Introduction
Prevalence of Helicobacter pylori
still remains quite high, despite actively carried out eradication therapy.
According to N.V. Zakharova et al., H. pylori
in St. Petersburg is 50% of the total population [1].
On the other hand, eradication of H. pylori
leads to histological remission of chronic gastritis, interrupts the chain of events in the Correa cascade by reducing the activity of the inflammatory process and reducing the severity of atrophy and metaplasia of the gastric mucosa, established histologically in accordance with the OLGA classification (Operative Link for Gastritis Assessment ) or OLGA-IM (OLGA-intestinal metaplasia).
According to M. Kodama et al., the severity of atrophy and intestinal metaplasia decreases significantly 10 years after eradication [2]. A meta-analysis of 16 studies by YJ Kong et al. revealed a significant decrease in the severity of atrophy of the gastric mucosa in the antrum and body of the stomach, as well as intestinal metaplasia in the antrum [3]. Consequently, eradication of H. pylori
has not only a direct effect on reducing and eliminating the inflammatory process in the gastric mucosa, healing the ulcer and preventing the development of relapses and repeated bleeding (both with peptic ulcer disease and with the use of non-steroidal anti-inflammatory drugs against the background of the presence of
H. pylori
), the development of histological remission in the early stages of gastric maltoma, but also leads to good long-term results - a decrease in the severity of atrophy and intestinal metaplasia and ultimately to a decrease in the incidence of cancer of the distal stomach.
This makes it clear how important adequate eradication of H. pylori
is in clinical practice.
According to a Cochrane review, eradication of H. pylori
reduces the incidence of gastric cancer by 34% [4].
Meta-analysis data by YC Lee et al. prove the high effectiveness of H. pylori
in preventing the development of gastric cancer [5].
In Russia, evidence of a decrease in the incidence of cancer of the distal stomach [6, 7] associated with the eradication of H. pylori
.
The enormous importance of H. pylori
is reflected in numerous provisions and recommendations adopted in recent years by medical communities [8–20].
The need to eradicate H. pylori
in all patients infected with this pathogen is consistent with the Kyoto consensus on Helicobacter pylori gastritis, Maastricht V and Houston consensuses [8, 10, 20]. Realities of the 21st century are such that there has been a significant decrease in the effectiveness of previously used anti-Helicobacter regimens, including in Russia. Predictors of low effectiveness of anti-Helicobacter therapy are various factors, the main ones of which are recognized: pathogen resistance, insufficient acid-suppressive effect, low compliance.
Pharmacodynamics and pharmacokinetics
It contains three active components - omeprazole, tinidazole and clarithromycin. The drug has antiulcer and antimicrobial effects. Under the influence of omeprazole, the secretion and acidity of hydrochloric acid decreases (due to the inhibition of a special enzyme located in the membranes of parental cells in the gastric mucosa), and the level of stimulated and basal secretion . Oral administration of omeprazole inhibits the secretion of gastric juice after an hour, the effect persists throughout the day. A 97% reduction in gastric acidity is achieved by repeated administration of 20 mg of omeprazole during the day.
The second component of the drug Pilobact is clarithromycin , a semi-synthetic derivative of erythromycin A, an antibiotic of the macrolide , which acts on Helicobacter pylori , anaerobic microorganisms, gram-negative and gram-positive flora.
The third component of the drug Pilobact is tinidazole ; acts on Giardia, amoebas, Trichomonas , Helicobacter pylori, causative agents of anaerobic infections, and has an antiprotozoal effect.
Pilobact AM additionally contains amoxicillin (an antibiotic). Pilobact NEO is used for triple Helicobacter pylori therapy.
Pilobact and Pilobact AM
Pilobact
(lat.
pylobact
) and
Pilobact ® AM
(lat.
pylobact ® AM
) are combination drugs intended for the treatment of duodenal ulcer associated with
Helicobacter pylori
. According to ATC, both drugs belong to group “A02B. Antiulcer drugs and drugs for the treatment of gastroesophageal reflux”, subgroup “A02BD Combinations of drugs for the eradication of Helicobacter pylori”. The combined active ingredient Pilobact AM - omeprazole + amoxicillin + clarithromycin has a separate code A02BD05. The combined active ingredient of Pilobact is omeprazole + tinidazole + clarithromycin.
