General information
Encephalopathy occurs due to metabolic disorders in brain cells. Regardless of the cause, the pathology follows a single scenario. First, there is a decrease in the activity of neurons, then their gradual death. Foci of dystrophy are located throughout the brain, which causes a variety of symptoms.
The damage is irreversible, but with timely consultation with a specialist and quality treatment, the patient’s condition can improve. The remaining intact neurons partially take over the function of the dead cells, and brain function is significantly improved. If the disease was caught at an early stage, the patient retains complete clarity of mind.
Make an appointment
Prevention of vascular diseases of the brain
Vascular diseases of the brain are easier to prevent than to cure. To do this, experts recommend leading a healthy lifestyle: engaging in moderate sports, drinking about 1-1.5 liters of water per day (to avoid dehydration), eating properly and following a diet. The diet involves limiting table salt and foods containing large amounts of animal fats (for example, sour cream and fatty meats). Fresh vegetables and fruits should prevail in the daily diet. A split diet is recommended (4-5 meals per day).
The intake of alcoholic beverages should be minimized (or completely abandoned). The emotional component is the key to good health, so you should not be exposed to stressful situations. Sleep should be complete (at least 7 hours of sleep per day are required). Moderate physical activity should be regular; it significantly improves the condition of the body. These include: swimming, yoga, Pilates, cycling.
Exercising and proper nutrition help prevent the appearance of excess weight, while they train the cardiovascular system. At least once a year it is required to undergo a study of the state of cerebral circulation (especially for those who are at risk). This will allow timely detection of pathology.
In order to prevent the progression of multi-infarction conditions, patients are prescribed combination therapy (antiplatelet and anticoagulant). The most suitable anticoagulants are selected depending on blood clotting parameters. If any signs of bleeding appear, it is important to contact a specialist promptly.
Vascular diseases of the brain are often accompanied by dizziness. To prevent them, doctors prescribe medications that affect the autonomic nervous system. To prevent cognitive impairment (memory deterioration, increased inattention), drugs that improve metabolism are prescribed. In the presence of movement disorders, therapeutic exercises, physiotherapy, massage and other methods of rehabilitation therapy are useful.
Causes
Damage to nerve cells can occur due to exposure to various pathological factors.
- previous trauma;
- acute or chronic intoxication with salts of heavy metals, narcotic substances, alcohol;
- blood supply disorders (atherosclerosis, arterial hypertension, amyloidosis, etc.);
- infectious diseases (diphtheria, botulism, tetanus and others);
- disorders of the liver or kidneys, accompanied by the accumulation of toxins in the blood;
- disorders of glucose metabolism;
- lack of vitamins (especially group B);
- water retention, lack of sodium in the blood and resulting swelling;
- immunodeficiency states;
- exposure to ionizing radiation;
- hypoxia: insufficient oxygen supply to brain cells.
Kinds
Doctors distinguish between congenital and acquired encephalopathy. The first occurs against the background of an abnormal course of pregnancy or childbirth and, often, develops while the fetus is in the womb. Its signs are detected immediately after birth or appear in the first weeks of life. Neonatologists and pediatricians are involved in the diagnosis and treatment of this condition.
Acquired encephalopathy occurs in adulthood. It is divided into several types depending on the cause of neuronal death:
- post-traumatic: occurs against the background of a traumatic brain injury; often develops within a few years after it and often leads to severe mental disorders;
- toxic: associated with acute or chronic poisoning of the body with alcohol, poisons, narcotic drugs, medicines, salts of heavy metals, etc.; Alcoholic encephalopathy is often distinguished separately within this type;
- metabolic: associated with metabolic disorders in the body; The following subtypes of pathology are distinguished: hepatic: occurs when the liver or biliary tract is damaged;
- uremic: associated with impaired renal function;
- diabetic: is one of the frequent complications of diabetes mellitus, occurs against the background of persistent microcirculation disorders and increased blood viscosity;
- anoxic: develops after clinical death and is associated with oxygen starvation of the brain with the subsequent development of a “metabolic storm”;
- Gaye-Wernicke syndrome: encephalopathy caused by vitamin B1 deficiency;
- pancreatic: is a complication of inflammation of the pancreas;
- hypoglycemic: occurs against the background of a sharp decrease in blood glucose;
- atherosclerotic: develops due to atherosclerosis and thickening of the walls of blood vessels;
Depending on the speed of development of the process, encephalopathy is divided into acute and chronic. The first can develop within a few days or hours, and more often occurs against the background of severe intoxication, trauma, or an infectious process. The chronic process can last for years or decades.
