Stages of disease development
The pathogenesis of a brain abscess involves four stages of its development:
- Early brain inflammation (1-3 days). The patient develops encephalitis, a limited inflammation of brain tissue. The important thing is that at this stage it is still quite possible to reverse the disease. The inflammatory process can end spontaneously or upon completion of antibacterial therapy.
- Late stage (4-9 days). This stage occurs when the protective functions of the patient’s body are weakened or due to incorrectly chosen treatment tactics. Therefore, the inflammation begins to progress - the cavity filled with pus begins to increase in size.
- Early encapsulation (10-13 days). This stage of inflammation is characterized by necrosis of the central part of the brain, as well as the formation of a capsule that limits the further spread of pus.
- Late encapsulation (starting from day 14). Starting from the second week after activation of the inflammatory process, the patient is diagnosed with a clear collagen capsule filled with pus and surrounded by a zone of gliosis. The further development of inflammation depends on the reactivity of the patient’s body, the virulence of the flora, and proper treatment. Often at this stage there is an increase in the volume of purulent content and the formation of new foci of inflammation.
Types of disease
Most often in the clinic there are contact abscesses caused by otitis, mastoiditis, suppuration in the nasal cavities, meninges, orbit or skull bones.
- Otogenic. Occurs in most cases. An abscess is more often complicated by chronic purulent otitis than by an acute process. In the case of otitis media, the infection enters the brain from the temporal bone through the cavernous sinuses and the roof of the tympanic cavity into the middle fossa of the skull, resulting in inflammation of the brain in the temporal lobe of the brain. An infection of otogenic origin can also penetrate into the posterior cranial fossa, passing through the labyrinth and then the sigmoid sinus, which is why a cerebellar abscess occurs.
- Rhinogenic. Often concentrated in the frontal parts of the brain. First, it is caused by local pachymeningitis, after which it passes into the stage of adhesive limited meningitis and ultimately this process ends with the formation of limited purulent encephalitis in the brain tissue. It is very rare that rhinogenic and otogenic types of disease manifest themselves hematogenously as a result of sinuses, venous thrombosis or septic arteritis. In this case, the abscesses are concentrated deep in the brain.
- Traumatic. Often occur during open skull trauma. If the dura mater is damaged, the infection enters the brain tissue through the perivascular gaps. If a foreign body enters the brain, the infection enters along with it. Nowadays, traumatic abscesses reach 15% of all possible types of this disease.
- Metastatic. Often occurs as a result of lung diseases such as pleural empyema, pneumonia (pneumonia) or bronchiectasis. Such abscesses are accompanied by the penetration of infection into the brain by septic embolism. About 30% of metastatic abscess diseases are multiple and form in the deep parts of the white matter of the brain.
General cerebral symptoms
General cerebral symptoms arise due to sudden jumps in intracranial pressure. The most common symptom of the pathology is headache accompanied by vomiting. The patient may experience problems with vision: often, against the background of an abscess, optic neuritis develops, and congestive discs appear in the fundus. The clinical picture of the disease also includes mental disorders, inhibition of thought processes, lethargy, weakness, and apathy. In the case of intracranial hypertension, epileptic seizures may occur. Most patients also experience persistent drowsiness, and in the most severe cases, coma may occur.
Symptoms
As mentioned above, the complaints of patients with this disease often correspond to the clinic of any extensive formation. A person may experience a wide range of symptoms, ranging from pain in the head to cramps. In many ways, the manifestations of the disease depend on its location.
Let us consider in more detail what complaints arise at various stages of pathology.
The onset of the disease is usually characterized by general intoxication and cerebral syndromes. A person develops a fever, chills, weakness and fatigue. Patients experience severe headache, dizziness, nausea, vomiting, and fainting may occur. At this stage of the disease, the purulent cavity has not yet formed, so the changes are reversible. If the pathogen is highly virulent, the brain tissue melts, forming a cavity with an accumulation of pus, which over time becomes overgrown with a capsule. After 5-6 weeks, when the process of formation of a brain abscess is completed, the patient’s condition often improves.
Frequent headaches
Subsequently, focal neurological symptoms gradually increase. Based on complaints that arise at this stage, one can assume the localization of the pathological process. The clinical picture can be similar to a stroke (if the left half of the body is paralyzed, there is a pathological focus in the right hemisphere and vice versa) or a mass formation in the occipital lobe (visual impairment).