Composition of Pilobact AM
Pilobact AM is a set of tablets and capsules:
- enteric capsule containing 20 mg omeprazole
- film-coated tablet containing 500 mg clarithromycin
- capsule containing 500 mg amoxicillin (as trihydrate)
Omeprazole is a proton pump inhibitor that reduces the acidity of gastric juice, ATC code A02BC01.
Clarithromycin is a semisynthetic antibiotic from the macrolide group, ATC code J01FA09. Amoxicillin is a semisynthetic antibiotic from the group of broad-spectrum penicillins, ATC code J01CA04. One set of Pilobact AM corresponds to the daily dose and contains:
- 2 capsules omeprazole 20 mg
- 2 tablets of clarithromycin 500 mg
- 4 capsules amoxicillin 500 mg.
Composition of Pilobact
Pilobact differs from Pilobact AM in that instead of 4 amoxicillin capsules it contains 2 tablets containing 500 mg of tinidazole each. One set of Pilobact corresponds to the daily dose and contains:
- 2 capsules omeprazole 20 mg
- 2 tablets of clarithromycin 500 mg
- 2 tablets of tinidazole 500 mg.
Tinidazole is a synthetic antibacterial agent, ATC code J01XD02.
Indications for use of Pilobact AM and Pilobact
Eradication therapy of Helicobacter pylori
for duodenal ulcer.
Method of use of Pilobact and Pilobact AM and dose
The tablets and capsules included in the Pilobact and Pilobact AM kits are swallowed whole and should not be broken or chewed.
Each kit is intended to be taken within one day. Half in the morning, half in the evening. Tablets and capsules are taken before meals with water. When treating with Pilobact AM, take the following included in the kit at a time: one capsule of omeprazole, one tablet of clarithromine and two capsules of amoxicillin.
When treating with Pilobact, take the following included in the kit at a time: one capsule of omeprazole, one tablet of clarithromine and one tablet of tinidazole.
The duration of the eradication course is one week (seven days).
Professional medical articles concerning the use of Pilobact and Pilobact AM in the treatment of gastrointestinal diseases
- Minushkin O.N., Zverkov I.V., Volodin D.V., Ivanova O.I., Shuleshova A.G. The effectiveness of the drug "Pilobact AM" in eradication therapy of duodenal ulcer // Doctor. – No. 5. – 2008.
- Maev I.V., Samsonov A.A., Andreev D.N., Kochetov S.A., Andreev N.G., Dicheva D.T. Modern aspects of diagnosis and treatment of Helicobacter pylori infection // Medical Council. 2012. No. 8. pp. 10–19.
On the website in the literature catalog there is a section “Helicobacter pylori”, containing articles devoted to gastrointestinal diseases associated with Helicobacter pylori
.
Pharmacological properties of Pilobact and Pilobact AM
Triple therapy, including omeprazole, clarithromycin and amoxicillin (or tinidazole), can achieve a high percentage of Helicobacter pylori
(85-94%). Omeprazole inhibits the secretion of gastric acid due to the specific inhibition of blocking the proton pump (H+/K+-ATPase, an enzyme located in the membranes of the parietal cells of the gastric mucosa. It reduces basal and stimulated secretion, regardless of the nature of the stimulus. After a single dose of the drug orally, the effect of omeprazole occurs during the first hour and continues for 24 hours, the maximum effect is achieved after 2 hours.After stopping the drug, secretory activity is completely restored after 3-5 days.
Amoxicillin is a semi-synthetic penicillin, a broad-spectrum antibiotic due to inhibition of peptidoglycan synthesis during division and growth. Has pronounced activity against Helicobacter pylori
.
Helicobacter pylori
resistance to amoxicillin is rare.
Tinidazole is a synthetic drug whose antimicrobial effect is associated with inhibition of synthesis and disruption of the DNA structure of sensitive microorganisms.