Meningitis
Encephalitis
Fungus
Vomit
Rubella
Measles
27231 07 June
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Meningitis: causes, symptoms, diagnosis and treatment methods.
Definition
Meningitis is an infectious inflammation of the meninges of the brain and spinal cord, accompanied by intoxication, fever, increased intracranial pressure syndrome, meningeal syndrome, as well as inflammatory changes in the cerebrospinal fluid.
The meninges are connective tissue membranes that cover the brain and spinal cord. There are dura mater, arachnoid and pia mater.
The dura mater of the brain has a dense consistency and thickness of 0.2-1 mm; in places it fuses with the bones of the skull. The arachnoid membrane is a thin, translucent, non-vascular connective tissue plate that surrounds the brain and spinal cord. The soft shell is a thin connective tissue plate directly adjacent to the brain, corresponds to its relief and penetrates into all its recesses. In its thickness is the vascular network of the brain.
The most common inflammation is inflammation of the pia mater, and the term “meningitis” is used.
Causes of meningitis
The meninges can be involved in the inflammatory process primarily and secondary. Meningitis that occurs without a previous general infection or disease of some other organ is called primary. Secondary meningitis develops as a complication of an existing infectious process. Secondary ones include tuberculous, staphylococcal, pneumococcal meningitis. The primary ones are meningococcal, primary mumps, enteroviral meningitis and others.
The disease is transmitted by airborne droplets, household contact or nutrition.
Purulent inflammation of the meninges can be caused by various bacterial flora (meningococci, pneumococci, and less commonly, other pathogens). The cause of serous meningitis is viruses, bacteria, fungi.
According to the forecast, the most dangerous is tuberculous meningitis, which occurs when there is a tuberculous lesion in the body. The development of the disease occurs in two stages. At the first stage, the pathogen, through the bloodstream, infects the choroid plexuses of the ventricles of the brain with the formation of a specific granuloma in them. In the second, inflammation of the arachnoid and soft membranes is observed (as a rule, the membranes of the base of the brain are affected), which causes acute meningeal syndrome.
The development process of meningococcal meningitis also consists of several stages:
- contact of the pathogen with the mucous membrane of the nasopharynx;
- entry of meningococcus into the blood;
- penetration of the pathogen through the blood-cerebrospinal fluid barrier, irritation of pia mater receptors by toxic factors and inflammation.
The course of the infectious process depends on the pathogenic properties of the pathogen (the ability to cause disease) and the state of the human immune system.
Previous viral diseases, sudden climate change, hypothermia, stress, concomitant diseases, therapy that suppresses the immune system can be significant for the occurrence and course of meningitis.
Classification of the disease
According to the type of pathogen:
- Viral meningitis (influenza, parainfluenza, adenovirus, herpes, arbovirus (tick-borne), mumps, enterovirus ECHO and Coxsackie).
- Bacterial meningitis (meningococcal, tuberculous, pneumococcal, staphylococcal, streptococcal, syphilitic, brucellosis, leptospirosis).
- Fungal (cryptococcal, candidiasis, etc.).
- Protozoal (toxoplasmosis, malaria).
- Mixed.
According to the nature of inflammation:
- Serous.
- Purulent.
According to the mechanism of occurrence:
- Primary.
- Secondary.
With the flow:
- Spicy.
- Subacute.
- Fulminant.
- Chronic.
By severity:
- Easy.
- Medium-heavy.
- Heavy.
According to the prevalence of the process:
- Generalized.
- Limited.
According to the presence of complications:
- Complicated.
- Uncomplicated.
Symptoms and syndromes of meningitis
There are a number of syndromes common to all meningitis:
- meningeal syndrome - manifested by rigidity (increased tone) of the neck muscles and long back muscles, hypersthesia (increased sensitivity) of the sensory organs, headache, vomiting, changes in the cerebrospinal fluid;
- cerebral syndrome - manifested by drowsiness, impaired consciousness, nausea, vomiting, dizziness, psychomotor agitation, hallucinations;
- asthenovegetative syndrome – manifested by weakness, decreased ability to work;
- convulsive syndrome;
- general infectious syndrome - manifested by chills and fever.
