Osteochondritis dissecans (Koenig's disease) is a phenomenon that represents the necrosis of the bone area under the articular cartilage.
The affected tissues covering the bones begin to slowly peel off, sometimes completely separating from the bone, provoking the formation of an inflammatory process and free intra-articular bodies.
The disease often occurs in males (age category 15 - 30 years).
Older men and women are also susceptible to the disease.
The localization of the process in the lateral condyle varies in 9-12% of cases; in the medial condyle - up to 75-85% of cases and the lesion is localized in the patella in up to 5% of cases.
What is Koenig's disease (osteochondritis dissecans)
Koenig's disease (osteochondritis dissecans) is a pathological process that occurs in the area of the subchondral bone plate, against the background of which there is destruction of the cartilage in the immediate vicinity and degenerative changes in the bone. The undesirable consequences of this disease include osteoarthritis, which consists of inflammation, deformation and impaired mobility of the joints.
Most often, osteochondritis dissecans is diagnosed in several areas of bone tissue formation. It is characterized by slow tissue necrosis. This pathological process involves cartilage and the bone itself, but at the initial stage the subchondral bone plate suffers.
The first mention of osteochondritis dissecans of the knee joint can be found at the end of the 19th century: in 1840, surgeon Joseph Malgaigne (France) announced the possibility of excision of pathologically altered cartilage and bone tissue from the knee area, and in 1870, British pathologist James Paget defined the pathology as “ silent necrosis."
Stages of pathology
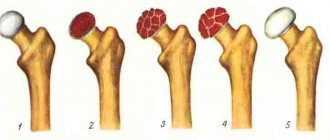
Depending on the degree of degeneration, there are 4 stages of osteochondritis:
- A focus of necrosis is formed. The patient has an unexpressed aching pain syndrome; in the projection of the knee in front, slight local swelling is possible, soft to palpation. During diagnosis, cartilage defects, changes in its structures and tissue heterogeneity are noted.
- Clear boundaries of the pathology appear in the form of cartilage deformation and osteochondral changes with inflammatory effusion (synovitis). The patient feels increased acute pain with clear localization and swelling with hyperthermia. One third of patients continue to report pain of unclear localization.
- The cartilage partially peels off and begins to “ballute”, capturing the subchondral layer of the bone. The joint ceases to perform its functions.
- The cartilage is completely torn off and begins to move in the joint capsule, causing a “jammed joint.”
In childhood and adolescence, two knee joints are often affected at once, in older age – only one.
The pain is localized in 80% of cases only in the anterior (frontal) part of the knee joint, and in 20% - in the frontal medial part. Up to stage 3, it occurs during physical activity and sudden movements. When synovitis appears, the pain syndrome becomes diffuse.
At the site of injury, swelling swells, the skin above it becomes hot (hyperthermia) and redness is observed (hyperemia). The patient’s general condition worsens already at the second stage: an increase in body temperature to subfebrile (37.5°C), weakness, dizziness and drowsiness occur. When the first symptoms appear, you should consult a doctor, because only timely therapy can stop the destruction of the joint.
Causes of development of Koenig's disease
Until now, the exact etiology of the appearance of osteochondritis dissecans of the knee joint has not been studied. One of the most obvious factors causing the disease is circulatory disorders. This limits the sufficient flow of nutrients to the articular cartilage area and impairs metabolic processes. Due to the gradual development of the disease, it is not possible to clearly name its causes.
If we talk about predisposing factors for the occurrence of Koenig's disease or osteochondritis dissecans, then these include:
- Arterial diseases;
- Inflammation of the inner lining of the venous walls in the lower extremities, formation of deep vein blood clots;
- Congenital anomalies in the area of cartilage and bones;
- Dislocations, fractures and sprains of the knee joint;
- Complications in the postoperative period;
- Endocrine pathologies;
- Chondromatosis of the joints.
There are also risk factors that can worsen the course of the pathological process:
- Males;
- Patients in the age category up to 30 years;
- Excessive consumption of alcoholic beverages and tobacco products;
- Heredity;
- Obesity;
- Increased and prolonged stress on the legs resulting from heavy physical labor or professional sports activities;
- Long-term exposure to toxins from activities in hazardous industries.
Pathogenesis
Despite the fact that diagnosed cases are found in modern medical practice, the pathogenesis of osteochondritis dissecans remains incompletely understood.
Today, there are a large number of assumptions, each of which makes it possible to form a more or less complete picture. So, there are several theories. Let's try to look at a few of them.