Clarithromycin is an antibiotic from the macrolide group, a semi-synthetic derivative of erythromycin A. It has an antimicrobial effect, which is associated with the suppression of protein synthesis by interaction with the 50S ribosomal subunit of the microbial cell. Effective against a large number of gram-positive, gram-negative aerobic and anaerobic microorganisms, including Helicobacter pylori
.
The metabolite 14-hydroxyclarithromycin formed in the body also has pronounced antimicrobial activity. Combinations of clarithromycin with amoxicillin or tinidazole have a potent antimicrobial effect against Helicobacter pylori
.
Manufacturer of Pilobact and Pilobact AM
— Ranbaxy Laboratories Ltd., India.
Pilobact and Pilobact AM have contraindications, side effects and application features; consultation with a specialist is necessary. Back to section
Contraindications
Pilobact is not prescribed for porphyria , breastfeeding, chronic diseases of the hepatic system, intolerance to active components (omeprazole, tinidazole, clarithromycin, for Pilobact AM - amoxicillin), during pregnancy, severe renal, liver failure, when taking ethanol (the risk of developing disulfiram-like disorders increases). reactions), children under twelve years of age.
Material and methods
A two-center controlled multifactorial study was conducted according to a specially developed protocol in accordance with GCP (Good Clinical Practice) standards. All patients signed informed consent. In the 1st study group (n=201), there were 90 men and 111 women. Age ranged from 18 to 87 years (mean age 47.9±6.9 years). Average height - 168.3±9.5 cm. Body weight - 73.2±11.7 kg. Among the patients, 177 were with H. pylori
- induced chronic gastroduodenitis, 19 - with peptic ulcer, with ulcer localization in the duodenal bulb, 5 - with gastric ulcer.
Patients of the 1st group received a 14-day MPAMOT - the drug Pilobact AM (in accordance with the instructions for this complex drug), which includes omeprazole 20 mg, amoxicillin 1000 mg and clarithromycin 500 mg, 2 times / day and additionally omeprazole 20 mg 2 times a day 30–45 minutes before breakfast and dinner, colloidal bismuth subcitrate (CBS) 240 mg 2 times a day 40–60 minutes after breakfast and dinner for 14 days and a prebiotic complex 5.0 × 2 times. /day 28 days. In group 2 (n=15), patients received SPAMOT - omeprazole 20 mg twice a day, amoxicillin 1000 mg and clarithromycin 500 mg twice a day for 7 days. The compared groups did not have statistically significant differences in age, gender and other criteria, including nosological forms, frequency and severity of symptoms before treatment, which could have affected the results of the study. The rationale for the 14-day course was based on data from a Cochrane meta-analysis assessing the effectiveness of the anti-Helicobacter regimen depending on its duration [31]. H. pylori
eradication rates [32, 33]. A prebiotic complex with fructooligosaccharides, gum arabic, and lactitol was introduced into the anti-Helicobacter regimen.
Diagnosis of H. pylori
carried out using a rapid urease test (Biochit), histologically, and eradication of
H. pylori
after 1 month.
after the end of all medications - by determining the H. pylori
in the stool and a carbon-labeled urease breath test, which corresponded to provisions 20, 21 and 27 of the Houston Consensus on the diagnosis of
H. pylori
in the USA. The fact of eradication was established only if the results of both validated tests were negative.
Side effects
Omeprazole, which is part of Pilobact, can cause headaches, increased gas formation, diarrhea, weakness, dizziness, epigastric pain, constipation, nausea, thrombocytopenia, increased levels of liver enzymes, eosinocytopenia , neutropenia, leukopenia, skin rashes.
Tinidazole can cause cholestatic jaundice , gastralgia, nausea, headache, allergic reaction in the form of itching and rash, pseudomembranous enterocolitis , diarrhea, vomiting, and the development of secondary resistance of microbial flora. Side effects of tinidazole: skin itching, vomiting, leukopenia, unpleasant taste in the mouth, appetite disturbances, headaches, urticaria.
Pilobact, instructions for use (Method and dosage)
The medicine is taken orally.
Each blister contains 2 capsules of omeprazole at a dose of 20 mg, 2 tablets of tinidazole at a dose of 500 mg and 2 tablets of clarithromycin at a dose of 250 mg.