Meningococcal meningitis ranks first among purulent meningitis.
Its incubation period ranges from 1 to 10 days, with an average of 2-4 days. The disease usually begins acutely against the background of complete health or shortly after nasopharyngitis. Patients can indicate not only the day, but also the hour of illness; they are worried about chills, body temperature above 38℃, severe bursting headache, aggravated by any noise and movement of the head. Patients may experience pain in various parts of the body, and touching causes excruciating sensations. Vomiting is not associated with food intake and does not bring relief. Soon, stiffness of the neck and long back muscles sets in. Patients take a “meningeal” position. Infants cry constantly, they may experience bulging fontanelles and gastrointestinal disorders. Pneumococcal meningitis, as a rule, is observed in young children against the background of an existing pneumococcal process (pneumonia, sinusitis).
With streptococcal meningitis, hepatolienal syndrome (enlarged liver and spleen), renal failure, adrenal insufficiency, petechial rash (hemorrhages due to damage to the capillaries, as a result of which blood, spreading under the skin, forms round spots, the size of which does not exceed 2 mm).
Purulent meningitis caused by Pseudomonas aeruginosa and fungi are rare. The diagnosis is established only after additional laboratory tests.
Serous tuberculous meningitis is characterized by a gradual onset, although in rare cases it can manifest itself acutely. At the onset of the disease, patients complain of fatigue, weakness, irritability, and sleep disturbances. The temperature is usually no higher than 38℃, and there is an intermittent moderate headache. On the 5-6th day of illness, the temperature rises above 38℃, the headache intensifies, nausea, vomiting, and drowsiness appear. Unconsciousness develops quickly. A divergent strabismus, a low position of the upper eyelid in relation to the eyeball, and pupil dilation may be observed.
When diagnosing mumps meningitis, it is important to identify recent contact with someone with mumps.
Clinical manifestations of damage to the meninges may develop even before the enlargement of the salivary glands.
Enteroviral meningitis is characterized by two- and three-wave fever with intervals between waves of 1-2 or more days. Other manifestations of enterovirus infection are almost always observed (muscle pain, skin rash, herpangina).
For the diagnosis of measles and rubella meningitis, an indication of contact with a patient with these diseases, as well as typical clinical symptoms of measles or rubella, is of great importance.
Diagnosis of meningitis
To confirm the diagnosis of meningitis, the doctor may prescribe a set of laboratory and instrumental studies:
- clinical blood test with determination of hemoglobin concentration, number of erythrocytes, leukocytes and platelets, hematocrit and erythrocyte indices (MCV, RDW, MCH, MCHC), leukoformula and ESR (with microscopy of a blood smear in the presence of pathological changes);
Symptoms
Signs of encephaloptia depend on the location of the source of destruction, as well as the degree of development of the disease. Most often, patients and their relatives experience the following symptoms:
- headache: can involve the entire head or concentrate in certain areas; the intensity depends on the degree of damage and gradually increases; pain is poorly relieved by taking analgesics;
- dizziness: occurs sporadically, accompanied by loss of orientation in space; Often a person is forced to wait out this condition in bed, since the slightest movement worsens the symptom; the condition is often accompanied by constant nausea and vomiting;
- impairment of cognitive functions: a gradual decrease in the ability to think adequately is a characteristic sign of encephalopathy; a person gradually becomes forgetful, absent-minded, has trouble concentrating on a specific process and has difficulty switching between different activities;
- emotional and behavioral disorders: a person has difficulty controlling his emotions, becomes irritable, whiny, gets excited quickly; as the disease progresses, apathy, depression and complete reluctance to do anything arise;
- increase or decrease in muscle tone; often accompanied by hyperkinesis (trembling in the limbs, obsessive movements, etc.);
- decreased vision and hearing;
- increased weather sensitivity.
In some patients, behavioral disorders predominate, others cease to have normal control of their body; in others, it is mainly the sense organs that are affected. In severe cases, a person requires constant care and supervision of others.
Primary encephalitis
Tick-borne encephalitis
As a rule, the causative agent of this type of disease is the neurotropic tick-borne encephalitis virus. The carriers of the virus are considered to be ixodid ticks, which enter the human body through a tick bite or through nutrition, which means by consuming raw contaminated milk. Subsequently, the penetration of the virus into the plane of the nervous system will be hematogenous.
