Any injury to the bones of the skull is extremely dangerous. The jaw is most often affected; young men aged 18 to 40 are at risk. Fractures of the upper and lower jaw require serious and immediate treatment
, so it is very important to contact a specialist in time.
What is a jaw fracture?
A jaw fracture is a facial injury that damages the integrity of its bones. Occurs when the intensity of the traumatic factor exceeds their strength. This injury is common and can be caused by any injury: strong blows to the face, a fall on a hard surface.
Most often, traumatologists observe a fracture of the articular process, although there are also injuries in the area of the angle of the lower jaw, in the middle of the body of the lower jaw bone, in the projection of the mental process. The fracture can be complete or not, open or closed.
Signs of injury are obvious: a person is unable to open his mouth wide, he experiences pain when trying to talk, and his bite changes. Sometimes double vision, numbness in an area of the face, and deformation of the cheekbone may occur. The full list of symptoms will depend on the nature of the injury and its location.
Metal Kirschner spokes
This type of wire was first used to treat fractures of the lower jaw in 1933. Intraosseous insertion of these wires can be carried out both percutaneously (without incisions) and with soft tissue incisions.
In 1975 V.V. Donskoy used an original technique, with which he inserted a wire into the branch of the lower jaw through the mucosa without an incision, then carried out a reposition, and fixed it like a splint to the teeth or to a splint. Later, in 1988, Deryabin E.I. and Osipov V.Yu., and Yu.G. Kononenko and G.P. Ruzin proposed modifications of this method in 1991. Today there are many techniques where the wire suture is combined with knitting needles, staples, surrounding wire ligatures, etc.
Fracture of the lower jaw
If we talk about a fracture of the lower jaw, then we should consider the main types of such injury:
- A complete fracture is considered when there is a displacement of fragments of the jaw. They may vary in shape and quantity.
- A fracture is called incomplete when there is no displacement.
- With an open injury, both the mucous membranes of the mouth and the soft tissues of the face are damaged.
- With a closed injury, the bone does not break through the adjacent tissues, but remains inside them.
- A comminuted fracture of the jaw is rare because it requires incredible force to occur. He requires mandatory surgical intervention.
The following signs are characteristic of a fracture of the lower jaw:
- Swelling and hemorrhage in the damaged area and the resulting asymmetry of the face. The swelling is usually severe, with redness of the skin and an increase in its temperature. When the fracture is closed, blood accumulates in the soft tissue and forms a clot. With an open injury, blood more often enters the oral cavity than into the external environment. The greater the blood loss, the larger the vessel was damaged, and the faster first aid and delivery of the victim to a medical facility is required.
- Sensation of pain when touched. It intensifies when trying to talk, as the periosteum is damaged.
- Displacement of fragments of varying degrees of severity, their mobility.
- Change in bite.
- Increased sensitivity and electrical excitability of teeth.
Depending on where the injury is localized, there are:
- A fracture passing through the center of the incisors is median.
- Trauma between the first and lateral incisors is incisal.
- A fracture localized in the canine area is a canine fracture.
- The injury opposite the chin is mental.
- Injury to the body of the jaw, the one located between the 5th and 8th teeth.
- The fracture beyond the 8th tooth is angular.
- In the upper third of the jaw there is a fracture of the jaw branch.
- Fracture of the base of the condylar process.
- Cervical fracture, that is, the one located near the process of the jaw (condylar) and coronal, located near the coronoid process.
Providing first aid if a person has suffered a fracture of the lower jaw is as follows:
- To begin with, the jaw must be fixed. This is done using a bandage. You need to place a flat, hard object, such as a ruler, under your teeth. The lower jaw is then pressed against the upper jaw and immobilized by wrapping it in a bandage. If the person is not conscious, then this cannot be done, as it will be possible to miss swallowing the tongue or getting vomit into the respiratory tract.
- If there is bleeding, it must be stopped. To do this, the wound is pressed or tamponed with a clean, preferably sterile, material. If you additionally apply cold to the site of injury, this will help reduce blood flow and also somewhat alleviate the pain symptom.
- It is important to keep the oral cavity clear of possible debris, in particular: blood clots and vomit.
- Try not to disturb the person until the medical team arrives. It is better for him to sit; if this is not possible, then you can lay him face down or on his side.
- If severe pain occurs, it is necessary to relieve it. For this, analgin, revalgin, and naproxen are used. Since a person with such an injury will not always be able to swallow a tablet, it is necessary to crush it into powder and dissolve it in water and give it to the victim to drink. An intramuscular injection will be even more effective, but, as a rule, it is rarely possible to do it during first aid. Cold, which will constrict blood vessels, reduce swelling and pain, will also help alleviate the condition. But before applying ice, it must be wrapped in a cloth.
