Author
: Grachev Ilya Illarionovich
Editor
: Efremov Mikhail Mikhailovich
Date of publication: 06.10.2014 Date of update: 12.11.2020
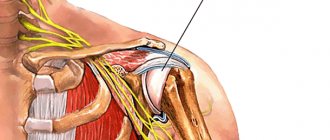
A disease characterized by inflammation of the periarticular bursa in the shoulder area is called bursitis of the shoulder joint. This disease refers to diseases of the musculoskeletal system. It can most often occur in professional athletes and people whose work involves lifting weights.
The disease causes severe pain when rotating a limb or moving the arm to the side, so bursitis is difficult to miss. After the first symptoms appear, it is important to begin timely and high-quality treatment in order to prevent the disease from entering the chronic stage. By contacting our clinic, we can quickly solve the problem that has arisen.
Any form of bursitis has serious complications, so you should not delay treatment.
See how easily the disease can be cured in 10-12 sessions.
Causes of shoulder bursitis
The main causes of shoulder bursitis are all kinds of trauma or tissue damage. In general, causes can be divided into infectious and aseptic. Common causes of the disease include the following:
- Physical overload
- Autoimmune or allergic diseases
- Prolonged stress on a joint can also cause bursitis.
- Chronic intoxication of the body due to alcoholism or smoking
- Shoulder arthritis of any origin
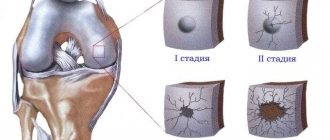
Classification of bursitis disease
As a disease, bursitis is usually divided into:
- specifics of the course
(acute, subacute, chronic or recurrent); - pathogen
(specific or nonspecific infections, inflammation without an infectious pathogen), as well as origin (primary or secondary bursitis); - type of exudate
(serous, purulent, hemorrhagic) - localization
.
Bursitis with a sudden onset and acute course can be completely cured if therapy is started early. If a visit to the doctor is constantly postponed or his recommendations are not followed, the transition to a chronic form is most likely
- in this case, the disease lasts several months, and subsequently recurs, causing irreparable consequences.
As a primary disease, bursitis occurs with direct damage to the joint capsule or local infection. Secondary - as a consequence of another chronic disease. The type of exudate can be determined only after taking a sample - based on it, treatment will be selected.
Symptoms of shoulder bursitis
Limited movement in the joint and severe pain are the main symptoms of shoulder bursitis. It becomes difficult for a person to perform usual actions with an injured hand, and his ability to work is limited. Other obvious signs, if you notice them, you should immediately seek qualified medical help:
- Pain when feeling the joint, accompanied by redness of the skin, as well as noticeable swelling in the shoulder area
- As a consequence of the body's protective reaction, bursitis causes an increase in muscle tone
- Inability to perform normal activities with the injured arm
- General weakness, local fever
Intra-articular injections of hyaluronic acid
Chondroprotectors: what are they, how to choose, how effective are they?
How to prevent bursitis?
In order to prevent the occurrence of bursitis, it is recommended to follow the advice of experienced specialists:
Reducing physical activity, which is aimed at the area of the shoulder girdle and collarbone;
Rejection of bad habits. In this case, you need to stop drinking alcoholic beverages and stop smoking tobacco products. They contain carcinogenic substances that quickly penetrate the bloodstream and contribute to abnormal changes in the body;
Proper nutrition. The diet should contain natural products, animal and plant proteins, as well as a high level of fiber. These components help normalize metabolic reactions and promote the elimination of toxic substances;
Timely diagnosis and properly selected treatment make it possible to prevent serious pathologies in the body in time;
Active lifestyle. Regular movement helps prevent salt deposits in the joints and bone mass. It has been scientifically proven that professional athletes are less likely to suffer from this pathology.
Treatment methods for shoulder bursitis
High-quality treatment of shoulder bursitis at the Paramita clinic is based on the use of the most effective methods of oriental therapy. For each patient, after a thorough examination, the clinic’s doctors develop an individual set of procedures, among which the following methods are the most effective:
- Acupuncture – improves overall well-being, relieves swelling and inflammation
- Moxibustion therapy treats bursitis by improving tissue nutrition and accelerating joint recovery
- Therapeutic gymnastics improves blood circulation, relieves pain in the joint
- Jiu therapy relieves inflammation, stimulates blood circulation and tissue nutrition
- Pharmacopuncture stimulates accelerated tissue healing, relieves inflammation, strengthens the immune system
- Vacuum therapy is aimed at draining lymph from the source of inflammation and thus removing tissue swelling.
- PRP therapy is the latest method of stimulating recovery processes. It is used to restore joint function after diseases and injuries, including to restore the function of the musculoskeletal system in case of bursitis.