Typically, the incubation period for people with encephalitis is up to 30 days if the virus entered through a tick bite. In some cases, the incubation period will reach 60 days. If the infection was alimentary, then the interval of such a period will be 4-7 days.
Microscopy of the brain can reveal hyperemia and various glial or mesodermal reactions, as well as infiltrates arising from mononuclear or polynuclear cells.
As a rule, inflammatory changes are localized on the nuclei of the medulla oblongata, as well as in the anterior parts of the so-called horn of the cervical segments located in the spinal cord and on the pons. In addition, the cerebral cortex can be affected by the inflammatory process.
Traditional symptoms of tick-borne encephalitis will be: acute onset, which manifests itself in the form of an increase in body temperature up to 40 degrees; aching joints; pain in the lower extremities and lower back.
In the very first days of the illness, the patient experiences typical symptoms of encephalitis such as nausea, vomiting and headache. Confusion of consciousness is also observed, which in some cases reaches the development of mental disorders, expressing themselves in the form of delusions, sound hallucinations and severe depressive disorder.
Today there are several forms of tick-borne encephalitis:
- polio;
- encephalitic;
- meningeal;
- febrile;
- polyradiculoneuritis;
- two-wave viral.
The difference between all these forms is how pronounced certain neurological symptoms are. When diagnosing tick-borne encephalitis, great importance is given to the anamnesis. As you know, a very small percentage of ticks (up to 5%) are considered carriers of the pathogen virus, so you should not mistake every disease for encephalitis if it occurs after a tick bite.
Encephalitis is determined on the basis of the neutralization reactions obtained, the complement fixation reaction or the inhibition of hemagglutination. When diagnosing, great importance is given to the type of virus found in the blood or cerebrospinal fluid. Typically, laboratory tests determine ESR in the blood, as well as leukocytosis, while in the cerebrospinal fluid itself they “look for” lymphocytic pleocytosis with a presence of an increase in protein with an indicator of up to 1 g/l.
First of all, the signs of tick-borne encephalitis are differentiated from typhus, acute polio and serous meningitis.
Japanese mosquito encephalitis
This type of disease is caused by a neurotropic virus. Typically, its carriers are considered to be those species of mosquitoes that are characterized by transovarial transmission of the virus. In this case, the incubation period lasts up to 14 days. It should be said that Japanese mosquito encephalitis develops very sharply. It begins with a sudden increase in body temperature (which in some patients is up to 40 degrees). Other symptoms include vomiting and severe headaches.
The symptomatic picture of this type of disease is also characterized by symptoms such as tachycardia, herpetic rashes, facial hyperemia and dry tongue. Today, there are several forms of Japanese mosquito encephalitis:
- convulsive;
- hemiparetic;
- bulbar;
- hyperkinetic;
- lethargic.
The difference between these forms is the presence of one or another predominant syndrome. Regardless of the form of Japanese mosquito encephalitis, the course of this disease is particularly acute. In the first 5 days, symptoms increase, body temperature rises and remains high for 12-14 days. Body temperature can usually decrease lytically. If we talk about death, it occurs in 70% of patients in the first week of the disease. Of course, death is possible in later stages of the disease. This is facilitated by an additional complication, which most often is pulmonary edema.
Considerable importance in diagnosing this disease is given to its seasonality and the collected epidemiological data. Verification of the diagnosis is carried out on the basis of complement and neutralization reactions, as well as determination of antibodies, which is possible already in the second week of the disease.
Epidemic lethargic encephalitis Economo
Today, Economo's epidemic lethargic encephalitis practically does not occur, and its causative agent has not yet been definitively identified. In their clinic, the disease is divided into two stages:
- acute stage (characterized by an inflammatory nature);
- chronic stage (it is characterized by a progressive course of a degenerative nature).
The classic version of the symptomatic severity of the lethargic form of encephalitis, which has developed to the acute stage, begins with high body temperature, which often reaches 39 degrees, vomiting, general weakness and severe headaches. The patient has been feverish for two weeks. At the same time, neurological symptoms such as constant drowsiness (or vice versa, insomnia), abnormalities in the functioning of the oculomotor nerves occur, which sometimes leads to ptosis.
