- What is inflammation of the synovial bursa of the shoulder joint?
- Symptoms of shoulder bursitis
- Causes of inflammation of the mucous bursa in the shoulder
- Diagnosis and medical examination of bursitis
- Conservative treatment
- Surgical treatment of shoulder bursitis
In addition to inflammation of the mucous membrane, there are other causes of shoulder pain. Tendon inflammation, traumatic injuries or, for example, arthrosis have similar symptoms. A specialized medical examination will help establish the causes of pain and select the appropriate treatment. © yodiyim / fotolia Bursitis (Latin bursa “bag”) is a painful inflammation of the periarticular bursa of the shoulder. The bursae are located close to the joints to balance the high mechanical load between bones and other tissues. The largest bursa in the human body (Bursa subakromialis or subacromial bursa) is located in the shoulder. The cause of its inflammation may be pathologies of various structures of the complex shoulder joint. The shoulder may become inflamed due to bone spurs on the acromion of the clavicle (acromion) or structural changes in the supraspinatus tendon (eg calcium deposits and tears). Typically, these injuries are caused by traumatic injuries or excessive stress. Often the pain appears gradually, for example, when raising your arm. If a person does not attach importance to this and continues to load the shoulder, the pain intensifies and symptoms such as swelling and overheating appear. In most cases, doctors provide conservative treatment for shoulder bursitis. Experienced shoulder specialists recommend rest, anti-inflammatory medications, and biological treatment based on cell technology in this case. Quite rarely, clinics perform surgical treatment to remove the inflamed bursa.
What is inflammation of the synovial bursa of the shoulder joint?
During painful bursitis, there is swelling in the area of the shoulder joint and an increase in the joint capsule, causing pressure on nearby tissues. The synovial bursa itself is an elastic, slit-like cavity filled with synovial fluid, capable of changing its shape between muscles, tendons and bone structures. In addition, the bursa allows painless movement of various tendons, bones and muscles within a highly mobile joint without friction. Bursitis in the shoulder is basically an inflammation of the periarticular bursa located between the head of the humerus and the acromion. Additionally, bursitis is the most common cause of stabbing pain in the arm. The subacromial joint capsule is the largest bursa in the human body, which is most often subject to inflammation of various types. Doctors use the term "subacromial" or "subacromial" bursitis when the area under the acromion of the collarbone (acromion) becomes inflamed.
Prevention
To prevent the development of pathology and prevent periarticular inflammatory process, it is necessary to follow certain rules:
- stick to a rational and balanced menu;
- provide the body with moderate physical activity;
- take walks outdoors;
- control body weight;
- Avoid repetitive physical activity that puts pressure on your hips;
- strengthen your immune system;
- maintain an active lifestyle;
- follow a daily routine, do not reduce rest time;
- wear comfortable and, if necessary, orthopedic shoes.
Anatomy of the shoulder joint: Position of the periarticular bursa under the acromion
Changes to the underlying supraspinatus tendon (eg, tears and calcium deposits) can distort the bursa.
Inflammation of the shoulder bursa can be caused by structural changes in the acromion, such as bone spurs. Therefore, in search of the causes of persistent bursitis, it is necessary to undergo a complete examination of all structures of the shoulder. © bilderzwerg / fotolia Inflammation of the periarticular bursa of the shoulder joint is characterized by swelling in the area of the subacromial bursa, located under the acromion. Muscles, ligaments, tendons and the bursa, that is, the soft tissues of the shoulder, are located close to each other. Thus, the largest bursa ensures the health of the supraspinatus tendon, the tendon between the shoulder blade and the head of the shoulder. If the load on the subacromial region is exceeded due to raising the arm above the head, pressure is also exerted on the supraspinatus tendon, which often causes inflammation and pain in the shoulder.
Complications
Complications of bursitis develop when the immune system is impaired or due to improper treatment. Then, as a result of tissue breakdown, the pathological process can spread to adjacent areas. Possible complications of the disease include:
- Abscesses and phlegmons are local or diffuse purulent cavities in the subcutaneous fatty tissue.