We combine proven techniques of the East and innovative methods of Western medicine
Read more about our unique method of treating bursitis
Treatment of shoulder bursitis at the Paramita clinic
When the first symptoms of the disease appear, we recommend that you contact the clinic. Our doctors have many years of experience and high qualifications, which allows us to guarantee treatment of shoulder bursitis quickly, without the use of drugs or surgery.
We practice an individual approach to each patient, and in addition to eliminating pain symptoms, as well as the root cause of the disease, our specialists will restore immunity and increase the patient’s energy, improve overall well-being, and restore lost ability to work. You will forever forget about such a disease as bursitis. By contacting our clinic, the disease will be cured, and pain will be a thing of the past.
Sign up for a free initial appointment
Treatment
Treatment of joint bursitis is aimed at quickly relieving pain and further eliminating the disease. Therapy lasts 14 days or 1.5 months. Surgical intervention is necessary in advanced cases.
Treatment for bursitis includes:
- taking medications;
- physiotherapy;
- aspiration;
It is important to provide rest to the diseased part of the body and avoid further traumatization. If you endure pain, move or work through discomfort, then bursitis will develop into a chronic stage.
The doctor prescribes compresses and ointments to treat bursitis. Cold compresses can be applied to the sore spot for no more than 15 minutes; if kept longer, there is a risk of frostbite.
Non-steroidal medications are prescribed. These include: Ibuprofen, Dexalgin. Antibiotics if infection is present.
If liquid has accumulated, it is removed. This is done after the inflammation in the bursa has decreased, but the fluid remains. Using a syringe, the specialist pumps out 5 to 20 milliliters of liquid, then injects cortisone. Apply a pressure bandage to prevent fluid from accumulating. It is important to carry out such manipulations only in sterile conditions, minimizing the risk of infection and infection.
Injections into the sore joint help a lot. Injections for bursitis are prescribed with Diprospan. Glucocortisone, Prednisolone, Methylprednisolone, Dexamethasone, Triamcinolone are also prescribed.
Physiotherapeutic methods are used such as: ultrasound or diathermy. Physiotherapy helps relieve inflammation, relieve pain, and increase the effect of medications. At the same time, physiotherapy often has no contraindications. Perfectly complements the complex treatment of bursitis.
Other physiotherapy methods:
- balneotherapy;
- magnet therapy;
- electrophoresis;
- shock wave therapy;
A massage may be prescribed, but only during the period when the illness subsides.
Surgery is needed when there is a very large lump, and the treatment will be long and lengthy. Then the specialist can perform a puncture or drainage of fluid in the bursa.
Surgery for bursitis is performed in case of accumulation of purulent contents in the bursa. Sometimes a specialist performs tissue excision or bursectomy. This is done when the previous treatment did not have the desired effect.
Diagnosis of shoulder bursitis
Diagnosis of bursitis in our clinic is carried out on the basis of effective techniques of oriental medicine, which allow not only to make an accurate diagnosis, but also to identify the causes and neutralize the consequences of the disease.
Diagnostics using oriental techniques is carried out in several stages, during which our specialist:
- conduct a conversation, ask a series of questions to understand the nature of the possible source of the disease;
- perform pulse diagnostics on both arms and, based on these data, draw a conclusion about the state of the body;
- will perform an initial examination of the shoulder;
- will carry out a test load to determine the severity of the disease;
- determine the type of bursitis and the degree of its development by palpation of the shoulder.
If necessary, additional studies will be ordered using special equipment and modern scientific advances.
Disease prevention
You can prevent the risk of bursitis using preventive measures:
- reduce physical activity;
- use a bandage or simply bandage the shoulder area tightly;
- treat wounds in a timely manner;
- observe safety measures;
- avoid hypothermia.
Preventive measures should be carried out taking into account the general condition of the patient, therefore the doctors of our clinic recommend them to each patient individually.
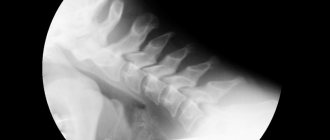
Diagnosis of pathology
An experienced doctor is able to quickly diagnose this pathology. Diagnostics includes the following steps:
Inspect the affected area for redness and swelling;
Questioning the patient. This manipulation allows you to accurately determine the cause of the disease and the duration of its course;
Radiography. This will allow us to identify the location of the inflamed lesion and its size;
Puncture of fluid from the joint capsule. Such a study makes it possible to study its composition and the presence of purulent contents;
Ultrasound diagnostics. It is carried out to determine the exact location of the inflamed area;
Magnetic resonance imaging of the shoulder.
