Fatty liver disease, non-alcoholic fatty liver disease (NAFLD) - symptoms and treatment
The accumulation of cholesterol, namely lipids (fat-like organic compounds) in the liver, is primarily caused by the following factors:
- excess supply of free fatty acids (FFA) to the liver;
- increased synthesis of free fatty acids in the liver;
- decreased levels of beta-oxidation of free fatty acids;
- decreased synthesis or secretion of very high-density lipoproteins.[7]
In obese patients, the liver tissue has an increased content of free fatty acids, which may be the cause of liver dysfunction, since fatty acids are chemically active and can lead to damage to the biological membranes of hepatocytes, forming a gateway for endogenous fat to enter the cell, in particular lipids (mainly low and very low density), and transport is an ester - triglyceride.[2]
Thus, hepatocytes become filled with fat, and the cell becomes functionally inactive, swells and increases in size. When more than a million cells are damaged, the liver macroscopically increases in size, in areas of fatty infiltration the liver tissue becomes denser, and these areas of the liver do not perform their functions or perform them with significant defects.
Lipid peroxidation in the liver leads to the synthesis of toxic intermediates that can trigger the process of apoptosis (programmed cell death), which can cause inflammation in the liver and form fibrosis.[2]
Also of important pathogenetic importance in the formation of NAFLD is the induction of cytochrome P-450 2E1 (CYP2E1), which can be induced by both ketones and a high-fat, low-carbohydrate diet.[7] CYP2E1 generates toxic free radicals leading to liver damage and subsequent fibrosis.
In addition, endotoxin-mediated damage is of pathogenetic importance in the formation of NAFLD, which, in turn, enhances the production of pro-inflammatory cytokines (TNF-α, IL-6 and IL-8), leading to disruption of the integrity of hepatocyte membranes and even to their necrosis[ 9], as well as to the development of inflammatory cell infiltration both in the portal tracts and in the liver lobules, which leads to steatohepatitis.
Products of lipid peroxidation, hepatocyte necrosis, TNF and IL-6 activate stellate (Ito) cells, causing damage to hepatocytes and the formation of fibrotic changes.
How to get rid of liver fat? 5 rules of behavior
Unfortunately, there is no “magic pill” for fatty liver disease. Only diet and physical activity. That's why:
- Limit animal fat - exclude butter, fatty meat, lard, smoked meats, remove the skin from poultry, switch to vegetable oils.
- Limit sweets and starchy foods, love vegetables - only “slow” carbohydrates, up to 100 g per day, instead of sugar - use substitutes, preferably stevia.
- Eat enough proteins, but less red meat - fish, poultry, low-fat cottage cheese, natural yogurt, eggs are best.
- Stop drinking alcohol or reduce the dose to a safe one.
- Exercise 3 times a week for 45 minutes. Every time you exercise, your insulin levels drop for 48 hours and your liver will gradually stop storing fat.
Diagnostics
Diagnosis of the disease is difficult. Firstly, steatosis has no specific symptoms. Secondly, biochemical tests do not show significant changes. Sometimes the activity of serum transaminases increases, but this indicator does not change in all patients with steatosis. In this regard, differential diagnosis with hepatitis, biliary tract obstruction, primary hemochromatosis, and hepatocerebral dystrophy is of primary importance.
The doctor makes the final diagnosis based on a comprehensive examination and a series of tests, including ultrasound and biopsy.
To find out the cause of fatty hepatosis, the level of insulin in the blood, serum glucose concentration, hormonal status, antibodies to cytomegalovirus and hepatitis viruses, markers of autoimmune hepatitis, etc. are determined.
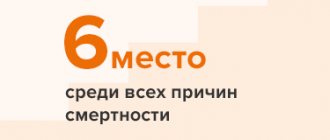
Why is NAFLD dangerous?