Among the extrapyramidal symptoms that are characteristic of the chronic stage of this disease, hyperkinesis (athetosis, choreoathetosis or gaze convulsions), amymia, muscle rigidity, akinesis (which constitutes akinetic-rigid syndrome) are often distinguished.
In special cases, at the acute stage, epidemic encephalitis can occur with such pronounced psychogenic disorders as auditory or visual hallucinations, which manifests itself in the inability to correctly distinguish the color of surrounding objects.
The acute stage of this pathology during diagnosis is often characterized by lymphocytic pleocytosis, a slight increase in the level of glucose, lymphocytes and eosinophils in the blood. The acute stage of the disease can last for 4 days, and in some cases up to several months, after which either the patient recovers, or the disease becomes chronic with the possible preservation of partial symptoms in the form of depression, ptosis, insomnia or convergence.
The main symptomatic manifestation of the chronic stage of Economo encephalitis is considered to be parkinsonism syndrome, in parallel with which all sorts of endocrine-type disorders arise (menstruation disorders, infantilism, obesity, cachexia or diabetes insipidus).
It is very difficult to diagnose epidemic encephalitis at the acute stage. Diagnosis, as a rule, is based on forms of sleep disturbance, which is accompanied by psychosensory disorder and manifestations of impaired functionality of the oculomotor nerves. Considerable attention must be paid to increasing body temperature.
If we talk about the diagnosis of the chronic stage of this disease, it is based on the study of parkinsonism syndrome, as well as on checking endocrine disorders (of central origin) and possible changes in the psyche and behavior of the patient.
Complications
Complications of encephalopathy are associated with severe and irreversible damage to the brain and represent the extreme extent of the symptoms observed:
- loss of self-care ability due to motor or cognitive impairment;
- dementia: loss of knowledge and skills up to complete collapse of personality;
- loss of vision and hearing;
- severe mental disorders;
- convulsions;
- disturbances of consciousness: stupor, coma;
- death.
Secondary encephalitis
Influenza encephalitis
Influenza encephalitis is caused by influenza viruses B, A1, A2 and A3. The disease occurs as a complication after the flu. Among the main pathogenetic mechanisms of this disease, dyscirculatory phenomena occurring in the brain come first. In addition to them, the disease is influenced by neurotoxicosis. As you know, it is almost impossible to avoid damage to the nervous system during influenza. Typically, such damage to the nervous system manifests itself in the form of muscle and headaches, drowsiness and weakness. If influenza encephalitis continues to develop, the patient suddenly begins to feel unwell, vomiting and dizziness.
If we talk about the cerebrospinal fluid, then a slight increase in the level of protein, as well as slight pleocytosis, can be detected in it, which is detected in the case of a lumbar puncture, when the cerebrospinal fluid begins to leak due to increased pressure.
In many cases, at the acute stage of influenza-type encephalitis, severe damage can develop, which manifests itself as a hemorrhagic type of influenza encephalitis, which begins with a sharp rise in body temperature, as well as chills and disturbances of consciousness, which in rare cases even leads to coma. Traces of blood are often observed in the cerebrospinal fluid. The course of this form of the disease is particularly severe, so very often death can occur. If the disease has a positive outcome, then some neurological disorders will still remain in the patient even after recovery.
Measles encephalitis
Measles encephalitis is an infectious-allergic type of encephalitis. It develops quite quickly and in an acute form, which on the 5th day manifests itself in the form of a rash or measles, even when the body temperature, it would seem, has already returned to normal, it suddenly jumps to 40 degrees.
Very often, with measles encephalitis, severe disturbances of consciousness may occur, such as:
- auditory or visual hallucinations;
- generalized seizures;
- psychomotor type agitation;
- impaired coordination of movements;
- characteristic paresis of the limbs;
- hyperkinesis;
- disruptions in the functioning of the pelvic organs.
During the examination of the cerebrospinal fluid, an increased protein content, as well as possible pleocytosis, can be determined. Doctors note a very severe course of this disease, the mortality rate is about 20-25%.