Course of a brain abscess
As for the course of the disease, it often has a very violent and acute onset, which is characterized by focal and hypertensive manifestations. The inflammatory process almost always develops against a background of elevated temperature. In rare cases, the onset of the disease may be less pronounced and resemble the clinical picture of meningitis. However, with minimal symptoms and normal temperature, the first stage of the disease is extremely rare.
After 5-30 days, the disease passes into the next, latent, stage, which is characterized by either a complete absence of any symptoms, or minimally expressed signs of the disease. The patient may complain of severe and regular headaches, mental retardation and vomiting. The duration of this stage varies: in some patients it lasts a couple of days, while in others it lasts several years. Then, due to the influence of some factor (for example, infection), this stage ends and the patient’s symptoms begin to actively progress. The most severe and life-threatening consequence of a brain abscess is its rupture, which usually leads to death.
Symptoms
Any degenerative processes in the brain cause similar symptoms and signs, especially in the initial stages of occurrence. In the first stages, the patient may only be bothered by headaches and dizziness. Next, attacks similar to epileptic syndrome occur. As the lesion grows, symptoms of an oncological or benign formation appear. Since adjacent tissues are subject to displacement and compression, depression of consciousness and cognitive abilities occurs. Over time, the signs intensify and are complemented by more and more new symptoms.
Diagnosis of brain abscess
Timely comprehensive diagnosis of brain abscess is important in its further treatment. To make a diagnosis, a neurologist uses medical history and examination results of the patient, as well as information obtained during instrumental and laboratory tests. The following methods are used to diagnose the disease:
- General blood analysis. The disease is usually indicated by test results such as an increase in ESR and pronounced leukocytosis. At the stage of capsule formation around the abscess, a normal or slightly increased number of leukocytes is observed in the patient’s blood.
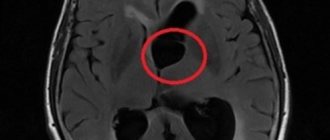
- CT scan. The accuracy of detecting an abscess using this technique depends on the stage of the pathology. In the early stages, an abscess is very difficult to detect. At the stage of encephalitis, CT may reveal an area of reduced density that has an uneven shape. At this stage, the contrast agent accumulates unevenly - often only in the peripheral areas. It is much more accurate to diagnose the disease at a late stage in the development of encephalitis.
- Magnetic resonance imaging. This is a more accurate and effective method of diagnosing an abscess, which allows it to be detected at an early stage. Since the technique is considered the most informative, treatment can be prescribed based on its results even without bacteriological tests.
- Echoencephaloscopy. This diagnostic method is usually prescribed if for some reason MRI and CT cannot be performed. Using this study, it is possible to detect displacement of brain structures, which indicates compression of its tissues by an abscess.
- Bacteriological research. This technique involves taking a puncture of pus from the abscess for examination. A detailed examination of the pus helps to identify the causative agent of inflammation, which then makes it possible to select the most appropriate tactics of drug therapy.
- X-ray of the skull. This technique is used to detect the source of infection that caused the abscess.
- Craniography. Prescribed to detect symptoms of intracranial hypertension.
Causes
This pathological process is always secondary, i.e. is a complication of another disease, and not the primary lesion. Infection can enter the cranial cavity in several ways:
- With blood flow.
- As a result of the spread of infection from the maxillary sinuses, inner ear, etc.
- Due to an open craniocerebral injury.
- Due to wound infection after surgery.
In the first case, the site of development of pathology most often is the organs of the respiratory system or the heart (bacterial endocarditis, pleural empyema, etc.). The infection penetrates the main organ of the nervous system with the help of a blood clot, which breaks off from the vessel wall at the site of primary inflammation. Next, the bacteria settle in the small vessels of the brain and begin to infect healthy cells and tissues.
With frontal sinusitis, sinusitis and sinusitis, the pathological process can spread in two ways: through the sinuses and veins of the dura mater of the brain or directly through it. In the second option, inflammation first develops in the meninges, and then spreads to the tissues adjacent to them.
Brain abscess in traumatic brain injury is associated with direct entry of bacteria into the skull as a result of a violation of its integrity. The number of such cases in peacetime reaches only 10-15% of the total incidence of this pathology. After neurosurgical operations, focal accumulation of pus in the brain tissue occurs only in people with low immunity or in severely ill patients.
