The knee is a large joint with a large and constant load. It is not surprising that injuries often occur here and the risk of knee joint diseases is high. Periodic knee pain bothers almost 50% of people at the age of 40, and by the age of 70 it becomes a constant companion. One of the common pathologies of this joint is bursitis of the knee joint. In this case, the periarticular sac becomes inflamed and fluid accumulates in it. Movement becomes limited and painful. Doctors at the Kuntsevo Medical and Rehabilitation Center know how to recognize and treat bursitis. The clinic’s specialists are ready to help with acute and chronic forms of the disease using the most modern, safe and effective methods.
Knee bursitis and its types
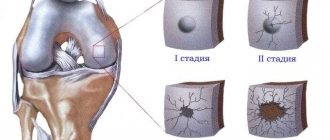
The term “bursitis” is applied to the inflammatory process that occurs in the anatomical structure of the joint – the bursa.
This is a kind of hydraulic airbag - a cavity made of dense connective tissue that protects the joint from external damage. On the outside, it consists of dense tendons and ligaments that provide a durable outer covering. Inside is a layer of cells that produce synovial fluid. This is a special joint lubricant that facilitates the sliding of bone heads in it, protects tendons from friction, nourishes and moisturizes joint tissues. When moving, cartilage, like a sponge, absorbs this liquid along with nutrients.
The knee is a complex joint, in which there are several synovial bursae: above, below and in front of the kneecap, on the lateral ligaments, tendons, heads of the gastrocnemius and popliteus muscles. Inflammation can appear in each of them or in several at the same time.
Bursitis occurs at the site of inflammation:
- Anterior kneecap - prepatellar - inflammation and swelling occur as a result of diseases such as rheumatism, gout and from constant injury. For example, when working specifically with frequent support on the knee. Maid's or priest's bursitis is what they call this type of pathology, in which the front of the knee swells.
- Popliteal – the tendon bursa in the lower part of the kneecap becomes inflamed. A typical cause for this type of pathology is falls and strong impacts to the knee, injuries and tears of the meniscus. Traumatic bursitis of the knee joint is common in people with arthritis or excess weight.
- Goose - or Baker's cyst. Inflammation occurs in the inside or back of the joint. It manifests itself as pain in the knee when moving, walking up stairs, and more often affects overweight women.
Knee bursitis is classified according to its course:
- Acute – occurring suddenly, with noticeable and intense symptoms and lasting up to a month.
- Subacute.
- Chronic – lasts up to a year.
- Recurrent - periodically worsens.
According to the type of cause, bursitis occurs:
- Aseptic is a non-infectious pathology caused by injuries (post-traumatic bursitis of the knee joint), gout, and autoimmune diseases.
- Septic – caused by bacteria or infections (tuberculosis, syphilis and others).
According to the type of accumulated synovial fluid: serous, purulent and others.
An accurate classification of bursitis is needed to understand its cause and which treatment methods will be effective.
Classification
Knee bursitis is classified into several types. In accordance with the clinical course, the pathology can be: chronic, subacute and acute.
Depending on the pathogen that became the source of the problem, bursitis can be nonspecific and specific (against the background of tuberculosis, gonorrhea, syphilis, brucellosis). In this subgroup, the disease is in turn divided into infectious and aseptic (non-infectious).
Depending on the nature of the liquid contents in the bag, the disease occurs:
- hemorrhagic - exudate contains red blood cells in a significant volume;
- serous - the liquid secretion contains plasma mixed with blood;
- purulent - the liquid contains destroyed leukocytes and cellular tissue, bacteria;
- fibrinous - the exudate contains an increased amount of fibrin.
Symptoms
General signs of bursitis of the knee joint (they will appear when different joint capsules are affected) include:
- Pain – bothers you at rest or when moving: running or walking up the stairs. Pain with bursitis of the knee joint most often occurs in the morning and gradually increases with increasing strength or intensity of exercise.
- Swelling – of the knee as a whole or of a specific joint capsule.
- A rise in temperature – both local (a feeling of heating appears in the knee) and in body temperature as a whole.
- Limitation of the possibility of movement - from slight stiffness and pain (the leg bends and unbends worse) to the complete inability to transfer body weight to the leg and walk normally.
- Signs of general intoxication during infections and purulent inflammation.
- Local symptoms of bursitis of the knee joint: swelling and pain in the area of the inflamed bursa.
Application of a knee brace
As an additional therapeutic device for bursitis, you can resort to using a new device - a knee brace. It helps stimulate local blood circulation due to the influence of a certain spectrum of radiation.
The device affects the body with rays similar in range to solar radiation. Thanks to this, additional energy is produced, which the body receives and uses for accelerated tissue repair.