Diagnostics
A neurologist is involved in the diagnosis and treatment of encephalopathy. Patient examination includes:
- survey: collection of complaints and anamnesis; it is mandatory to clarify information about previous diseases, injuries, risk factors, the time of the first violations, the rate of development, etc.;
- neurological examination: assessment of reflexes, sensitivity, muscle strength, motor function;
- electroencephalography (EEG): assessment of electrical impulses arising during brain function; allows you to identify signs of epilepsy, inflammation, the presence of tumors, etc.;
- Doppler ultrasound of the vessels of the brain and neck: assesses the quality of blood flow in large vessels, identifies areas of narrowing, assesses the volume of incoming blood;
- rheoencephalography: complements ultrasound, allows you to assess the tone and elasticity of blood vessels, detect blood clots;
- angiography: X-ray examination of blood vessels by introducing a contrast agent into them;
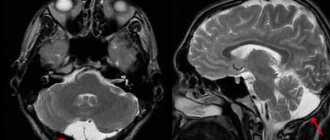
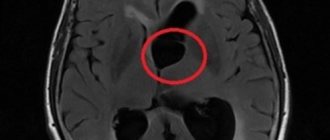
- CT and MRI: allow you to detect foci of sclerosis, tumors, inflammatory foci, consequences of stroke and other structural changes;
- blood tests (general, biochemical): make it possible to evaluate the functioning of the kidneys, liver, pancreas, and identify toxins that can affect the condition of the brain.
If necessary, other tests and examinations may be prescribed, as well as specialist consultations to accurately determine the cause of encephalopathy.
Make an appointment
Diagnosis of meningitis
The diagnosis of meningitis can be made based on the results of additional studies - laboratory and instrumental:
- detailed blood test;
- fundus examination;
- X-ray examination of the skull;
- heart electrocardiograms;
- electroencephalography;
- computer and magnetic resonance imaging.
Doctors at the Yusupov Hospital confirm or refute the diagnosis of meningitis using a study of cerebrospinal fluid. A lumbar puncture is performed immediately after examining the patient. Normal cerebrospinal fluid is transparent, colorless, and flows out under a pressure of 130-180 mm during puncture. water Art. It detects from two to eight cells in one microliter. In serous meningitis, the cerebrospinal fluid is colorless, clear or opalescent. During cerebrospinal puncture, it flows out under a pressure of 200-300 mm. water Art. at a speed of 60-90 drops per minute. In the cerebrospinal fluid, from 200 to 800 cells are determined in 1 μl, 80-100% are lymphocytes. The amount of protein and glucose is increased. After the puncture, the patients' condition improves significantly.
With serous-bacterial meningitis, the cerebrospinal fluid may be colorless or yellow, opalescent. During puncture, it flows out in a stream under a pressure of 250-500 mm of water column. The number of cells increases to 800-1000 in 1 μl, they contain the same number of lymphocytes and neutrophils. Protein levels are increased and glucose concentrations are significantly decreased.
The liquor in purulent-bacterial meningitis is cloudy, whitish or greenish-brown. Due to the high viscosity and blockage of the liquor pathways, it often flows out in rare drops under high pressure. The number of cells in one milliliter of cerebrospinal fluid exceeds 1000; they consist mainly of neutrophils. Protein concentration varies from 600 to 16,000 mg/l, glucose levels are reduced.
To confirm the diagnosis of meningitis, doctors use bacteriological examination of mucus from the nasopharynx and cerebrospinal fluid. During bacterioscopic examination of cerebrospinal fluid, smears are stained with Gram or methylene blue. To exclude fungal meningitis, the specimen containing cerebrospinal fluid is stained with ink. Laboratory assistants isolate a pure culture on media with the addition of normal horse serum or cattle serum and identify it by biochemical activity and antigenic structure.
In case of viral meningitis, in preparations prepared with Gram staining and ink, it is impossible to identify the causative agent of the infection. Cultivation of bacteria and fungi also gives negative results. By culturing cellular material with standard laboratory cell lines, a pathogen serologically identical to the measles virus can be isolated. Rubella virus is isolated using the co-cultivation method.
To identify oligoclonal immunoglobulins, the method of agarose gel electrophoresis or isoelectric focusing of cerebrospinal fluid gamma globulins is used. Immunoglobulins appear in a number of viral infections. As a result of immunological studies, viral antigens or antibodies are detected in the cerebrospinal fluid, and the nucleic acid of the virus is detected using the polymerase chain reaction method. The enzyme immunoassay method detects pathogen antigens in feces, urine or saliva. Express methods allow you to quickly and early determine the presence of the herpes simplex virus antigen in the cerebrospinal fluid and blood or the DNA of the virus (using the polymerase chain reaction method).
