues.
Cholesterol in the form of esters is deposited in tissues; the majority of esterified cholesterol is found in “foamy” - endothelial cells and macrophages (“foamy” - a cell overloaded with cholesterol and embedded under the endothelial surface of the arteries). A high concentration of non-esterified cholesterol leads to its crystallization; in the crystalline state, cholesterol is found outside the cells. The main task of prevention, treatment of atherosclerosis and prevention of its complications is to reduce the elevated level of atherogenic lipoproteins in the blood plasma - LDL, VLDL, LDLP and increase anti-atherogenic HDL. Treatment begins with the prescription of diet therapy and if it turns out to be ineffective, then they switch to medication.
To achieve the most complete pharmacotherapeutic effect, as part of treatment, drug therapy should be combined with a diet that limits the intake of cholesterol and saturated fatty acids.
Antiatherosclerotic drugs (drugs) are divided into 7 groups.
1. Sequestrants of bile acids (sequestrate – remove). Medicines that increase the excretion of bile acids from the body and reduce the absorption of cholesterol in the intestine. Anion exchange resins - Cholestyramine (Questran), Colestipol (Choletide) and the drug Ezitimib (Ezetrol).
2. Statins are inhibitors of cholesterol synthesis. Drugs that inhibit 3-hydroxy-3-methylglutaryl coenzyme A reductase (HMG-CoA). Lovastatin (Mevacor), Simvastatin (Zocor), Pravastatin (Pravachol), Fluvastatin (Lescol), Atorvastatin (Liprimar), Rosuvastatin (Crestor).
3. Fibrates. Drugs that lower the level of VLDL in the blood and increase the breakdown of cholesterol - Bezafibrate (Holestenorm), Fenofibrate (Grofibrate, Lipantil-200M), Gemfibrozil (Gevilon), Ciprofibrate (Lipanor), Etofibrate (Lipo-Merz).
4. Nicotinic acid and its preparations. Niacin (nicotinic acid, vitamin PP or B3). Preparations – Nicotinic acid, Xanthinol nicotinate, Enduracin, Nicobid.
5. Antioxidants. Drugs that inhibit the early stage of cholesterol biosynthesis and facilitate its transport, reducing the effects of lipid peroxides and free radicals. Medicines – Probucol (Alcolex, Fenbutol).
6. Angioprotectors. Endotheliotropic drugs that reduce cholesterol in the intima of arteries and prevent platelet aggregation. Drugs – Pericarbate (Parmidin, Anginin).
7. Additional drugs. This group includes drugs containing unsaturated fatty acids - Linetol, Lipostabil; plant drugs containing a sum of saponins - Tribusponin, Polysponin; containing vitamins - rosehip and sea buckthorn syrup; garlic preparations - Alisat, Allitera, Allilchep, Allicor and dietary supplements (dietary supplements) - Cholestade, Lysivit S.
Anion exchange resins - cholestyramine, colestipol from the gastrointestinal tract (GIT) are not absorbed and are not destroyed by digestive enzymes. The mechanism of action is the binding of bile acids (necessary for the absorption of dietary cholesterol) in the intestinal lumen with the formation of insoluble compounds due to quaternary ammonium groups. The resulting complex is excreted in excrement. As a result, the enterohepatic recirculation of bile acids is disrupted and enteral cholesterol resorption is reduced.
In the liver, the synthesis of the missing fatty acids necessary for the formation of cholesterol is activated, the number of surface LDL receptors increases and, thereby, the rate of removal of LDL from the plasma increases. Anion exchange resins are started at 1.0 g x 6 times a day and, if well tolerated, the dose is increased to 8.0 g - 24.0 g per day. The level of cholesterol in the blood decreases by 15-20%. The development of serious systemic complications is unlikely, because they are not absorbed. The most common gastrointestinal disorders are: nausea, vomiting - due to unpleasant taste; dyspeptic disorders; constipation With long-term use, it must be remembered that drugs impede the absorption of fat-soluble vitamins and iron, and when used together, they adsorb many drugs.