Inflammatory processes
A large number of specialists around the world are inclined to believe that the pathogenesis of the disease in question lies precisely in inflammatory processes, which is confirmed by several histological samples. Thus, one of the authors described 24 such cases, while another noted 42 cases in 12 months.
It is worth noting that a fairly large number of histological analyzes were carried out, which, in the presence of symptoms, did not at all show the presence of inflammatory changes.
The theory about the origin of pathology from inflammation has no scientific or literary support.
Injuries
Two other American scientists noted 14 cases of pathology in which there was an assumption that the progression of tissue deterioration could be caused by injuries (both acute and chronic).
Considering this theory, one can trace a fairly obvious connection: pathological processes originate in the most vulnerable place of the joint, damage to which is extremely difficult to diagnose. Over time, bone tissue is destroyed, which causes necrosis and separation of the osteochondral fragment.
Systematic microtraumas
When talking about injuries, one should not ignore such a situation as microtrauma. Despite the apparent insignificance, repeated damage to tissue integrity (for example, minor blows to a limb) may well lead to very serious consequences.
Hereditary predisposition
A huge number of scientific works are devoted to the study of genetic factors.
Despite the large number of studies conducted, as well as the endlessly relevant discussions of medical workers around the world about the influence of the genetic factor, there is no exact confirmation of the existence of a connection between the formation of osteochondritis dissecans and heredity.
Ischemia (decreased vascular nutrition)
As you know, lack of blood circulation can lead to extremely negative, sometimes even irreversible, consequences. Thus, in connection with the results of numerous studies, the study of diagnosed cases and taking into account a number of other factors, a significant reduction in the number of vessels was noticed.
Considering this issue theoretically, we can come to the conclusion that circulatory disorders can be caused by various factors, for example, various types of trauma or abnormalities of the cardiovascular system.
Symptoms of Koenig's disease
As stated earlier, this pathology is characterized by gradual development. Moreover, Koenig's disease of the knee joint occurs in the same way in both children and adults. At the initial stage, the patient feels pain in the joints, which is of a volatile nature: they are of low intensity and stop after a long rest. The severity of the disease is often influenced by inflammation of the synovial membrane of the joints. In adults, it is accompanied by swelling in the knee joint, which is a consequence of the accumulation of fluid in the internal cavity, as well as redness and burning of the skin in this area. In children, this pathological process may be accompanied by general intoxication: pain in the head, difficulty in the digestive tract and fever.
As the disease develops, pain increases, which over time makes itself felt even at rest. As a result of pinched muscles, stiffness occurs. To prevent discomfort, patients often limit physical activity.
Make an appointment Online booking
- Clinic on Krasnopresnenskaya +7 (499) 252-41-35 Volkov lane, 21
- Clinic on Varshavskaya +7 (499) 610-02-09 Varshavskoe highway, 75, building 1
- Clinic in Annino +7 (495) 388-08-08 Varshavskoe highway, 154, building 1
Types and stages of Koenig's disease (osteochondritis dissecans)
The classification of the disease is based on the age factor, the results of X-ray examinations and arthroscopic examination of the joint.
Today, two types of osteochondritis dissecans are known: adult and juvenile. In the first case, there is injury to the joint, in the second, a violation of the development of the expanded section of the tubular bone.
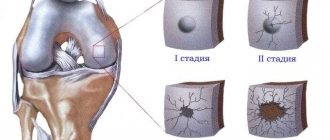
Next, you will get acquainted with the classification based on the anatomical characteristics of the affected area. The following stages of the disease are distinguished:
- First stage. The radiograph shows the lesion. MRI and CT images show a sclerotic line, but there is no damage to the articular cartilage;
- Second and third stages. A crack and a split-off part forms on the cartilage tissue;
- Fourth stage. Symptoms of the degenerative process in the cartilage make themselves felt, and the osteochondral fragment changes its position.
How does Koenig's disease develop?
By analogy with arthrosis, this disease also has several stages.
In the first stage, minor discomfort appears, the pain is localized in the knee, the cartilage is not yet deformed, but damage to the bone marrow has already begun.
On the second, more areas with dead tissue are formed, and the symptoms intensify. The synovial membrane becomes inflamed, and the destruction of cartilage begins.
In the third, the dead area of tissue is separated from the bone, the symptoms intensify even more, and mobility is limited due to severe pain.
In the fourth stage, the affected tissues form a separate substance in the synovial bursa and cause a strong inflammatory process.