Each blister is designed for 1 day of antiulcer therapy. According to the instructions, you need to take 1 capsule of omeprazole, 1 tablet of tinidazole and 1 tablet of clarithromycin in the morning (the capsule and tablets are located in the orange part of the blister), repeat the procedure in the evening (the capsule and tablets are located in the blue part of the blister).
Each package contains 7 blisters, designed for a weekly course of antiulcer therapy.
After completion of treatment, it is recommended to take omeprazole at a dose of 20 mg per day for three weeks.
Pilobact®
Clarithromycin
When used simultaneously with astemizole, cisapride, pimozide, terfenadine, an increase in the concentration of the latter in the blood was reported, which can lead to cardiac arrhythmias (prolongation of the QT interval on the electrocardiogram, ventricular tachycardia, ventricular fibrillation, torsade de pointes). Concomitant use of clarithromycin with astemizole. cisapride, pimozide, terfenadine are contraindicated.
The simultaneous use of clarithromycin and ergotamine or dihydroergotamine (ergot alkaloids) can lead to acute ergotamine intoxication, accompanied by severe peripheral vasospasm (impaired sensitivity, paresthesia, pain and a marked decrease in pulsation in the extremities, disorders of the central nervous system - dizziness, convulsions, coma). Concomitant use of clarithromycin with ergot alkaloids is contraindicated. Caution should be exercised when using clarithromycin concomitantly with ototoxic drugs, primarily aminoglycosides, due to increased ototoxicity. During and after treatment, the function of the hearing organ and vestibular apparatus should be monitored. Concomitant use of zidovudine in HIV-infected adult patients may result in decreased steady-state zidovudine concentrations. Since clarithromycin affects the absorption of concomitantly administered oral zidovudine, it is recommended that these drugs be taken at least 4 hours apart.
Concomitant use of clarithromycin and digoxin
Digoxin is suspected to be a Pgp substrate. Clarithromycin is known to inhibit Pgp. When clarithromycin and digoxin are used together, inhibition of Pgp by clarithromycin may result in increased effects of digoxin. Post-marketing studies have shown that coadministration of digoxin and clarithromycin may also result in increased serum concentrations of digoxin. Some patients have experienced clinical symptoms of digoxin toxicity, including potentially fatal arrhythmias. Serum digoxin concentrations should be carefully monitored when clarithromycin and digoxin are coadministered.
Interactions caused by
CYP3A CYP3A4
isoenzyme (for example, rifampicin, phenytoin, carbamazepine, phenobarbital, St. John's wort) can induce the metabolism of clarithromycin . This may result in subtherapeutic concentrations of clarithromycin, resulting in reduced effectiveness. In addition, it is necessary to monitor the concentration of the CYP3A isoenzyme inducer in the blood plasma, which may increase due to the inhibition of the CYP3A isoenzyme by clarithromycin. The following drugs have a proven or suspected effect on clarithromycin plasma concentrations; if they are used together, dosage adjustments or switching to alternative treatment may be necessary.
Efavirenz, nevirapine, rifampicin, rifabutin, rifapentine increase the metabolism of clarithromycin, reducing its concentration in the blood plasma and increasing the concentration of its biologically active metabolite 14-hydroxyclarithromycin. In patients receiving inducers of CYP3A isoenzymes, alternative antibiotic therapy options should be considered. The simultaneous use of clarithromycin and rifabutin leads to an increase in the concentration of rifabutin and a decrease in the concentration of clarithromycin in the blood plasma with the risk of developing uveitis.
The concentration of clarithromycin decreases with the use of etravirine, but the concentration of the active metabolite 14-hydroxyclarithromycin increases. Because 14-hydroxyclarithromycin has little activity against Mycobacterium avium complex (MAC) infections, overall activity against Mycobacterium avium complex (MAC) infections may vary and alternative treatments should be considered for the treatment of MAC.
The simultaneous use of fluconazole leads to an increase in the steady-state concentration and area under the curve of “conconcurrent” ventricular tachycardia. Monitoring of ECG (increased QT interval) and serum concentrations of these drugs is necessary. Cases of hypoglycemia have been reported with the combined use of clarithromycin and disopyramide. It is necessary to monitor the concentration of glucose in the blood plasma when using these drugs simultaneously.