Ezetrol, when entering the small intestine, prevents the absorption of cholesterol from the intestine by 50%, reduces its content in the liver and increases the removal of cholesterol from the blood. It does not affect the excretion of bile acids and the synthesis of cholesterol in the liver. The drug is prescribed in combination therapy with statins. Side effects are minor: headache, dyspepsia, fatigue.
Statins - these drugs act through competitive inhibition of the enzyme HMG-CoA reductase, thus blocking the conversion of HMG-CoA to mevalonic acid. The ability of drugs to inhibit HMG-CoA reductase for a long time is distributed: lovastatin < simvastatin < fluvastatin < pravastatin < atorvastatin. The potency of the last two drugs increases ~70% due to active metabolites. As a result, the process of formation of cholesterol, necessary for the synthesis of fatty acids in the liver, is inhibited. To compensate for cholesterol deficiency, hepatocytes increase the number of LDL receptors and stimulate the flow of cholesterol from plasma into the liver, reducing its plasma concentration by 30-40% and increasing anti-atherogenic HDL. Lovastatin was isolated from various strains of the fungus; simvastatin, fluvastatin, pravastatin, etc. were obtained semi-synthetically and synthetically. Lovastatin and simvastatin are “prodrugs”, highly lipophilic, in the body the lactone ring opens and they are converted into a β-hydroxy acid, which penetrates well through the blood-brain and placental barriers. In contrast, pravastatin and fluvastatin are hydroxy acids; they are less lipophilic and do not penetrate these barriers. The drug is prescribed once a day in the evening, because Cholesterol is synthesized mainly at night. Doses of drugs - Lovastatin from 20 to 80 mg, simvastatin, fluvastatin, pravastatin 10-40 mg and atorvastatin from 10 mg/day-80 mg. Side effects are typical for all drugs, the most serious are myopathy, hepatotoxicity, allergic manifestations; alopecia, impotence.
Drugs that lower triglyceride levels (VLDL) are divided into 3 groups: fibrates, nicotinic acid and preparations containing fish oil.
Fibrates – increase the activity of endothelial lipoprotein lipase; increase the number of LDL receptors and stimulate the catabolism of LDL and VLDL by the liver, which significantly contributes to their removal from the body; The excretion of bile acids increases and the amount of neutral sterols in the feces increases. Fibrates have a slight effect on cholesterol synthesis. The level of total serum cholesterol in the blood decreases by 15-20% and triglycerides (VLDL) by ~ 30-40%. The main side effects of this group of drugs are gastrointestinal dysfunction - nausea, vomiting, diarrhea, allergic manifestations - itching, urticaria. When using clofibrate, the appearance of gallstones of cholesterol origin was observed; at present, it is used much less frequently. New drugs from the group of fibrates (fenofibrate, gemfibrozil) are less likely to cause side effects and are less toxic.
Nicotinic acid is found in animal organs: liver, kidneys, muscles, etc.; in fish, milk, yeast, vegetables and fruits, buckwheat and other products. The taken dose of nicotinic acid 3.0 g/day provides a drop in cholesterol levels by 10%, triglycerides by 28%, which is due to a decrease in the activity of intracellular lipase, inhibition of lipolysis in adipose tissue, this affects the supply of fatty acids to the liver and a decrease in biosynthesis VLDL, LDL. The level of HDL, which transports atherogenic lipoproteins to the liver, increases and lipoprotein lipase, which destroys them, is activated. Nicotinic acid causes a number of side effects - skin hyperemia, itching, diarrhea, vomiting, liver dysfunction, etc. This drug is undesirable for use in the secondary form of hyperlipidemia caused by diabetes mellitus, because a side effect is hyperglycemia.
Antioxidant - Probucol has moderate activity in reducing serum cholesterol (15%) and has a negligible effect on VLDL levels. However, its mechanism of action is not yet clear enough. It is believed to reduce the absorption of dietary cholesterol, inhibit the early stage of cholesterol biosynthesis, and increase LDL catabolism. Side effects: irritates the gastrointestinal tract; dizziness; angioedema; eosinophilia, thrombocytopenia. Use 0.5 g in the morning and evening with meals.