- Purulent arthritis is purulent inflammation of the adjacent joint.
- Osteomyelitis is a purulent-necrotic lesion of nearby bone tissue.
- Sepsis is the entry of purulent-necrotic masses and infections into the systemic bloodstream. Leads to purulent lesions and the formation of abscesses of internal organs, multiple organ failure and often ends in death.
Symptoms: Shoulder pain when raising your arm up
Symptoms:
- Pain when raising your arm up
- Pain when pressing on the shoulder and increased sensitivity
- Stitching pain upon final extension of the arm
- Night pain when lying down
- Weakened muscle strength
- Swelling, redness, hyperthermia
- Pain radiating from shoulder to arm
The pain caused by bursitis of the shoulder joint begins gradually and increases depending on the nature of the movements. As a rule, at the beginning of bursitis, patients complain of discomfort when raising their arms to the top.
If the patient does not attach much importance to his complaints and continues to lead his usual lifestyle, the pain gradually becomes stronger. If the shoulder joint begins to hurt suddenly, the cause is most likely not bursitis. Specialists who treat the shoulder joint strongly recommend not to put stress on the shoulder. Otherwise, the pain will become more and more powerful and will bring you discomfort even during rest. The shoulder's increased sensitivity to pressure can lead to severe pain at night. If the patient sleeps on an unhealthy shoulder, then the shooting pain can wake him up.
Shoulder pain due to bursitis is often accompanied by increased sensitivity on the outside of the shoulder.
When the shoulder joint's range of motion is completely exhausted, patients feel an unpleasant tingling sensation in the shoulder. Such sensations are observed when a person raises his hand above his head in order, for example, to dry his hair, comb his hair, or put on a jacket. People who constantly sleep on their sides also feel the negative effects of bursitis, since while sleeping on the sore shoulder, pressure is exerted on the inflamed mucous bursa. That is why shoulder bursitis is an unpleasant disease.
Repeated monotonous movements of the shoulder only increase the pain. Due to bursitis, pain may radiate towards the outside of the shoulder towards the elbow.
Unlike bursitis of the knee or elbow joint, inflammation of the bursa in the shoulder rarely causes external swelling or changes in the shape of the shoulder itself.
However, with extremely severe inflammation of the mucous bursa, the patient may experience redness of the shoulder joint. These not immediately noticeable signs are primarily concomitant phenomena of bacterial bursitis. Sometimes during bursitis a person's body temperature rises. Bacterial bursitis is also medically called “septic bursitis.”
Types of bursitis
In medicine, the disease is given several classifications. Types of the disease are distinguished by the location of inflammation, the composition of the exudate and the reasons that led to the development of the pathology. There are 160 bursae in the human body. But the bursae of large joints become inflamed more often:
- elbows;
- shoulder;
- knee;
- hip
Based on the composition of the exudate released into the capsule, serous, purulent, fibrinous and hemorrhagic bursitis are distinguished. In the first case, an almost transparent and quickly absorbable liquid accumulates in the bursa. In the purulent form of the disease, pus is released into it, fibrinous - fibrin, hemorrhagic - blood.
Bursitis can be primary or secondary. In the first case, there are no internal reasons that could cause it. Secondary pathology is usually a consequence of another disease - rheumatoid arthritis, psoriasis, diabetes, etc.
Causes of shoulder bursitis
Causes
- Impact, shock, injury
- Overload, especially during arm raising
- Monotonous movements
- Mature age
- Incorrect posture
- Impingement syndrome
- Diabetes
- Calcinosis of the forearm
Several circumstances contribute to the development of shoulder bursitis.