Concomitant use with HMG-CoA reductase inhibitors (simvastatin, lovastatin) leads to an increased risk of developing myopathy and rhabdomyolysis. Concomitant use of clarithromycin with simvastatin and lovastatin is contraindicated. Clarithromycin should be used with caution in combination therapy with other statins. If co-administration with statins is necessary, it is necessary to use statins that do not depend on CYP3A metabolism (for example, fluvastatin). It is recommended to take the lowest dose of statin. The development of signs and symptoms of myopathy should be monitored.
When using clarithromycin simultaneously with blockers of “slow” calcium channels that are metabolized by the CYP3A4 isoenzyme (for example, verapamil, amlodipine, diltiazem), caution should be exercised, as there is a risk of arterial hypotension and bradyarrhythmia. Plasma concentrations of clarithromycin, as well as slow calcium channel blockers, may increase with simultaneous use. Arterial hypotension, bradyarrhythmia and lactic acidosis are possible when taking clarithromycin and verapamil simultaneously.
Colchicine is a substrate for both CYP3A and P-glycoprotein, which are inhibited by clarithromycin. A single dose of 0.6 mg colchicine combined with clarithromycin 250 mg twice daily for a week resulted in a 197% increase in the maximum concentration of colchicine and the area under the conconconcontraindications curve. Omeprazole has been shown to interact with some antiretroviral drugs. The mechanisms and clinical significance of these interactions are not always known. An increase in pH during omeprazole therapy may affect the absorption of antiretroviral drugs. Interaction at the level of the CYP2C19 isoenzyme is also possible. When omeprazole is co-administered with certain antiretroviral drugs, such as atazanavir and nelfinavir, a decrease in their serum concentrations is observed during omeprazole therapy. In this regard, the combined use of omeprazole with antiretroviral drugs such as atazanavir and nelfinavir is not recommended.
With the simultaneous use of omeprazole and saquinavir, an increase in the concentration of saquinavir in the serum was noted; when used with some other antiretroviral drugs, their concentration did not change.
Omeprazole inhibits CYP2C19, the main isoenzyme involved in its metabolism. Concomitant use of omeprazole with other drugs metabolized by the CYP2C19 isoenzyme, such as diazepam, warfarin (R-warfarin) or other vitamin K antagonists phenytoin and cilostazol, may lead to a slower metabolism of these drugs. Monitoring of patients taking phenytoin and omeprazole is recommended; a dose reduction of phenytoin may be required. However, concomitant treatment with omeprazole at a daily dose of 20 mg does not affect the concentration of phenytoin in the blood plasma in patients taking the drug for a long time. When using omeprazole in patients receiving warfarin or other vitamin K antagonists, monitoring of the international normalized ratio is necessary; in some cases, it may be necessary to reduce the dose of warfarin or another vitamin K antagonist. At the same time, concomitant treatment with omeprazole at a daily dose of 20 mg does not lead to a change in coagulation time in patients taking warfarin for a long time.
The use of omeprazole at a dose of 40 mg once daily resulted in an increase in Cmax and AUC of cilostazol by 18% and 26%, respectively; for one of the active metabolites of cilostazol, the increase was 29% and 69%, respectively.
According to the study results, a pharmacokinetic/pharmacodynamic interaction was noted between clopidogrel (loading dose of 300 mg and maintenance dose of 75 mg/day) and omeprazole (80 mg/day orally), which leads to a decrease in exposure to the active metabolite of clopidogrel by an average of 46 % and reducing the maximum inhibition of ADP-induced platelet aggregation by an average of 16%.
The clinical significance of this interaction is unclear. An increased risk of cardiovascular events with concomitant use of clopidogrel and proton pump inhibitors, including omeprazole, was not shown in a prospective, randomized, open-label study of more than 3,760 patients receiving placebo or omeprazole 20 mg/day. concomitantly with clopidogrel and acetylsalicylic acid (ASA) therapy, and was not confirmed by additional non-randomized analysis of clinical outcomes from large prospective randomized trials involving more than 47,000 patients.