Endotheliotropic drugs include the angioprotector pericarbate (parmidine), which reduces the permeability of the endothelium to atherogenic lipoproteins. In places where cholesterol is deposited, it promotes the regeneration of elastic and muscle fibers and prevents platelet aggregation. Adverse reactions: minor gastrointestinal disorders, allergic reactions, palpitations. Among the drugs that promote catabolism and cholesterol excretion are polyunsaturated fatty acids (PUFAs) and saponins. PFAs convert cholesterol from esters of insoluble fatty acids into soluble, easily excreted ones, thereby increasing the cholesterol content in bile and excrement and reducing the level of cholesterol in the blood plasma. Side effects: dyspepsia, pain in the gallbladder area. Medicines of plant origin containing saponins delay the absorption of cholesterol in the gastrointestinal tract; a side effect is considered to be dysfunction of the gastrointestinal tract.
In many cases, in the treatment of hyperlipoproteinemia, the most pronounced effect is observed not with monotherapy, but with the combined use of drugs with different mechanisms of action and always in combination with diet therapy.
Reasons for the development of lipid metabolism disorders
Lipid metabolism disorders can be either hereditary or acquired. Among hereditary forms, homozygous and heterozygous disorders are distinguished. The key point in these forms is excessively high levels of low-density lipoprotein cholesterol. This leads to atherosclerotic vascular damage already in childhood and the development of heart and vascular diseases in the second or third decade of life.
Andrey Pristrom: “Persons with homozygous hypercholesterolemia have a very high likelihood of developing cardiovascular accidents (heart attacks and strokes) at 20–30 years of age, and sometimes younger. However, such disorders, compared to heterozygous forms, are quite rare: approximately 1 case per 200–300 thousand population.”
Acquired lipid metabolism disorders are most often diagnosed. Among the risk factors:
- smoking is the most significant risk factor. Smoking damages the vascular endothelium and triggers the development of all disorders. This applies to both active, including electronic devices for tobacco consumption, and passive smoking;
- consumption of large quantities of foods high in saturated fats: red meat, sausages, sausages, hard cheeses, pastries and baked goods;
- obesity;
- inactive lifestyle;
- the presence of concomitant diseases (diabetes mellitus, liver and kidney diseases, arterial hypertension, decreased thyroid function);
- chronic stress;
- age.
Men with lipid metabolism disorders are more likely than women to develop cardiovascular diseases. However, after menopause in women, this indicator levels off in both sexes.
Andrey Pristrom: “More than a third of the male population of our country aged 18 to 44 years have more than 3 risk factors for the development of cardiovascular accidents. Most often these are smoking, obesity, hypertension and high cholesterol.”
Treatment of dyslipidemia
Treatment of dyslipidemia is complex and includes:
- Drug therapy - fibrates, vitamins, statins and other drugs that correct lipid metabolism disorders;
- Non-drug treatment - weight normalization through fractional meals, dosed physical activity, limiting alcohol and smoking, and stressful situations.
- Diet therapy - foods rich in dietary fiber and vitamins are recommended (vegetables, cereals, fruits, beans, low-fat lactic acid products); fatty and fried meats are not allowed.
If lipid imbalance is a secondary pathology resulting from exposure to negative factors or any disease, NEARMEDIC cardiologists prescribe therapy aimed at timely detection and treatment of the underlying disease.
Dyslipidemia develops over years and requires equally long-term treatment. You can prevent further disturbances in lipid metabolism by strictly following the recommendations of doctors: move more, watch your weight, quit bad habits.
Contact your doctors on time!
In the early stages, stopping the pathological process is much easier. Timely therapy, elimination of risk factors and disciplined implementation of doctors’ recommendations significantly prolong and improve the lives of patients
Contact our clinics, do not delay your visit to the doctor. You will be consulted by experienced doctors, and you will undergo an expert examination using high-tech diagnostic equipment. Based on the results obtained, the cardiologist will prescribe competent treatment for dyslipidemia and recommend preventive measures.
To make an appointment with a cardiologist, call or fill out a request on the website.