One of the most common causes is damage to the structure of the shoulder (trauma). A fall or blow to the shoulder can cause hemorrhage into the bursa and inflammation of the mucous membrane. Despite the fact that over time the body reduces the blood content in the bursa, inflammation of the mucous membrane on the outside of the mucous bursa remains for a long time. Thus, from a common injury, chronic bursitis of the periarticular bursa of the shoulder is formed. Doctors call this form of inflammation “traumatic bursitis.”
Another cause of bursitis is repeated pressure or excessive stress on the shoulder. In this case, the mucous bursa becomes inflamed due to repeated minor injuries, leading to the same results as hitting the shoulder on a hard surface. Painters, fitters, or people whose profession involves raising their arms above their heads suffer from this pathology more often than others. Athletes who perform powerful overhead movements, such as tennis or badminton players, report similar symptoms.
With age, the likelihood of developing bursitis due to traumatic injuries or excessive stress increases.
Incorrect posture is another cause of inflammation of the shoulder bursa. When the body is strongly bent forward, the scapula is pulled towards the top, which narrows the space under the acromion. If a patient comes to the doctor with such complaints, he is diagnosed with impingement syndrome of the shoulder joint and referred for treatment. If the subacromial area is narrowed for a long time, the mechanical pressure on the subacromial periarticular bursa and the tendon apparatus responsible for shoulder mobility (rotator cuff) increases. The interaction of these factors contributes to the development of the inflammatory process inside the synovial bursa.
Bursitis that has been treated for a long time can also contribute to the appearance of inflammation of the shoulder bursa.
Metabolic disorders of the shoulder joint can also cause bursitis: Calcification of the forearm (calcification of the supraspinatus tendon) often appears simultaneously with bursitis. Calcium deposits in the supraspinatus tendon can lead to rupture of the overlying subacromial bursa and long-term inflammation of the bursa.
Impingement syndrome is characterized by friction of the rotator cuff tendons against the acromion, which is the so-called roof of the shoulder joint. In addition, during humeroscapular periarthritis, bone spurs (osteophytes) are formed on the acromial process of the clavicle, causing ruptures and inflammation of the mucous membrane of the shoulder bursa.
Causes of the disease
Bursitis is usually infectious in nature. It can be caused by untreated inflammatory pathologies. Viruses and bacteria are often the causative agents, leading to the development of sinusitis, otitis, bronchitis, abscess or the formation of another source of infection.
The cause of the onset of the inflammatory process can also be:
- allergic reaction;
- poor circulation in the joint capsule;
- injuries of the synovial bursa or its vessels.
People at risk include people with low or excessive physical activity. In both cases there is an increased risk of injury. Therefore, inflammation of the joint capsule is more common among housewives, office workers, drivers, miners, and professional athletes.
Diagnosis and clinical examination of bursitis
Before starting treatment, an orthopedic specialist conducts a series of examinations to rule out certain causes of the disease. Inflammation of the tendons, impingement syndrome or arthrosis of the shoulder joint have similar symptoms. In some cases, these pathologies are also accompanied by additional inflammation of the periarticular bursa of the shoulder. Thus, medicine presents several causes of shoulder pain. High-quality diagnostics at the Gelenk Klinik medical center in Freiburg in Germany, based on advanced technologies, make it possible to establish the main cause of shoulder pain.
History: diagnostic consultation with a doctor
During the anamnesis, compiling a medical history, the doctor asks the patient several questions regarding his health:
- Previous and current diseases
- General state
- Diseases caused by metabolic disorders (eg diabetes, rheumatism or gout)
- Motor vehicle accidents or other incidents involving shoulder injuries
- Overloads and shocks
- Sports loads and features of professional activity
In this way, the doctor receives a complete picture of the possible effects, deficiencies and predispositions of the shoulder joint.
Physical examination and clinical examination
During the examination, the shoulder specialist pays special attention to the following aspects:
- Pain when pressed (increased sensitivity)
- Swelling
- Hyperthermia and skin color changes
- Features of posture
Special tests to determine the strength and mobility of the arm during movement in different directions indicate possible tendon ruptures and injuries.