Koenig's disease develops over many years
Diagnostics - MRI and ultrasound for osteochondritis dissecans
In order to more accurately diagnose osteochondritis dissecans of the knee joint and select the correct treatment, experts recommend undergoing the following diagnostic measures:
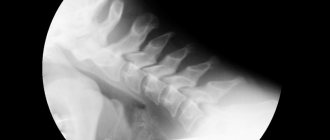
- X-ray. The highest information content is possible only at stages 3-4 of the disease;
- Ultrasound and MRI of the knee joint. They are also highly informative and allow diagnosis to be made at the initial stages of the disease;
- CT. Allows you to detect the disease at 2-3 stages;
- Athroscopy. This method is famous for its increased reliability and reliability. Provides an opportunity to study the condition of the outer shell of the joints;
- Analysis of rheumatoid indicator. Allows you to determine the likelihood of rheumatic changes in the joint.
Brief Definition
Before you understand what the prerequisites and symptoms of the pathology in question are, you should first understand, at least in general terms, what this disease is.
Koenig's disease is nothing more than osteochondritis dissecans of the knee. The disease has a fairly extensive clinical picture and belongs to the category of pathologies of a focal, idiopathic type.
As the pathological condition progresses, the patient's subchondral bone tissues are affected, which leads not only to a loss of cartilage stability, but also to its gradual destruction, leading to necrosis and pathological changes in the bone.
The impossibility of timely diagnosis, lack of treatment and neglect of prevention and therapy can provoke the premature development of osteoarthritis of various stages.
Any person on the planet is susceptible to Koenig's disease, regardless of age and gender. In the vast majority of diagnosed cases, the pathology develops in young adolescence. Despite the large risk group, it is worth noting that statistics show that diagnosis occurs in 21 cases out of 100,000.
Nuances of the manifestation of pathology in children
A juvenile form of the disease, which is characterized by asymptomatic manifestations or bilateral lesions.
Through the use of innovative diagnostic methods and periodic examination of the state of the body of children, this pathology can be detected at the initial stage - during the period when the use of conservative procedures gives the maximum positive result.
With timely implementation of treatment measures, the patient can count on full restoration of health. Patients in the teenage age group deserve special attention, since the effect on insufficiently formed structures is considered more noticeable. Surgery for Koenig's disease of the knee joint is required only in advanced situations.
Diagnostics
The initial stage of the study is reduced to X-ray diagnosis of the knee joint. By examining x-rays, the doctor can easily determine the degree of damage to the joint tissue, the stage of development of the disease, and will also be able to select the correct treatment method. However, X-rays are powerless against Koenig's disease, which is at an early stage of development.
To identify visible defects in cartilage and bone tissue, MRI is used, if necessary with a contrast agent. The contrast agent is administered intravenously/intra-articularly. Damaged and healthy areas react differently to the drug (displays MRI).
Ultrasound is considered to be quite effective among instrumental diagnostic methods.
diagnostics.
CT makes it possible to most accurately determine the location of the osteochondral defect, as well as the area and depth of bone damage.
Modern traumatology also uses endoscopic methods for diagnosing diseases of the knee joint. Athroscopy is considered an effective way to identify affected tissue areas.
The method involves inserting an endoscope (a device equipped with a light emitter or a miniature camera) into the cavity of the knee joint. Thanks to a device (arthroscope), the doctor has the opportunity to examine the patient’s joint apparatus in detail.
Koenig's disease and the army
If we talk about problems directly related to the knee joint, then the following pathologies occur:
- A purulent-necrotic process developing in the bone and bone marrow;
- Condition of lack of range of motion in the collarbone, joint or patella;
- Stable contracture of one of the joints with a slight limitation of motor ability;
- An increase in the length of the Achilles tendon, tendon or patellar ligament, which is acquired. In this case, the motor activity of the joint is significantly weakened.
Treatment of osteochondritis dissecans of the knee joint (Koenig's disease)
The duration of conservative procedures reaches 12-18 months. In this case, the patient is recommended to completely eliminate excessive stress on the joint and refuse sports activities. In addition, experts advise resorting to the help of elastic prosthetic devices - orthoses and knee pads. They promote strong fixation of the joint, prevent the possibility of deformation and accelerate recovery processes.
Radioisotope scanning is also regularly performed during all treatment procedures. This examination allows us to study the ability of cartilage to recover. Based on its results, the doctor has the opportunity to adjust the treatment plan.