Laboratory diagnosis of meningitis using modern research methods can be performed at the Yusupov Hospital. According to indications, doctors determine changes in brain tissue using computer or magnetic resonance imaging. If the first signs of meningitis are present, adequate antibiotic therapy is started immediately after diagnosis.
Make an appointment
Treatment
The sooner treatment for encephalopathy is started, the greater the chance of stopping the progression of the pathology and restoring full brain function.
First of all, it is necessary to eliminate the cause of neuronal damage:
- adjust blood sugar levels;
- stabilize blood pressure;
- restore the functioning of the liver, kidneys, pancreas;
- reduce blood cholesterol levels;
- remove toxins;
- normalize hormone levels, etc.
Direct treatment of encephalopathy requires the prescription of drugs that improve blood flow in the vessels of the brain and metabolism within the cell. Depending on the cause and extent of the lesion, doctors may prescribe:
- nootropics (Cerebrolysin, piracetam): aimed at enhancing metabolism;
- blood thinners (aspirin, pentoxifylline, etc.): help accelerate blood flow, prevent the formation of blood clots;
- antioxidants: neutralize toxins;
- angioprotectors (Cavinton, nicotinic acid and others): necessary to accelerate blood circulation and metabolism;
- vitamin-mineral complexes, amino acids;
- symptomatic drugs: sedatives, anticonvulsants, etc.
For encephalopathy, courses of treatment are carried out regularly, at least 2 times a year. This allows you to keep the disease under control. The selection of specific drugs and determination of dosage is carried out only by a doctor. There is no single treatment regimen for all patients.
To enhance the effect of drugs, non-drug treatment methods are used:
- physiotherapy (reflexotherapy, electrophoresis, magnetic therapy, laser therapy);
- physical therapy to improve muscle condition and facilitate control over them;
- massage to relax and improve blood circulation;
- acupuncture.
In some cases (with the vascular nature of encephalopathy), it is necessary to resort to surgical treatment:
- elimination of a blood clot from the lumen of blood vessels;
- expansion of narrowed sections of the artery with the installation of a stent that supports the walls in the correct position;
- bypass: restoration of blood flow by creating an alternative path that bypasses the affected area.
Treatment of encephalitis
When treating any type of encephalitis in neurology, several types of therapies are used, which may include several areas at once:
- Dehydration and methods to combat brain swelling (usually a solution of mannitol 20% is used for this, which is administered intravenously at 1.5 g per kilogram of body, furosemide, which is also administered intravenously; as an option, acetazolamide at 40 mg per dose can be used).
- Desensitization (using diphenhydramine, chloropyramine or clemastine).
- Hormone therapy that can have an anti-inflammatory, dehydrating or desensitizing effect on the patient’s body. In addition, hormone therapy helps protect the adrenal cortex from exhaustion (prednisolone is usually prescribed at 10 mg per kilogram of the patient’s body, administered into the body using pulse therapy over the next 5 days, and dexamethasone is also often prescribed, administered intravenously or intramuscularly at 16 mg per day).
- An isotonic solution of dextran, administered intravenously through a dropper. This therapy significantly improves microcirculation.
- Parenteral or enteral nutrition, the use of potassium chloride or dextran - all this helps maintain normal homeostasis and water-salt balance.
- The use of angioprotectors (for example, a combination of etamivan, hexobendine, vinpocetine or pentoxifylline).
- The use of antihypoxants, including ethylmethylhydroxypyridine succinate.
Treatment of cardiovascular abnormalities may be prescribed. Typically, such treatment involves the use of glycosides, glucocorticoids, camphor and vasopressors. It is possible to normalize the patient's breathing in case of encephalitis with the help of hyperbaric oxygenation or oxygen therapy, as well as by intubation or mechanical ventilation.
When treating encephalitis, specialists may be faced with the need to restore proper metabolism within the brain. For this purpose, the use of special vitamins, piracetam or polypeptides is prescribed. Among the anti-inflammatory drugs, salicylates and ibuprofen are often prescribed.