Fatty hepatosis, especially at the very beginning, can be practically asymptomatic, and the existing symptoms are not specific and, thus, make diagnosis difficult. However, you should not relax - diagnosing fatty hepatosis is important for any suspicion of the presence of this disease. Because this disease, developing gradually, practically without manifesting itself clearly, nevertheless increases the risk of cardiovascular death several times - in other words, it increases the risk of developing strokes and heart attacks.4 In addition, advanced fatty hepatosis can ultimately lead to ultimately, to the development of cirrhosis and liver failure. The likelihood of this event is low, however, if it occurs, the consequences can be fatal. The fact is that cirrhosis usually requires organ transplantation, which can be further complicated in the presence of cardio-metabolic disorders and diseases that often accompany fatty hepatosis.3
Stages of development of NAFLD
- 1
Stage of fatty hepatosis (steatosis)
The initial stage of the disease, often asymptomatic
- 2
Non-alcoholic steatohepatitis
Hepatosis with accompanying inflammation of liver cells
- 3
Fibrosis with further transition to cirrhosis
At this stage, liver tissue begins to be replaced by connective tissue, which leads to disruption of the structure and, ultimately, disruption of the organ.3
Risk factors for the development of steatosis 1.3
- Obesity or overweight, with a body mass index of 25 or higher
- Type 2 diabetes mellitus or decreased insulin sensitivity
- Lipid metabolism disorders, in particular dyslipidemia
- Metabolic syndrome
- Age 30 – 59 years
- Physical inactivity
- Binge eating
What are the signs of fatty liver disease?
As we mentioned above, the main feature of this condition is the absence of specific symptoms. Therefore, the disease is often detected by chance, often during a routine medical examination or examination for a completely different disease.
Among the symptoms that often occur with fatty hepatosis, but can be ignored, you should pay attention to:
- Discomfort in the area of the right hypochondrium, without a clear connection with food intake
- Fatigue
- Weakness
If these symptoms are detected and there is concern about the condition of the liver, then to clarify the diagnosis, you should consult a doctor who can prescribe a diagnostic method such as ultrasound. Ultrasound will help identify increased liver volumes and changes in the echogenicity of the organ. The doctor may also recommend testing liver enzymes - ALT, AST. In some cases, a specialist may see the need for a liver biopsy (examination of liver tissue under a microscope), which provides the most reliable information about the condition of the organ.1,4
Classification
Based on etiology, hepatosis is divided into non-alcoholic fatty liver disease and alcoholic steatosis. The first type of disease is diagnosed in only 7–10% of cases.
Hepatosis occurs:
- primary - caused by metabolic disorders, for example, obesity or hyperlipidemia;
- secondary – due to the impact on the body of external negative factors, which subsequently lead to metabolic disorders, for example, fasting, long-term use of corticosteroids, intestinal resection.
Doctors also take into account the characteristics of fat deposition, according to which hepatosis is divided into:
- diffuse;
- zonal;
- focal disseminated;
- pronounced disseminated.
Frequently asked questions about fatty liver disease
Which doctor should I contact?
A hepatologist specializes in liver diseases.
How to determine fatty hepatosis?
Unfortunately, the disease has no specific symptoms. A comprehensive examination allows you to identify deviations.
Can hepatic steatosis be cured?
With proper and timely therapy, changes in the liver are reversible. The main thing is to strictly follow all the doctor’s instructions, stick to your diet, and give up alcohol and “harmful” foods.
Causes and mechanism of development of fatty hepatosis
The main reasons for the development of fatty hepatosis is the accumulation of triglyceride molecules, fat breakdown products, in liver cells. This is due to a disruption in the processes of synthesis and utilization of these molecules, due to the development of insulin resistance and disruption of the hormones responsible for fat metabolism.
Currently, the exact mechanisms of development of fatty liver are unknown; the question still remains as to the reasons for the transition of hepatosis to steatohepatitis and subsequently to cirrhosis of the liver
Prevention
Preventive measures include:
- proper nutrition, in particular limiting fatty, spicy, fried and smoked foods;
- moderation in the consumption of alcoholic beverages;
- taking medications correctly;
- regular physical activity.
Fat accumulation is often caused by excess weight due to a sedentary lifestyle. Scientists have proven that if you eat only fast food for 4 weeks, this disease will almost certainly occur. Student volunteers took part in the experiment. Moreover, the first signs appeared after 1 week of such nutrition. Therefore, nutrition and weight control are of great importance.
For prevention, hepatoprotectors should be used, especially during periods of increased load on the liver, for example, with prolonged alcohol consumption, antibiotic treatment, and following a diet aimed at weight loss.