Use of medications
Since the key factor in the progression of Koenig’s disease is circulatory impairment, at the initial stage of treatment it is advisable to use drugs to stabilize it (Eufillin and Pentoxifylline). The main purpose of their use is considered to be: relief of pain, restoration of normal well-being, removal of edema, elimination of the inflammatory process in the area of the synovial membrane. This means that if a patient is diagnosed with osteochondritis dissecans, treatment involves the use of non-steroidal anti-inflammatory drugs (Diclofenac, Diclofenac, Voltaren, Meloxicam, Nimesulide). To calculate the dosage, the body weight and age of the child are taken into account.
For the purpose of partial regeneration of cartilage tissue in adults, it is recommended to use Dona, Teraflex, Artru, etc.
Physical therapy for Koenig's disease
After relief of the inflammatory process and acute pain, the patient is recommended to engage in physical therapy. Also, physical exercise is indicated during the rehabilitation period after surgery. At the same time, when drawing up a treatment complex, the specialist takes into account the severity of the disease and the degree of its manifestation.
At the primary stage, post-isometric relaxation is used. Next, the patient is recommended to proceed to the following exercises:
- The patient assumes a “sitting” position, and then alternately flexes and straightens the lower limbs;
- Lunges;
- The patient raises his knees high and walks around the room
As a result of these exercises, it is possible to restore normal blood circulation in the joint area, increase the number of movements and strengthen the muscle.
Therapeutic massage for osteochondritis dissecans
If a patient is diagnosed with Koenig's disease, treatment involves the use of various massage techniques. In this case, cupping, acupressure and classic massage can be used, allowing to completely restore the functions of the knee joint and strengthen the muscle tissue in this area.
When performing massage procedures, the specialist acts on the areas where the muscles are located, and not on the cartilage and bone structures. At the initial stage, he makes light kneading and stroking movements, after which he moves on to more severe vibrations and intense palpation.
Physiotherapeutic treatment
During the rehabilitation period, the patient is referred to MRI, laser, UHF, UVT, galvanotherapy and ultraviolet irradiation procedures. It is also advisable to conduct electrophoresis using drugs that promote the restoration of cartilage tissue and B vitamins. The therapeutic effect is based on the impact of low-power current pulses on the knee joint area. This helps accelerate regeneration and metabolic processes.
Shock wave therapy for Koenig's disease
Due to exposure to low-frequency acoustic pulses (UAP), it is possible to improve the nutrition of the subchondral bone plate.
New vessels appear in it, participating in the exchange of substances between blood and tissues. This improves the supply of nutrients to bone tissue, and through it, cartilage.
Thanks to the processes described above, it becomes possible to prevent connective tissue dysplasia and restore the natural structure of the joint surface.
Exposure to shock waves is recommended to be performed both at the initial stage of the disease - in order to exclude subsequent surgical intervention and eliminate painful manifestations, as well as during the rehabilitation period after surgery - to speed up the patient's recovery process.
In general, the treatment course includes 8-10 procedures, once a week. This technique can be used simultaneously with other methods of exposure and is completely safe for the patient’s body.
In medicine, shock wave therapy is one of the priority methods in the treatment of Koenig's disease and the elimination of other pathologies in the area of the knee and ankle joint. At the same time, we use innovative Swiss equipment and provide a personal approach to each visitor. In addition, we provide flexible discounts on the services provided.
Surgery for Koenig's disease
The technique of performing the intervention differs between adult patients and children. This is due to different rates of regenerative processes. For example, conservative therapy is most often used for children, while for adults, surgical intervention is the most effective.
It is performed after the “articular mouse” is formed. To excise it, they resort to metal clamps. The key goal of surgical treatment is to recreate the shape of the adjacent articular parts in full compliance with each other. In this case, minimally invasive intervention is allowed, and an open method is also performed.
In our clinic, in addition to UVT, surgical intervention is also performed. This procedure is carried out by high-class specialists, which guarantees a successful result and ensures a shortened rehabilitation period. This means that even if you are diagnosed with severe osteochondritis dissecans, we are able to guarantee effective treatment and complete recovery of the body.
Traditional methods of treatment
Traditional medicine methods are not used in the treatment of this pathology. Firstly, if the disease is diagnosed in a child, he is prohibited from giving any decoctions or infusions. Secondly, these remedies do not eliminate the disease and restore cartilage tissue.
Make an appointment Online booking
- Clinic on Krasnopresnenskaya +7 (499) 252-41-35 Volkov lane, 21
- Clinic on Varshavskaya +7 (499) 610-02-09 Varshavskoe highway, 75, building 1
- Clinic in Annino +7 (495) 388-08-08 Varshavskoe highway, 154, building 1
Treatment
Until the age of 20, the bone growth zones have not yet closed, so treatment for uncomplicated cases is carried out conservatively. So, in the 1st stage, therapy includes NSAIDs locally in the form of ointment or cream and orally in the form of tablets, limiting exercise up to bed rest and physiotherapy (electrophoresis, massage, etc.).