If we talk about such a common type of therapy as etiotropic, then it involves the use, first of all, of antiviral drugs, for example, nucleases that can delay the replication of the virus. So, for example, interferon alpha-2 or it in combination with ribavirin is often prescribed (only in the most extreme cases). If doctors are dealing with DNA viral encephalitis, then the most effective treatment will be the use of tilorone, while drugs from the group of corticosteroids (for example, metipred) are prescribed at a rate of 10 mg per kilogram of body daily for three to four days.
Symptomatic therapy is one of the most common in the treatment of encephalitis. It involves performing manipulations in several directions:
- antipyretic treatment;
- anticonvulsant therapy;
- treatment of delirious syndrome.
To stop an epileptic seizure, diazepam can be used (usually prescribed 10 mg as a dextrose solution intravenously) or a one percent solution of sodium thiopental (also intravenously). In addition, doctors may prescribe phenobarbital or primidone.
Among antipyretics, lytic mixtures, metamizole sodium solutions, ibuprofen or droperidol are usually prescribed. If we talk about individual therapy for delirious syndrome, then the use of magnesium sulfate or lytic mixtures comes first.
To restore the normal functioning of the nervous system and rehabilitate consciousness, all kinds of biostimulants, antidepressants or tranquilizers are prescribed.
As for rehabilitation therapy, it involves the use of several drugs at once that fight parkinsonism, Kozhevnikov epilepsy, muscle paresis, and neuroendocrine disorders. For example, parkinsonism is treated with anticholinergics or levodopa, while the stereotactic type of surgery is indicated in cases of increased rigidity and poor effectiveness of drug treatment. As for the use of metabolic drugs, tranquilizers or neuroleptics, they are indicated in the treatment of hyperkinesis.
The use of anticonvulsants and antipsychotics helps in the treatment of Kozhevnikov epilepsy, while for the treatment of severe paresis, energy correctors and medications that can stimulate metabolic processes inside the brain are used. If we talk about methods of treating neuroendocrine disorders, the use of metabolic drugs, antipsychotics and desensitizing medications is shown here.
Physicians strongly recommend exercise therapy, massage therapy, or physical therapy.
Prevention
Encephalopathy is a complex disease. There is no clear method to prevent its occurrence and eliminate all risk factors. Doctors recommend adhering to the following rules:
- provide yourself with a full daily routine with alternating work and rest, a full night’s sleep;
- minimize stress;
- eat properly and balanced, avoid overeating and excess body weight;
- ensure sufficient supply of vitamins and microelements;
- quit smoking, drugs, alcohol;
- exercise in moderation (not professionally);
- promptly identify and treat chronic diseases: hypertension, diabetes, atherosclerosis;
- consult a doctor at the first signs of trouble.
FAQ
Who is most at risk for encephalitis?
Encephalitis is a rare disease, but it can manifest itself in representatives of both sexes. According to statistics, it most often affects people with weakened immune systems.
Can the vaccine cause encephalitis?
There really are such cases. But the risk of getting sick from what you are vaccinated against is much higher than the risk of getting a complication such as encephalitis. Therefore, it is unreasonable to refuse vaccination.
Treatment at the Energy of Health clinic
Doctors at the Health Energy Clinic are always ready to see patients of any age. We will conduct a thorough examination, identify possible causes of encephalopathy and take all measures to eliminate it:
- we will prescribe the most appropriate therapy, describe the course of treatment and the frequency of its repetition;
- We will carry out all the necessary manipulations (placement of a drip, intravenous and intramuscular injections) in the comfortable conditions of a day hospital and manipulation room;
- We will complement the therapy with modern physiotherapeutic procedures;
- We will conduct a massage course and prescribe exercise therapy for maximum effectiveness.
Our neurologists will monitor the patient’s condition and adjust treatment if necessary. Treatment of encephalopathy is a long and complex process, but we are ready to take on it.
Advantages of the clinic
If you require a full examination and high-quality treatment, welcome to the Health Energy clinic. Here you are waiting:
- experienced specialists who regularly improve their skills to keep abreast of all new trends in the world of medicine;
- modern diagnostic equipment;
- everything necessary for physiotherapy, massage, exercise therapy;
- own day hospital for slow drip administration of medications;
- affordable prices for all services.
If you or your relatives have signs of encephalopathy, do not delay contacting a doctor. The sooner treatment is started, the better the result. Sign up for the Health Energy clinic and let our doctors choose the optimal therapy.