As for the pathogens that cause the development of such pathology, most often cultures indicate the presence of the following microorganisms:
- Streptococci.
- Staphylococci.
- Proteas.
- Aspergillus.
- Bacterioids.
However, isolation of the pathogen is not always successful. Thus, in 20-25% of cases, the contents of the abscess remain sterile during culture.
Important! In order for such a pathology to develop, the presence of two factors is always necessary: high virulence (ability to infect) of the infectious agent and a decrease in the body’s defenses.
Differential diagnosis of brain abscess
Since the majority of symptoms of brain abscess are not specific, differential diagnosis plays an important role. If the doctor has doubts during diagnosis, he may prescribe MR spectroscopy. This technique is carried out in order to differentiate a brain abscess from tumors of the cerebral hemispheres. It is based on different contents of lactate and amino acids in tumors and purulent accumulations.
As for other diagnostic methods, they are considered less informative. For example, signs such as an increase in C-reactive protein in the blood, chills, an increase in ESR, and leukocytosis may indicate a variety of inflammatory processes. Blood cultures from an abscess are often sterile.
Clinical picture
The clinical picture depends on the location of the abscess and its size, the stage of development of the pathological process, and the reaction of surrounding tissues.
There are 4 stages during the disease: initial, latent, overt and terminal. The initial stage lasts one to two weeks and is called the encephalic stage of brain abscess. It is characterized by symptoms such as lethargy, high body temperature, headache, nausea and vomiting.
The duration of the latent stage is on average 2 weeks. It is characterized by 4 groups of symptoms.
The first group includes manifestations that are characteristic of suppurative processes: lack of appetite, lethargy, stool retention, bad breath, exhaustion, “coated” tongue, changes in the composition of the blood characteristic of the inflammatory process.
Make an appointment right now!
Call us by phone or use the feedback form
Sign up
The second group includes general cerebral symptoms: headache, bradycardia (decrease in heart rate below 60 beats), stiff neck, positive Kernig and Brudzinski symptoms.
The third group presents symptoms of disturbances in the activity of conduction systems and subcortical nuclei: hemiparesis (paresis of one half of the body) and hemiparalysis, paresis of the facial nerve of the central type, convulsive seizures, paresis of the oculomotor nerve, pyramidal symptoms (Babinsky, Oppeheim, etc.).
The fourth group of symptoms is very important for determining the localization of the process and reflects cluster symptoms. If amnestic and sensory aphasia (speech disorder) appears in right-handed patients, this indicates that the abscess is localized in the left temporal lobe of the brain. If patients experience ataxia (impaired coordination of movements) and dizziness, then most likely the abscess is located in the right temporal lobe and spreads to the pathway that connects the right temporal lobe and the left cerebellum. Mental disorders of an emotional and personal nature may also be observed, which are manifested by euphoria or a depressive state, lack of a critical attitude towards one’s illness, psychomotor agitation, negativism (opposition and contradiction to other people). When the right temporal lobe is affected, an important symptom is a violation of the visual fields - hemianosmia, with loss of the same halves of vision in each eye.
Friends! Timely and correct treatment will ensure you a speedy recovery!
With a cerebellar abscess, there is a decrease in muscle tone on the affected side. The main symptom is ataxia, which is usually detected when walking and performing coordination tests (digital-digital, finger-to-digital, digital-to-digital, adiadochokinesis (inability to perform rapid, alternating movements), study in the Romberg position). Falls and misses on the part of the affected cerebellum are characteristic. Very indicative is nystagmus (involuntary movement of the eyeballs), directed upward and in both directions, often multiple.
A blood test reveals moderate neutrophilic leukocytosis and increased ESR. With an uncomplicated abscess, cerebrospinal fluid leaks under high pressure. Most often it is light and has a moderate shift: slight pleocytosis (increase in the number of cells) to a level of 100-200 cells in 1 μl. and a moderate increase in protein. If an abscess breaks into the subarachnoid space, the cerebrospinal fluid becomes purulent. With a cerebellar abscess, when taking a spinal tap, the fluid must be released slowly and in small portions to avoid wedging the brain stem into the foramen magnum.