Diagnostics (lipid profile)
The main method for diagnosing lipid metabolism disorders is the determination of 4 main indicators of lipid metabolism in venous blood (total cholesterol, low and high density lipoproteins, triglycerides), which is called a lipid profile. To make a diagnosis, such an analysis is performed at least twice, one to several weeks apart. Blood is taken on an empty stomach, and it is recommended to avoid a heavy dinner the night before.
If a person is healthy and does not have cardiovascular diseases, diabetes mellitus or serious kidney disorders, the main indicator is total cholesterol. The norm is less than 5 mmol/l.
In the presence of pathologies of the heart and blood vessels, as well as a high risk of their development (determined by the cardiovascular risk scale - SCORE), another control criterion is used: low-density lipoprotein cholesterol.
The target depends directly on the level of risk:
- for low-risk patients – less than 3 mmol/l;
- for patients with moderate risk – less than 2.6 mmol/l;
- for high-risk patients – less than 1.8 mmol/l;
- for patients with a very high risk level - less than 1.4 mmol/l.
The risk of developing cardiovascular accidents is considered high with a score of 5 or more on the SCORE scale.
Elevated levels of LDL cholesterol can cause lipid deposits in the walls of blood vessels, usually in the arteries. It is LDL cholesterol that leads to the appearance of atherosclerotic plaques, which narrow the lumen of blood vessels or completely clog them, thereby blocking the flow of blood.
Andrey Pristrom: “In people with a severe lipid profile disorder, it is also recommended to perform an ultrasound of the brachiocephalic arteries in order to identify atherosclerotic plaques. Atherosclerosis, which develops against the background of lipid metabolism disorders, is a systemic process. If there are changes in the brachiocephalic arteries, then they will be in other vessels.”
The consequences of atherosclerosis are very severe. This is the development of myocardial infarction, stroke, chronic coronary heart disease, occlusion of peripheral arteries, which can lead to amputation of the lower extremities.
Hereditary hypercholesterolemia can be suspected by a blood test: the level of low-density lipoprotein cholesterol will be above 5 mmol/l. In addition, in such people, yellow formations (xanthomas) and white cloudy stripes on the cornea can be seen on the eyelids. Another sign of a hereditary form of lipid metabolism disorders is the appearance of growths on the extensor tendons of the fingers and in the area of the Achilles tendon. In such cases, genetic testing is recommended to confirm or refute hereditary hypercholesterolemia.
The frequency of studies depends on the presence of a risk of cardiovascular accidents. If the risk is low, a blood lipid profile should be performed approximately once every five years; if the risk is high, once a year. However, after 40 years, it is advisable to do a blood test for cholesterol levels annually.
Metabolic disorders: symptoms
Common signs of metabolic failure are:
- Unhealthy skin color.
- Labored breathing.
- Sudden weight gain or loss without objective reasons.
- Joint and muscle pain.
- Deterioration in the quality of hair, nails, skin.
- Thermoregulation disorders (increased sensitivity to cold and heat).
- Sleep problems.
- Changes in blood pressure.
- Edema.
- Prolonged increase or decrease in body temperature.
- Frequent urination.
- Bowel problems: diarrhea or constipation.
- Memory impairment.
- Mood swings.
- Skin rashes.
- Tooth decay.
Symptoms of metabolic disorders in women include infertility and menstrual irregularities (the most common manifestation is scanty discharge).
Also, failures of different types of exchanges may have their own signs, identified by the results of laboratory tests. If carbohydrate metabolism is disturbed, the following may occur:
- Changes in the concentration of glucose in the blood (therefore, a common consequence of a failure of carbohydrate metabolism is diabetes mellitus - a violation of the absorption of glucose).
- Presence of glucose in urine.
Symptoms of lipid metabolism (its disturbance is usually associated with deterioration in the digestion and absorption of fats) are:
- Steatorrhea (presence of lipids in stool).
- Development of cholesterolosis (deposition of cholesterol in cell membranes or on the walls of blood vessels).
Signs of protein metabolism disorders are:
- Content of uric acid in the blood.
- Presence of amino acids in urine.
- Increased bilirubin levels in the blood.