After carrying out these activities, the person must be taken to a medical facility for further treatment by professionals. X-ray examination is used to diagnose a fracture. Since this is a serious injury, often accompanied by a spinal injury, an additional x-ray of the cervical spine is often prescribed before starting treatment. This is done to prevent damage to the spinal cord. It is also necessary to make sure that the person does not have a concussion or intracavity cranial bleeding.
International standards
A real revolution in maxillofacial surgery occurred in 1958, when M. Muller, M. Allgower, R. Schneider, H. Willenegger organized the International Association for the Study of Internal Fixation (AO/ASIF - Ardeitsgemeinschaft fur Osteosynthesefragen/Association for the Study of Internal Fixation – working association for the study of osteosynthesis/association for the study of internal fixation).
According to the postulates of AO/ASIF, the osteosynthesis technique implies that:
1. the structures used must be made of bioinert metal alloys;
2. bone fragments must be anatomically accurately compared and fixed;
3. the use of gentle surgical techniques ensures the preservation of blood supply to bone fragments and surrounding soft tissues;
4. stable fixation of fragments is ensured by interfragmentary compression;
5. early application of functional load is indicated;
6. restoration of contractile activity of muscles and movement in the joint.
AO/ASIF staff also developed and implemented metal plate systems for mandibular osteosynthesis:
· dynamic compression plates;
· reconstructive (blocking) plates (Locking reconstruction plates);
· blocking (locking) plates (Locking plates 2.0 mm);
· universal plates (Universal fracture plates);
· mandibular plates (Mandible (Mandible plates 2.0 mm).
They developed dynamic compression plates (DCP), through which it was possible to create compression between fragments for their primary fusion. The design of these plates includes oval holes with beveled walls, which allows the fragments to be brought closer together when the screws are tightened. The use of dynamic compression plates made it possible to achieve stable internal immobilization, reduced the number of cases of delayed fusion of fragments, and eliminated the need for additional fixation. But their use still does not eliminate the risk of microcracks in the area of the fracture line and the development of osteoporosis in the bone at the site of contact with the plate.
The locking plate/screw system, with threaded plate holes and locking screw heads, was developed to prevent bone necrosis under the plate. The system provides rigid fixation of bone fragments using a plate and a plate and screws to each other - this helps prevent the screws from unscrewing and avoid possible displacement of the fragments while tightening the screws in the hole of the plate. The plate itself is located at a certain distance from the surface of the bone, which prevents the development of lysis.
Foreign studies have not revealed significant differences in the effectiveness and possible development of postoperative complications during osteosynthesis with locking plates with screws and non-locking plates.
Another system developed by AO/ASIF experts is the LCP (locking compression plate system with angular stability) is a design of multi-cell plates with numerous holes and consists of two parts: a threaded one for fixing the head of a locking screw and a hole for creating dynamic compression by eccentric insertion of standard cortical or cancellous screws.
Installation of the plate requires special tools and is carried out according to clearly established technology.
If the adjustment of the LCP to the shape and relief of the outer surface of the lower jaw bone is carried out in accordance with the established requirements, then this creates ideal conditions for the fusion of fragments during osteosynthesis of multiple comminuted fractures of the lower jaw of various locations, in case of suppuration of a bone wound, traumatic osteomyelitis, in case of a fracture with the occurrence of a bone defect tissue, fracture of toothless jaws. Limited contact of LCP with bone helps prevent the development of bone necrosis under the plate.
Maxillary fracture
A fracture of the upper part is somewhat less common and accounts for up to 30% of all cases of jaw damage.
It is classified depending on the fracture line:
- The inferior line (lefor one) has a direction from the beginning of the pyriform aperuta to the process of the sphenoid bone (pterygoid).
- The middle line (lefor two) runs along the bones of the nose, including the bottom of the orbit and the pterygoid process.
- The upper line (lefor three), directed to the cheekbone, through the bones of the nose.
The danger of injury lies in its consequences, which can be expressed in meningitis, concussion and osteomelitis. The higher the break line is located, the more often undesirable consequences occur.
Signs of a fracture of the upper jaw, depending on its type:
- If there is a fracture under the palatal vault, with a fracture of the maxillary sinus and a fracture of the nose, the victim experiences swelling of the cheeks, nose and lips, with severe bleeding between the lip and teeth.
- If part of the upper jaw is torn off from the base of the skull, and the fracture line crosses the orbit and bridge of the nose, then there is numbness in the area under the eyes, and pronounced hematomas in the same place. Blood flows from the nose, and it is often impossible to stop the drooling. The sense of smell is either completely absent or significantly impaired.