Imaging examination of the shoulder joint: ultrasound, x-ray, MRI
Modern medicine offers several imaging diagnostic methods, each of which shows different aspects of the disease.
Ultrasound helps the doctor test the mobility of the muscles, tendons and soft tissues of the shoulder. Also, an ultrasound examination shows swelling and accumulation of excess fluid in the bursa. Ultrasound also shows structural damage to the shoulder, for example. tendon ruptures and inflammation. © Gelenk-Klinik
Ultrasound examination (ultrasound)
Ultrasound imaging shows accumulation of excess fluid in the bursa of the shoulder joint, as well as injuries to the ligaments and tendons during movement. In addition, ultrasound shows tendon ruptures and calcium deposits.
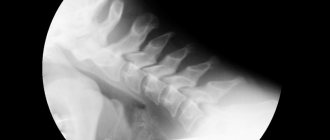
X-ray
An x-ray does not show the condition of the soft tissues: the image shows only the position and condition of the bones of the shoulder joint. This image shows sufficient space between the head of the humerus and the acromion. It follows from this that impingement syndrome is not the cause of inflammation of the shoulder bursa. Ultrasound allows the doctor to examine muscles, tendons and soft tissues during movement. In addition, an ultrasound examination provides information about the presence of edema due to the accumulation of excess fluid in the bursa. Tendon injuries and inflammation in the shoulder also become visible after an ultrasound.
This image shows sufficient space between the head of the humerus and the acromion. It follows from this that impingement syndrome is not the cause of inflammation of the shoulder bursa. © Gelenk-Klinik
MRI (Magnetic resonance imaging)
MRI (tomographic medical images) provide information about soft tissue damage, inflammatory processes, and structural changes in the shoulder joint. For the treatment of bursitis, MRI is not the main diagnostic method. If a patient is suspected of having inflammation of the mucous membrane of the bursa, specialists at orthopedic clinics first perform an ultrasound.
Before making a diagnosis of shoulder bursitis and starting treatment, it is necessary to conduct an imaging examination to exclude tendon ruptures and injuries to bone structures. MRI is performed only in the case of a complicated form of bursitis and helps make a final decision regarding the most appropriate form of treatment for the disease. Magnetic resonance imaging helps to choose the right method of surgical treatment and prepare for surgery.
In complex cases that are not amenable to conventional treatment, a very important aspect is to exclude injuries such as tendon ruptures and bone deformations using imaging diagnostics. Magnetic resonance imaging (MRI) is one of the most important methods for diagnosing shoulder bursitis.
Laboratory analysis of blood and joint fluid
Laboratory diagnostics
- Diabetes
- Gout
- Rheumatism
- Bacterial inflammation (septic bursitis)
- Arthritis
Movement problems are not always the cause of shoulder pain. The patient may also feel discomfort in the hand due to metabolic disorders that limit mobility and cause pain. Such pathologies include, for example, rheumatoid arthritis, an inflammatory autoimmune disease. A blood test shows the presence of rheumatoid factor, which allows you to confirm rheumatoid arthritis. In addition, a clinical blood test helps to exclude bacterial infections: With an increased number of leukocytes in the blood, the likelihood of disease increases.
Symptoms
If bursitis is not associated with injury, then the disease progresses from several days to several weeks.
Symptoms of bursitis are:
- swelling;
- increased temperature in the area of inflammation;
- pain and discomfort in the joint and area around the joint;
- pain on palpation;
- limited movement;
- skin redness;
If a joint is affected by bursitis, this area will be hot to the touch and discomfort will be felt upon palpation. In addition, a person will not be able to normally bend or straighten an arm, leg or other part of the body affected by the disease. In the morning, there may be limited movement and stiffness.
The inflamed bursa can increase significantly in size.
The entire range of symptoms will depend on the root cause that caused the disease, as well as the degree of the disease, the place where the bursa became inflamed.