At the terminal stage of development of the disease, dislocation symptoms manifest themselves: anisocoria (unequal pupil sizes), limited gaze, impaired breathing rhythm, loss of consciousness. The duration of this stage of abscess of the brain and cerebellum is several days and ends with the death of the patient. In this case, there is increasing swelling of the brain, paralysis of centers of vital importance, or an abscess breaking into the ventricles of the brain. Quite rarely, the breakthrough of an abscess into the ventricles of the brain and purulent ventriculitis (inflammation of the ventricles of the brain) result in a favorable outcome.
Treatment of brain abscess
Treatment for a brain abscess usually involves both drug therapy and surgery. Doctors select the most optimal treatment tactics based on the results of diagnosing the disease, as well as the general health of the patient. The stage of the disease is also taken into account. For example, in the early stages of abscess formation, conservative treatment can be used. If an abscess has already formed, and a dense capsule has formed around it, neurosurgical intervention cannot be avoided.
- Drug treatment
- Surgery
Drug treatment of brain abscess involves the prescription of antibiotics, decongestants and anticonvulsants. Since the inflammatory process is provoked by bacteria, treatment of the disease necessarily involves their destruction. The combination of penicillin and chloramphenicol has been considered the most standard and commonly used treatment regimen for brain abscess for decades.
Penicillin was prescribed to treat the disease because it can kill streptococci and most other bacteria that can cause brain abscess. Chloramphenicol was used because of its ability to easily dissolve in adipose tissue and destroy anaerobic bacteria.
Today doctors are slightly adjusting this scheme. For example, cefotaxime is prescribed instead of penicillin, and metronidazole is prescribed instead of chloramphenicol. Typically, the doctor prescribes antibiotic therapy several weeks before surgery. The duration of taking antibiotics can be about 6-8 weeks.
Patients whose brain abscess occurs due to immunodeficiency are also prescribed amphoreticin. If the abscess has resolved, the patient will need to take a course of fluconazole for ten weeks. Drugs such as sulfadiazine and pyrimethamine are commonly included in the treatment regimen of patients with HIV.
Of great importance in the treatment of the disease is the correct identification of the causative agent of infection using an antibiogram. However, there are cases when the culture turns out to be completely sterile. Therefore, in such situations, empirical antibiotic therapy is prescribed.
In addition to antibiotics, medications are also prescribed to help reduce swelling. For example, glucocorticoids are used for this purpose. However, the prescription of these drugs is indicated only in case of a positive result from antibacterial therapy. They can reduce the severity of a brain abscess and reverse the development of the capsule around it. However, the opposite effect is also possible, when glucocorticoids activate the spread of inflammation beyond the boundaries of the lesion. To eliminate convulsive manifestations, phenytoin is usually prescribed.
If a brain abscess is diagnosed in the late stages, and a dense capsule has already formed around it, it is impossible to do without surgery. To treat the disease, puncture aspiration and removal of the abscess are most often used.
As for puncture aspiration, it is advisable to prescribe it in the early stages of the pathology. In this case, antibacterial therapy should be carried out simultaneously. Indications for this procedure may also include multiple abscesses, a deep location of the abscess, the stage of cerebritis and a stable neurological condition of the patient. To ensure that the procedure is performed as accurately as possible, the doctor resorts to stereotactic biopsy and intraoperative ultrasound.
Needle aspiration has one important drawback - in most cases, a repeat procedure may be required after it is performed. In difficult cases, complete removal of the abscess is prescribed. This technique is also prescribed if they want to avoid a possible relapse of the disease. It is advisable to remove an abscess for the following indications: if antibacterial therapy or puncture aspiration are not effective, with a superficial abscess and a well-formed capsule around it.
If multiple abscesses were discovered in a patient during diagnosis, then first you need to drain the inflammation to prevent pus from breaking into the ventricular system of the brain. If neurological disorders increase or there is no positive dynamics on MRI and CT, a repeat operation may be prescribed.
Therapeutic measures
At the precapsular stage, as well as with a small diameter of the intracerebral “bubble” (up to three centimeters), traditional treatment based on taking antibiotics is carried out. When it is difficult to determine the nature of microorganisms, it is recommended to take a purulent substance for biophysical examination. Next, specific antibacterial drugs are prescribed.