- If the jaw separation is accompanied by a fracture of the base of the skull, then vision function will be impaired and the mouth will not be able to open. The face will be asymmetrical, the hematomas resemble glasses, the eyeballs will be lowered down.
Regardless of the type of fracture, a person often experiences nausea, vomiting may occur, the bite will be disturbed, and the pain will be pronounced. All other functions are difficult, such as breathing, chewing and speech. A concussion almost always accompanies this injury.
First aid, in addition to basic measures in the form of immobilization, pain relief and bleeding control, should be supplemented by restoring respiratory function. To do this, it is necessary to remove all foreign objects from the mouth, in particular, tooth fragments and vomit. If a person is feeling nauseous, they should immediately lay them on their side or face down.
Displaced jaw fracture
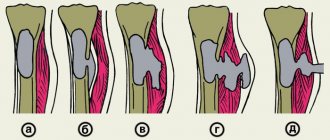
In case of a jaw fracture, displacement of fragments can be observed in three directions: sagittal, vertical and transversal. They play a decisive role in determining treatment tactics and choosing the device that will be used to reduce them.
Most often, splints made of wire are used, secured by the teeth. The bones are collected manually by the surgeon; at this time the patient can be under either local or general anesthesia. Fixation of fragments can also be carried out using a nylon core. Next, the jaw is secured with metal knitting needles or plates, which are applied externally.
When fixation is carried out, the patient is recommended to rest and take antimicrobial measures.
Consequences of a jaw fracture
In order to avoid the consequences of a jaw fracture, you should not self-medicate, but seek medical help as soon as possible. Complications include:
- Displacement of one row of teeth.
- The formation of pronounced gaps between the teeth, which will be located at the site of the fracture.
- Severe displacement of fragments with facial deformation due to muscle strength.
- Displacement of teeth resulting in an abnormal bite.
- Meningitis.
- Osteomelit.
Treatment of a jaw fracture
Treatment of a jaw fracture is the prerogative of the doctor. The sooner it is started, the better for the patient.
Basically, the activities come down to the following actions:
- Treating the existing wound and disinfecting it.
- If there is a displacement of the nasal septum, then its alignment.
- Comparison of possible fragments and alignment of whole bones.
- Reliable fixation of the jaw using a special splint. She must be completely immobilized. A splint is applied for up to 1.5 months, until the jaw bones heal. Sometimes doctors surgically implant metal plates into the jaw. They are fixed with screws.
- Carrying out anti-inflammatory therapy.
When the main course is completed and the splint is removed, then it will be possible to move on to the rehabilitation stage. It should be aimed at restoring several vital functions: chewing, swallowing, speech, vision.
Splinting for a jaw fracture
Splinting is one of the main methods of treating jaw injuries. The procedure involves fixing fragments using a structure consisting of plastic or wire.
The type of splinting depends on the nature of the injury:
- It is applied on one side when the fracture is one-sided; a wire is used to fix the damaged areas.
- It is applied on both sides, while the structure has a more rigid base. In addition to it there are hooks and rings.
- When both the upper and lower jaws are broken and there is displacement, then it is advisable to use double-jaw splinting. For fixation, copper wire is used, fastened to the teeth and fixing the jaws with rings.
If a plastic version is used, it should be placed under the chin and secured with a bandage around the head. But this method is indicated in cases where assistance must be provided in a short time in order to deliver the victim to the traumatology department.
When the fracture is complicated and there is significant displacement of the fragments, then before splinting, it is necessary to compare them.
On topic: 12 folk methods for home treatment
Recommendations
Treatment of mandibular fractures involves long-term immobilization of the jaws, which becomes a significant psychological problem for the patient. The success of treatment directly depends on how closely both the doctor and the patient act together and take the process seriously.
For the entire period of healing of the fracture, the patient is prescribed a diet (maxillary table No. 1 and No. 2); food is allowed to be taken only in a creamy consistency (well boiled and passed through a blender). In most cases, opening the mouth is impossible, because... The patient has an intermaxillary rubber traction device installed. Food is supplied through tubes, tubes and sippy cups.
From the moment of double-jaw splinting or osteosynthesis, the splints are left in place for an average of 21–30 days. If the doctor has confidence in the favorable course of the recovery process, then it is possible to reduce the period of wearing the intermaxillary rubber traction.
Even after removing the splints, the patient cannot fully open his mouth for 1-2 weeks. To restore the function of the chewing and facial muscles, he is prescribed myogymnastics.