If the bursa is located close to the skin, then common symptoms will be: swelling, redness and fever. For example, the outside of the heel, the elbow bursa at the very tip of that elbow.
With a deeply located bursa, swelling and hyperemia of the tissues will no longer be so pronounced; moreover, symptoms may be absent for some time at all. For example, vertebral bursa of the thigh, subacromial bursa of the shoulder.
Swelling may be less noticeable in people who are overweight.
If bursitis is of an acute type, then the pathology may develop unexpectedly, accompanied by acute pain, stabbing pain. At night, a person is tormented by shooting pains. When you feel the joint, you feel a seal, it is not hard, it is filled with liquid. It feels like a balloon filled with water. Movements are limited. There is heat in the area of inflammation, the joint area is hot.
Conservative treatment of shoulder bursitis
As a rule, inflammation of the periarticular bursa of the shoulder is treated conservatively, that is, without surgery.
Home remedies and home treatment
In most cases, patients can treat inflammation of the shoulder bursa on their own. However, if the pain does not stop and becomes stronger, you should immediately consult a doctor. Despite this, please note that home treatment is associated with certain risks: If you use home remedies, you may miss some important shoulder injuries or pathologies.
- Cooling compresses for acute shoulder pain.
- Anti-inflammatory medications (eg paracetamol or ibuprofen)
- Sports ointments (eg diclofenac)
- Anti-inflammatory and cooling curd compresses
- Applying aluminum acetate salt to the shoulder
In most cases, shoulder bursitis is treated with non-steroidal painkillers (NSAIDs). In addition, to restore the shoulder, orthopedic specialists recommend rest and cooling compresses to the patient. In the most difficult cases, injections of the anti-inflammatory hormone cortisone, as well as painkillers, help to immediately stop inflammation of the periarticular bursa and associated shoulder pain.
Physiotherapy and biological treatment based on cell technologies
If drug treatment does not bring the desired result and the patient continues to feel pain, the doctor refers him to physiotherapy or exercise therapy. One of the main specializations of the German medical center Gelenk Klinik in Freiburg is regulatory therapy based on cell technologies. The use of vibration therapy in medical practice helps stimulate metabolism in the inflamed synovial bursa of the shoulder joint, which helps to overcome inflammation in the shortest possible time.
Matrix therapy consists of several modules that interact to stop the development of the inflammatory process and tissue health. This image shows biomechanical stimulation (BMS) of the shoulder muscles using a vibrating device. This technique helps treat injuries, inflammation and structural disorders of the shoulder tendons. Inflammation of the mucous bursa is one of the main indications for this treatment. © gelenkreha.de
Therapeutic process
Treatment of the pathology comes down to keeping the patient at rest, doing physical therapy, and taking anti-inflammatory drugs. If the disease takes a protracted form, then physiotherapy, injection of glucocorticosteroids, and surgery are prescribed.
The starting point of the therapeutic process is taking anti-inflammatory drugs while eliminating movements that cause pain. As soon as acute pain symptoms have been effectively relieved, the course includes scratch exercises aimed at stretching the iliotibial band and tensioning the fascia lata. It is also important to strengthen your gluteal muscles. Exercises should be determined by the attending physician, taking into account the patient’s condition.
If the therapeutic process is not effective, physiotherapy is prescribed. Popular methods are electrophoresis and ultrasound therapy. To enhance the result, injections of glucocorticosteroids into pain points are prescribed. This complex of effects helps to get rid of the problem.
Among the methods of physiotherapy, magnetic therapy, laser therapy, decimeter wave therapy, transcutaneous electroanalgesia, and naphthalene applications can be prescribed. However, their effectiveness is questionable in the treatment of bursitis, since they provide only weak maintenance of the spontaneous manifestation of remission. There is no proven result of using extracorporeal shock wave therapy for bursitis.
In some cases, pain does not go away after conservative treatment, which is the basis for prescribing surgical intervention. For example, trochanteric bursitis can be treated surgically in several effective ways, which will allow the athlete to return to training and sports within a few months after the manipulation.