Since the device acts locally, the penetration of the energy flow is noted deep into the tissues of the synovial bursa, which accelerates the elimination of toxic substances and stimulates the growth of new tissues, as well as increasing their elasticity.
Causes
The main causes of knee bursitis:
- Knee injuries range from severe (from falls, impacts) to microtraumas due to regular physical activity on the knees.
- Excessive physical activity due to obesity, carrying heavy objects, and playing strength sports.
- Diseases in which salts are deposited in the joint in the form of microcrystals.
- Arthritis of various natures (rheumatic, psoriatic and others).
- Spread of bacterial infections.
- Autoimmune diseases.
- Arthrosis of the knee joint (gonarthrosis).
- Malfunctions of the endocrine system.
Factors provoking the development of the disease
As a rule, knee bursitis is formed under the influence of the following factors:
- Regular and prolonged physical activity that involves the knee joint, or if excessive pressure is applied to this area.
- A targeted blow, falls on the knee.
- Infection of a wound on the knee.
- Increased tension in the knees due to excess weight.
- Against the background of diseases of infectious origin (syphilis, tuberculosis, brucellosis, gonorrhea, etc.).
- Against the background of extreme training (when the risk of injury is increased).
The joint tissue in the knee can become inflamed both in people actively involved in sports and in the average person. The cause of the problem may lie even in minor injury.
Diagnostics
Consulting a doctor will help confirm bursitis. Inspection of the joint, palpation and a series of tests will be required. Moreover, with bursitis of the right knee joint, you need to pay attention to the left knee (and vice versa). An orthopedic traumatologist evaluates pain, swelling and other signs, asks you to make some movements to understand what exactly causes the most pain and where the inflammation occurs.
Instrumental diagnosis of bursitis:
- Ultrasound – for visualization of periarticular tissues, the meniscus, the amount and nature of intra-articular fluid, the location and boundaries of inflammation.
- MRI is the most informative method for diagnosing soft tissues.
- X-ray (an alternative to computed tomography) - assessment of bone structures - the presence and foci of their degeneration and destruction.
- Diagnostic puncture - collection and laboratory examination of fluid.
Laboratory diagnostic methods:
- Tests to look for diseases that could cause bursitis.
- A blood test for general and specific indicators that will indicate the autoimmune nature of bursitis.
- Analysis of joint fluid.
Prevention
Treatment of bursitis is a complex and lengthy matter. To prevent relapse, it is necessary to follow general recommendations for preventive purposes. To do this you need:
- limit heavy lifting;
- visit the pool;
- refuse strength training, visit the gym only under the supervision of a trainer with a medical education;
- monitor your body weight (every kilogram of excess weight increases the load on the supporting joint 10 times);
- undergo regular diagnostics;
- take complexes of vitamins and minerals to strengthen bone tissue;
- increase immunity and body resistance.
Treatment of knee bursitis
Both conservative methods and surgical interventions are used.
Conservative treatment:
- Medicines – for the treatment of bursitis of the knee joint, taking into account its cause, the following can be used: anti-inflammatory drugs, painkillers, antibiotics (in tablets, gels and ointments or injections). The course of taking prescribed medications is 5-7 days. If the clinical picture remains without positive changes, the drugs are changed.
- Puncture - a puncture is done to remove accumulated intra-articular fluid and rinse the cavity of the bursa with anti-inflammatory drugs. In case of purulent inflammation, drainage is installed for the internal cavity of the joint in order to remove the accumulating pus out.
- Physiotherapeutic procedures - techniques such as laser, ultrasound, magnetic, electro-, shock wave therapy activate blood circulation and lymphatic drainage, reduce inflammation, swelling and pain, accelerate healing processes, and “break up” salt deposits. One effective way to relieve swelling and pain is to apply a cold compress.
- Therapeutic physical education - classes using an individual set of exercises (and preferably under the supervision of a doctor or exercise therapy instructor) speed up recovery.
The operation is the opening and even removal of the inflamed bursa if conservative procedures are unsuccessful and an abscess or phlegmon develops (spill of purulent contents beyond the bursa and “melting” of its walls).
Exactly how to treat knee bursitis will differ depending on the type of pathology. So, in case of acute bursitis, which has developed for the first time, it is necessary to ensure temporary immobility in the joint (at least reduce the load). This will be helped by supporting bandages, wearing an orthosis, taping, temporary refusal or reduction of physical activity.
With chronic inflammation, joint immobility is less important. In this case, more attention is paid to an individually selected set of physical therapy exercises and the prescription of anti-inflammatory drugs.