Diet for shoulder bursitis
A preventative diet is of decisive importance for both the treatment of shoulder bursitis and the rehabilitation period.
Its key points:
- If possible, minimize the consumption of salty and sour foods;
- consume plant products daily, and meat products no more than 3 times a week;
- Be sure to include dairy products in your diet;
- reduce proteins and fats in the diet to a minimum;
- steam, boil, bake foods;
- coffee, chocolate, alcohol are absolutely prohibited;
- Eat foods that are difficult for the stomach (mushrooms, smoked meats) as rarely as possible.
Exercises for shoulder bursitis
After the pain disappears, you can develop the joint using the following exercises:
- Sit at the table with your hands on its surface. Make oscillating movements with your elbows to the outside and inside.
- In a standing position, lower your arms along your body. Make rotational movements with your shoulders.
- The starting position is the same as in the previous exercise. Move your shoulders up and down.
- The starting position is the same. Move your shoulders back and forth.
- Extend your arms in front of you. Lift up. Spread to the sides. Return to original position. Repeat 7-10 times.
Attention! You can choose any of the above exercises for yourself only with the consent of your doctor! Each body is unique: what is good for one patient may seriously harm another.
Clinic and diagnostics
Depending on the causative factor, bursitis can be serous (aseptic) or septic. Serous inflammation develops when:
- skeletal abnormalities (scoliosis, joint hypermobility, bone deformities, etc.);
- age-related changes;
- injuries;
- excessive stress on the joint;
- spondyloarthritis;
- rheumatoid arthritis;
- gout;
- metabolic disorders;
- systemic diseases and other pathologies.
Septic bursitis develops due to wound infection against the background of reduced immunity. Contribute to the development of the disease:
- purulent focus (boil, carbuncle, etc.);
- HIV;
- therapy with corticosteroid drugs;
- diabetes;
- alcoholism;
- hypothermia, etc.
Based on the nature of the pathological fluid accumulating in the joint, purulent, hemorrhagic, fibrinous and serous bursitis are distinguished.
The prevalence and localization of the disease is determined by the professional activities of people. Heavy physical labor, sports, and other dynamic and static loads provoke the development of bursitis. In this case, inflammation of the elbow joint is more common among engravers, polishers, and embossers; shoulder - for loaders, blacksmiths; knee – among miners, tilers, priests; heels - for nurses, surgeons, dancers, salespeople.
Bursitis also occurs as a complication when remaining immobile for a long time for therapeutic purposes. An example is the situation with patients with coronavirus infection being in a prone position (ventilation of the lungs is facilitated in a prone position).
General signs of the disease:
- joint pain that increases with movement, pressure and at night;
- edema;
- restriction of movements;
- redness, thinning, increased temperature of the skin over the joint.
Symptoms of individual types of bursitis have their own characteristics.
When the elbow joint is affected, the pain is moderate, a mobile red swelling appears, and movement is difficult.
Pain with shoulder bursitis manifests itself with flexion, abduction to the side, as well as in the lying position on the affected side, with irradiation along the arm. The patient finds it difficult to carry out daily activities.
The structure of the hip joint contains several synovial bursae. Inflammation of the greater trochanteric bursa is accompanied by pain along the lateral femoral surface, which intensifies when lying on this side, when moving and flexing the hip, when standing up, when climbing stairs, at night. The disease is more common in dancers and athletes.
With iliopectineal bursitis, swelling and pain are localized on the inner femoral surface in the groin area, and a tingling sensation appears. Pain increases with hip extension.
Sciatic bursitis is found mainly in people of thin build who lead a sedentary lifestyle, often against the background of spondyloarthritis. The pain intensifies when sitting on a hard surface or when bending the hip.
“Parquet floorer's knee” or prepatellar bursitis is usually diagnosed in people who have to kneel for long periods of time. Swelling, mild tenderness, redness, and a warm sensation in the knee joint are typical.
Anserine bursitis, or pes anserine bursitis, often accompanies arthrosis of the knee joint (gonarthrosis). The disease is common among women during menopause who are overweight. The pathology manifests itself as pain at night, swelling, and accumulation of fluid in the joint.
Rice. 2. External manifestations of bursitis
In the absence of adequate therapy, complications are possible. These are chronicization of the aseptic process, necrosis of the bursa, secondary septic arthritis, osteomyelitis, sepsis and other pathologies.
The diagnosis is established by:
- changes in blood test results;
- determining the level of pain using a visual analogue scale (VAS);
- assessment of mobility limitation upon examination, through goniometry;
- data from instrumental studies (radiography, ultrasound).
If necessary, a diagnostic puncture of the joint is performed to study the synovial fluid.