Deep lesions, growing, and also located in close proximity to the ventricles of the brain are a direct indication for emergency surgery. The affected areas must be immediately removed, since the entry of purulent fluid into the ventricles is fraught with subsequent death for the patient. If the cause of the disease is fungi, surgical treatment is also recommended.
Surgical treatment is completely contraindicated in cases where the neoplasm is located in vital parts of the organ:
- area responsible for visual function;
- brain stem;
- nuclei under the cortex.
In this case, a low-traumatic puncture penetration is carried out, when the cavity is opened, the contents are emptied, the internal area is cleaned with sterilizing solutions, and filled with antibacterial agents. This procedure can be performed repeatedly through an installed catheter. Partial surgery does not require putting the patient into medicated sleep; local anesthesia is sufficient. A contraindication to any surgical treatment is the person’s extremely serious condition, shock or comatose loss of consciousness. If the disease is large-scale and has multiple foci of inflammation, drainage must begin from the most dangerous areas that threaten subsequent critical complications, as well as from the largest capsules.
Prognosis for brain abscess
The outcome of the disease depends on whether the doctor was able to identify the causative agent of the abscess from culture. It is extremely important to do this, since then it will be possible to determine the sensitivity of bacteria to antibiotics and select the most appropriate treatment regimen. The prognosis for the health of a patient with a brain abscess also depends on the number of purulent accumulations, the patient’s health status, and the correct treatment tactics.
The risk of various complications with a brain abscess is very high. Namely, about 10% of all cases of the disease end in death, and 50% result in disability. In addition, most patients may develop epileptic syndrome after treatment, a condition characterized by the occurrence of epileptic seizures.
Doctors give less favorable prognoses to patients who have been diagnosed with subdural empyema. In this case, the patient does not have a clear boundary of the purulent focus due to the high activity of the infectious agent or the body’s insufficient resistance to it. Lethal cases with subdural empyema reach 50%.
The most dangerous form of brain abscess is considered to be fungal empyema, which is accompanied by immunodeficiency. This disease has practically no cure, and the number of deaths with it is about 95%. In turn, epidural empyemas have a more favorable prognosis and are almost never accompanied by complications.
Pathogenesis: how does the process develop?
The development of the disease consists of 4 separate stages, or stages:
- The first stage is early infiltration. During the first 3 days after entry of the pathogenic agent, a poorly demarcated diffuse focus of inflammation is formed with destruction of brain tissue and swelling around it.
- The second stage is late cerebritis. The center of focal inflammation undergoes suppuration and necrotization on days 4-9, which is accompanied by the formation of a cavity. The cavity is filled with semi-liquid purulent exudate. Fibroblasts accumulate along the outer part.
- The third stage is the formation of the gliosis capsule. From 10-13 days the protective capsule of the abscess begins to form. Thus, there is an intensification of the growth of the layer of fibroblasts bordered by a rim of neovascularization. Along with this, reactive astrorcytosis is noted.
- The last stage (4th stage) is the final formation of the capsule. The capsular component around the filled purulent cavity is fully compacted (reactive collagen takes part in this). The necrotic focus takes on clear outlines.
Further processes at the last stage depend on the virulence of the pathogenic flora, the route of spread, the immune status of the patient, and the level of hypoxia of the affected brain structures. The correctness of diagnostic and therapeutic measures will no less affect the degree of progression of AGM. As a rule, the disease cannot regress on its own. Without adequate therapy, in the vast majority of cases, the internal volume of the abscess increases, and the appearance of new infected areas along the periphery of the capsule cannot be ruled out.
Prevention of brain abscess
There are no effective methods for preventing brain abscess. However, with the help of several preventive measures, the risk of the disease can be significantly reduced. In particular, in the case of traumatic brain injury, the patient must receive adequate surgical care.
The disease can also be prevented by timely elimination of foci of infection (pneumonia, boils), treatment of purulent processes in the inner and middle ear, as well as the paranasal sinuses. Good nutrition also plays a great role in the prevention of brain abscess.
Treatment
Therapy for the disease must be comprehensive. Most often, surgical intervention is used in combination with adequate combination antibacterial therapy. Antibacterial therapy can last several weeks. Subsequently, a long period of rehabilitation is required. Depending on the resulting neurological defect, one should resort to neuroprotective therapy, massage, exercise therapy, and sometimes, when symptomatic epilepsy develops, the selection of antiepileptic drugs is necessary.