In case of septic inflammation, it is necessary to act on the causative agent of inflammation. You cannot do without antibiotics and (in many cases) without drainage of the joint cavity.
Complications
Any form of bursitis leads to severe complications. Untreated acute bursitis can provoke the development of an acute purulent process when the surrounding tissues are affected by pathogenic bacteria. Arthritis develops, which limits a person’s movements and does not allow him to fully engage in sports. When the acute phase becomes chronic, further discomfort and constant pain force a person to leave sports and stop engaging in his favorite profession.
If you start self-medicating and do not consult a doctor in time, you can bring the process to a sad state.
Where to treat bursitis in Moscow
A quick and accurate diagnosis of diseases of the musculoskeletal system (including joints) will be carried out at the Kuntsevo Treatment and Rehabilitation Center. For this we have all the necessary equipment and doctors with extensive experience.
We are ready to offer the safest and most effective treatment methods. The clinic has a specially equipped day hospital for minimally invasive procedures and a physical therapy room with all the necessary exercise equipment. Classes are held in small groups or individually.
Book a consultation by phone.
When to make an appointment and see a doctor
If you have symptoms of knee bursitis, bursitis of the elbow joint, finger, or shoulder, you should immediately contact the clinic. The sooner the diagnosis is made, the greater the chances of a complete cure of the disease.
We recommend that you make an appointment immediately if you experience:
- joint pain when walking or at rest;
- swelling;
- chills and fever;
- mobility restrictions.
Remember that treatment of joint bursitis is a long process that requires an integrated approach. We do not recommend using the advice of other patients from thematic forums, since each case has its own treatment algorithm. It depends on the causes of the disease, the stage of its development and concomitant chronic diseases.
How to make an appointment with an orthopedic traumatologist?
Bursitis is treated by a professional specialist - an orthopedic traumatologist. Carry out a diagnosis of bursitis, get a consultation with a doctor at JSC "Medicine" (clinic of Academician Roitberg) in the center of Moscow at the address: 2nd Tverskoy-Yamskaya Lane, 10. From the Mayakovskaya metro station you need to walk 5 minutes.
To make your first appointment with a specialist, please call. Calls are accepted 24 hours a day.
You can also submit an application through a short electronic form on the website. Don't forget to include your name and contact number for communication. The clinic administrator will call you back and make an appointment for you at the next available time.
Clinically Relevant Anatomy
The patella is a triangular bone located in the anterior part of the knee joint. When you bend or straighten your knee, it slides into the intercondylar groove of the femur. The patellar tendon is a tough structure that connects the underside of the patella to the tibia. The top of the patella is connected to the quadriceps muscle, which extends the knee and moves the patella upward. The bursae around the knee can be divided into two groups - those that lie around the patella (the suprapatellar bursa, the superficial and deep infrapatellar bursa, and the prepatellar bursa) and those that lie elsewhere (the pes anserine bursa and the iliotibial bursa).
Epidemiology
Prepatellar bursitis occurs more often in men than women and can occur at any age. 80% of people with prepatellar bursitis are men aged 40 to 60 years. In 1/3 of cases, prepatellar bursitis is septic in nature and in 2/3 it is non-septic. Infectious prepatellar bursitis occurs more often in children than in adults. Prepatellar bursitis is quite common, with an annual incidence of at least 10/100,000. The incidence of prepatellar bursitis is probably underestimated because most cases are not septic and only patients with the most severe conditions require hospitalization.
Why is synovitis dangerous?
The synovial membrane performs an important function in the joint - it ensures the separation of hard tissues. Due to this, the joint moves with minimal bending of the components. The membrane is capable of changing shape, thereby adapting to supporting surfaces and providing shock absorption. The quality and quantity of synovial fluid in the joint depends on its condition, the same fluid whose deficiency develops coxarthrosis or gonarthrosis.
The connective tissue that forms this membrane can become inflamed. Swelling forms in the joint, during movement the person feels pain, and bleeding is possible. If the disease is not treated, the synovial membrane thickens and new blood vessels appear in it. In the future, this will lead to frequent joint bleeding.
Synovitis without treatment can lead to joint dysfunction
What is tenosynovitis
Tenosynovitis is an inflammation of the tendon sheaths. The latter are tubular-shaped connective tissue filled with liquid lubricant. The sheaths surround the tendons, which are made of flexible fibrous collagen tissue. It is what attaches muscles to bones. If the outer covering of the tendons becomes inflamed, it is called tenosynovitis. Both inflammatory diseases are accompanied by pain when moving, so only a doctor can make an accurate diagnosis.
Tenosynovitis most often affects the hands, wrists and feet