The results of a number of observational studies are contradictory and do not provide a clear answer about the presence or absence of an increased risk of thromboembolic cardiovascular complications during the combined use of clopidogrel and proton pump inhibitors.
When clopidogrel was used together with a fixed combination of 20 mg esomeprazole and 81 mg ASA, exposure to the active metabolite of clopidogrel decreased by almost 40% compared with clopidogrel monotherapy, while the maximum levels of inhibition of ADP-induced platelet aggregation were the same, which is likely due to simultaneous taking ASA in a low dose.
Omeprazole does not affect the metabolism of drugs metabolized by the CYP3A4 isoenzyme. such as cyclosporine, lidocaine, quinidine, estradiol, erythromycin and budesonide.
No interaction of omeprazole with the following drugs has been identified: antacids, caffeine, theophylline, S-warfarin, piroxicam, diclofenac, naproxen, metoprolol, propranolol and ethanol.
With the simultaneous use of omeprazole and tacrolimus, an increase in the concentration of tacrolimus in the blood serum was noted.
Some patients experienced a slight increase in methotrexate concentrations when combined with proton pump inhibitors. If high doses of methotrexate are prescribed, temporary discontinuation of omeprazole should be considered.
Effect of drugs on the pharmacokinetics of omeprazole
The isoenzymes CYP2C19 and CYP3A4 are involved in the metabolism of omeprazole. Concomitant use of omeprazole and inhibitors of CYP2C19 and CYP3A4 isoenzymes. such as clarithromycin and voriconazole, may lead to increased plasma concentrations of omeprazole by slowing the metabolism of omeprazole. Concomitant use of voriconazole and omeprazole results in a more than twofold increase in the AUC of omeprazole. Due to the good tolerance of high doses of omeprazole, short-term joint use of these drugs does not require dose adjustment of omeprazole.
Co-administration of omeprazole with amoxicillin or metronidazole does not affect the concentration of omeprazole in the blood plasma.
Drugs that induce CYP2C19 and CYP3A4 isoenzymes. such as rifampicin and St. John's wort preparations, when used together with omeprazole, can lead to a decrease in the concentration of omeprazole in the blood plasma by accelerating the metabolism of omeprazole.
Tinidazole
Tinidazole enhances the effect of indirect anticoagulants and the effect of ethanol - disulfiram-like reactions are possible. Compatible with sulfonamides and antibiotics (aminoglycosides, erythromycin, rifampicin, cephalosporins). It is not recommended to administer together with ethionamide. Phenobarbital accelerates the metabolism of tinidazole.
Interaction
Clarithromycin, which is part of the drug Pilobact, can cause an increase in the level of theophylline and terfenadine in the blood (a prolongation of the QT interval is recorded on the ECG).
An enhanced effect of the drug is observed with simultaneous therapy with oral forms of anticoagulants .
When treated with digoxin, astemizole, phenytoin, carbamazepine, cisapride , pimozide, valproate, Lovastatin , disopyramide, cyclosporine , an increase in the concentration of the above drugs is observed.
Omeprazole can reduce the rate of metabolic processes when taking diazepam and phenytoin.
Pilobact reduces the absorption of iron salts (reducing acid production in the stomach), ampicillin, ketoconazole .
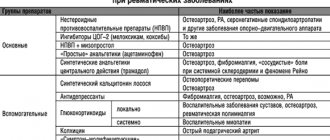
Methods for increasing the effectiveness of anti-Helicobacter therapy:
Targeted therapy taking into account bacterial resistance and genotypic polymorphism of CYP2C19, individualized anti-Helicobacter therapy taking into account the characteristics of micro- and macroorganisms.
Increasing the duration, frequency of administration or dose of components of the anti-Helicobacter regimen.
Use of double doses of proton pump inhibitors (PPIs). The use of new, stronger acid-suppressive drugs (K-competitive proton pump blockers - vonoprazan), control of acid production during the anti-Helicobacter regimen and maintaining it at a certain level.
The use of 3 antibacterial drugs simultaneously and the use of new antibacterial drugs, the use of natural antibiotics (pyloricidin A, B and C), natural antimicrobial peptides (cathelicidins and defensins), benzimidazole derivatives, polycyclic components.