In severe cases of the disease and in the age group over 20 years, surgical treatment is used. Arthroscopy allows for complete restoration without affecting nearby tissues.
The operation in the early stages of development involves excision of necrotic tissues and their complete replacement with healthy ones. This is possible through the use of Kirschner wire tunneling or micro-texturing. In this case, the cartilage is perforated to the area providing restoration (regeneration). Finally, the renewed cartilage is further fixed.
When stage 4 develops, the cartilage is completely removed, necrotic areas are excised, the edges of the cartilage are trimmed, and microfracture is performed. In some cases, they resort to autoplasty with the introduction of their own cylindrical sections of healthy, not heavily loaded areas of cartilage.
Complications of osteochondritis dissecans
The most serious consequences of this disease include complete degeneration of the joint and cartilage in the knee area. In this case, there is a lack of motor ability and dystrophic changes in the lower limb.
Violation of the mechanical properties of the joint due to insufficient nutrition of bone tissue can provoke the appearance of deforming gonarthrosis. The most characteristic sign of this pathology is pain, which increases with excessive stress; pathological change in gait. Patients also note a sensation of a foreign body inside the joint and its blocking. In addition, if you have been diagnosed with Koenig's disease, x-rays may show a decrease in joint space and the presence of pathological foci indicating a violation of the structure of bone tissue.
As the disease progresses, you may experience:
- Persistent decrease in range of motion and the appearance of crunching inside the joint;
- Changes in the contours of the knee joint, which is caused by atrophy of muscle tissue and loss of cartilage, as well as destruction of bone tissue;
- Noticeable reduction in joint space;
- The appearance of bone tissue growths near the joint space.
In advanced stages of the pathology, the patient is unable to fully bend and straighten the knee joint, he notes increased pain, gait changes and significant deformation of the limb occurs.
If the above stage of Koenig's disease of the knee joint occurs, loose intra-articular bodies are observed on x-rays, massive osteophytes are formed, a significant reduction in the joint space is noted, aseptic necrosis is diagnosed, as well as sclerosis and deformation of the articular surfaces.
We also perform x-rays and MRIs. In this case, modern high-precision equipment is used, which guarantees high information content and accuracy when making a diagnosis.
What to pay attention to so as not to miss the disease
The problem is that Koenig's disease has no specific symptoms. The signs are quite general and duplicate other pathologies of the musculoskeletal system, but the danger is much higher. Therefore, you should not ignore the following signs that your body gives you:
- knee discomfort;
- aching pain of varying intensity;
- increased discomfort when moving;
- pain without a good reason;
- tissue redness, local swelling;
- a crunch in the knee, which also occurs when cartilage is depleted;
- feeling of stiffness;
- inflammation in the joint;
- gait disturbance;
- visually noticeable changes in gait, lameness.
Prevention of osteochondritis dissecans
There are no special preventive measures to prevent this disease. This is due to the insufficiently studied etiology of the disease.
However, it is still possible to minimize the likelihood of its occurrence. To do this, you should strictly follow the recommendations below:
- Practice healthy eating habits by including enough vegetables, fruits and proteins in your diet.
- Eliminate the use of tobacco products and stop drinking alcohol.
- Minimize stress on the joint.
- Regularly prevent vascular diseases.
- Contact a qualified specialist at the first manifestations of Koenig's disease.
Forecast
If you contact a specialist in a timely manner and have a mild form of the disease, the prognosis for patients is in most cases positive. At the same time, it is possible to achieve rapid restoration of health.
Unfortunately, in advanced stages of the pathological process one cannot count on a complete recovery of the patient.
Timely initiation of treatment measures and compliance with prevention recommendations make it possible to stop the development of the disease and maintain a person’s quality of life. In turn, if pronounced pathological processes are detected, the patient is placed on disability.
Etiology and statistics
Scientists have not come to a general conclusion regarding the etiological cause of the development of osteochondritis dissecans. There are several reasons left:
- past joint injury;
- improper blood circulation in the hip projection;
- endocrine pathologies;
- violation of enchondral ossification (bone formation);
- genetic predisposition.
According to statistics, men aged 17-35 years are more often susceptible to pathology. Damage develops in 80% of cases on the medial (internal) condyle of the femur. Due to the rapid progression of degenerative destruction, a quick visit to a traumatologist and proper therapy will help save the joint.