During exacerbation of bursitis in the early stages of progression, patients are prescribed rest and wearing a pressure bandage. Compresses with a warming effect can also be used. Early treatment of the serous type of acute bursitis using bandages for fixation will help prevent the development of the disease in a purulent form.
The chronic development of bursitis is surgically treated with punctures, during which the exudate is removed and the cavity of the bursa is washed with a solution containing antiseptic components or antibiotics. The traumatic type of bursitis requires the injection of a solution with hydrocortisone into the synovial bursa. The course includes 2-5 procedures daily, 25-50 mg. Antibiotics are included in the solution. Pre-introduce 8-10 ml of 2% novocaine.
Purulent bursitis can be cured by punctures. If the pathology progresses, the bag is opened, from where the purulent masses are removed. Treatment of the wound is carried out according to the general standard scheme. In this case, the surgical wound heals for quite a long time.
The prognosis for the development of acute bursitis is determined by the degree of abnormal abnormalities in the bursa, the spread of the disease, the activity of the infection, and the patient’s immunity. Complicated progression of the pathology, along with which signs of arthritis, osteomyelitis, fistulas or sepsis appear, is associated with the likelihood of a negative prognosis.
Minimally invasive surgeries of the shoulder joint for inflammation of the periarticular bursa
Only in cases where drug treatment for shoulder bursitis, as well as physical therapy, have been unsuccessful and a person continues to feel tingling in the shoulder, does there become a need for surgical treatment of subacromial bursitis. We draw your attention to the fact that treatment of bursitis of the shoulder joint is carried out using arthroscopic minimally invasive techniques. This operation, during which the surgeon completely removes the inflamed joint capsule, is performed through the so-called “keyhole”.
Shoulder arthroscopy is a minimally invasive surgery for shoulder pain, for which the surgeon uses microscopic instruments with a diameter of 0.5 - 1 cm. An arthroscopic camera helps the doctor obtain a limited but accurate image of the surgical site. This intervention consists of aspiration (suction) of the contents from the joint capsule. In addition, in parallel, the surgeon can treat diseases that cause bursitis, such as impingement syndrome or calcification of the forearm. © bilderzwerg / fotolia
Additional operations when removing a bursa (bursectomy)
Additional interventions
- Removing calcium from the supraspinatus tendon
- Acromioplasty
- Suture placement of the supraspinatus tendon
In addition to the operation, the specialist examines and, if necessary, begins treatment of all structures of the shoulder joint. Thus, if bursitis is suspected, calcium deposits from the supraspinatus tendon, as well as bone spurs under the acromion, can be removed during arthroscopy.
Shoulder arthroscopy: Postoperative treatment and prognosis
After surgical removal of the periarticular bursa of the shoulder (bursectomy), a new bursa is formed in the same place within a short time, performing the functions of the removed tissue in full.
Motor functions of the shoulder are restored a few days after the operation. The pain syndrome disappears immediately.
Almost immediately, the patient can move the shoulder as before and return to previous activities. The stitches are removed after about 10 days.
Make an appointment
Diagnostic procedure
Diagnosis of hip bursitis is made based on the patient’s existing complaints. The doctor takes into account all the symptoms, localization and nature of the pain syndrome, the frequency of its occurrence. The diagnosis is clarified by palpating the affected area and performing the Ober test.
The specialist prescribes examinations in the following areas:
- a general blood test to identify signs of inflammatory changes;
- MRI;
- ultrasound diagnostics;
- history taking and examination;
- performing radiography;
- CT;
- performing a puncture with laboratory tests of the collected material;
- performing angiography of the circulatory system within the inflamed area.
The diagnostic process is complicated by the similarity of symptoms with manifestations of other inflammatory pathologies, for example, arthritis and synovitis. In addition to this, pathologies can develop in parallel, so it is not easy to determine the original cause of the pathological process.