Combination of anti-Helicobacter therapy and sanitation of the oral cavity (elimination of gingivitis, periodontitis, etc.).
Effect on H. pylori
(acetylcysteine, proteinase complex,
quorum sensing
, silver nanoparticles, nanoemulsions, lactoferrin, etc.), adjuvant use of probiotics, prebiotics or metabiotics.
Inclusion of rebamipide, pyridodiazepines, and sulfonamides into the treatment regimen.
Herbal medicine (ginger rhizome extract, red and chili pepper (capsaicin), broccoli (sulforaphane), red ginseng extract, green tea, St. John's wort, cloves), grapes, cranberry juice, curcumin, concentrated honey solution, red wine (resveratrol), vitamin supplements (vitamins C and E).
The use of special gastric drug delivery systems (gastro retentive drug delivery sestems - GRDDS), micro- and nanoparticles of various drugs.
It can be assumed that increasing the duration of the Pilobact AM-based anti-Helicobacter regimen from 7 to 14 days, increasing the dose of omeprazole from 40 mg/day to 80 mg/day and including bismuth in the colloidal subcitrate with the adjuvant use of a prebiotic complex will lead to a significant increase in H2 pylori
without increasing the number of adverse events.
All of the above served as the basis for studying the effectiveness of modified Pilobact AM-based therapy (MPAMOT) for the eradication of H. pylori
.
The introduction of a prebiotic complex into the anti-Helicobacter regimen can also increase the effectiveness of treatment [22–30]. The prebiotic complex selectively stimulates the growth and/or activity of a limited number of microbiota bacteria; prebiotics are resistant to the digestive process in the upper gastrointestinal tract, are fermented by intestinal microbiota, and have a proven synergistic effect on the intestinal microflora [22]. Prebiotics are well tolerated, act throughout the colon, have an anti-infective effect (due to the synthesis of propionate), and are highly effective [23–27]. The effect of the prebiotic does not depend on the viability of the culture, while its own microflora is maintained and not colonized by foreign ones. Probiotics create a positive effect in dysbiosis, but not always and not as expected [28]. Every second person who uses a probiotic exhibits antagonistic properties towards host microorganisms; biocompatibility - 15% [29].
Purpose of the study:
determine the effectiveness of MPAMOT in patients infected with
H. pylori
.
To achieve the intended goal, the following tasks are set:
Assess the eradication rates of H. pylori
in all patients included in the study.
Assess the eradication rates of H. pylori
in all patients undergoing treatment.
Assess the incidence of adverse events among all patients included in the study (intention to treat - ITT) and all patients undergoing treatment ( per protocol
- PP).
To compare MPAMOT with standard 7-day Pilobact AM-based therapy (SPAMOT) and targeted anti-Helicobacter therapy.
To assess the frequency of adverse events (diarrhea, nausea, abdominal discomfort, taste changes) with MPAMOT and SPAMOT.
special instructions
Tinidazole may cause urine to turn dark.
Throughout the entire course of antiulcer therapy, complete abstinence from drinking alcoholic beverages is required due to the risk of developing disulfiram-like reactions .
In case of chronic pathology of the hepatic system, periodic monitoring of the level of liver enzymes is mandatory.
Before starting therapy, the attending physician must exclude the presence of malignant neoplasms (taking omeprazole may mask the clinical manifestations of cancer).
Pilobact price, where to buy
The price of Pilobact is approximately 1250 rubles per set.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Pilobact combination set n42 (6 pcs x 7 blister)SUN Pharmaceutikal Industries Ltd.
RUB 1,176 order - Pilobact am combination set n56 (8 pcs x 7 strips) SUN Pharmaceutikal Industries Ltd.
RUB 1,289 order
Pharmacy Dialogue
- Pilobact combined set (set No. 7)Ranbaxy
RUB 1,268 order
- Pilobact combiner AM (set No. 7)Ranbaxy
RUB 1,312 order
show more
Pharmacy24
- Pilobact NEO N42 set of tablets Sun Pharmaceutical Industries Ltd, India
464 UAH.order
PaniPharmacy
- Pilobact neo tablets Pilobact Neo comb. table No. 42 India, SUN
476 UAH. order
show more