Consultation with a proctologist – 1,750 rubles.
- What is paraproctitis (rectal fistula)?
- Symptoms of paraproctitis
- Types and stages of the disease
- Diagnosis of rectal fistulas
- Treatment of paraproctitis
- Surgery
- Main risks
- Prevention
- Popular questions
Chronic paraproctitis (rectal fistula)
– a chronic inflammatory process in the anal crypt, intersphincteric space and pararectal tissue with the formation of a fistulous tract. The affected crypt is the internal opening of the fistula.
According to statistics, most patients with rectal fistulas associate the occurrence of the disease with acute paraproctitis. About a third of patients with acute paraproctitis consult a doctor after spontaneous opening of an abscess, after which in most cases a rectal fistula is formed. Approximately half of the patients with acute paraproctitis undergo radical surgery at the time of treatment, the other half only undergo opening and drainage of the abscess without eliminating the entrance gate of the infection, which can subsequently lead to the formation of a rectal fistula. In this case, constant infection occurs from the intestinal lumen, and a fistula tract is formed from scar tissue. The external opening of the fistula is most often localized on the skin of the perineum, its diameter is often no more than 1 mm. If the fistula tract is insufficiently emptied, purulent cavities may form along its length.
The prevalence of chronic paraproctitis reaches 23 cases per 100,000 population, the proportion among rectal diseases reaches 25-30%. Males are more susceptible to this disease than women; the disease more often manifests itself in young and middle age Source: Khomochkin V.V. Operation of ligation of the fistula tract in the intersphincteric layer in the treatment of chronic paraproctitis / V.V. Khomochkin [et al.] // News of surgery. - 2021. - T. 26. - No. 5. - P. 616-623. .
Symptoms of paraproctitis
Symptoms directly depend on where the fistula is located and the state of the patient’s immunity.
Usually, after an illness, a person experiences pain in the anus and a hole appears from which pus comes out. This causes itching, irritation, and bad odor. Sometimes ichor is released along with pus. This occurs when blood vessels are damaged. If the fistula has no outlet, then patients complain only of pain and/or discharge from the rectum or vagina.
An incomplete internal fistula provokes a sensation of the presence of a foreign body in the anal area. If the infiltrate does not leave the fistula cavity enough, the following symptoms appear:
- discomfort and pain in the anal area;
- retention of urination and defecation;
- discharge of mucus, infiltrate, pus from the rectum;
- increased body temperature, chills;
- redness and irritation of the skin around the anus and part of the buttocks.
Chronic paraproctitis during the period of exacerbation gives the following symptoms:
- fast fatiguability;
- sleep disturbance;
- nervous exhaustion;
- headache;
- regular increase in body temperature;
- intimate disorders;
- gas incontinence.
Physiological changes may occur:
- anal deformation;
- disruption of the anal sphincter;
- scars on the muscle tissue of the anal sphincter.
During periods of remission of chronic paraproctitis, the general condition is normal; with proper hygiene, the quality of life is almost not reduced. But with a long course of the pathology and frequent exacerbations, the following may occur:
- sleep disorders;
- powerlessness, weakness;
- headache;
- periodic changes in body temperature;
- nervousness;
- poor work ability;
- deterioration of potency.
A rectal fistula is a small “tunnel” in the tissue between the outer area of the anus and the anal canal - that is, the lowest part of the rectum. If there is itching, pain and wetness (weeping areas) in the anus for a long time, these may be signs of an anal fistula.
In most cases, an anal fistula occurs due to an abscess of the anus, that is, the formation of a capsulated purulent bubble in the anus. Through a fistula (fistula) - a pipe-like passage in the tissue - pus flows out.
Depending on the appearance of the anal fistula, doctors distinguish two forms:
- Complete rectal fistula: The fistula runs continuously from the intestinal mucosa in the anal canal to the outer skin and has two ends (openings).
- Incomplete rectal fistula: the fistula has an opening on only one side, either on the skin side (external opening) or on the mucous membrane side (internal opening). The opposite side ends in a “dead end”.
Most often, anal fistulas occur in young adults between the ages of 30 and 50. This disease occurs more often in men than in women. Typically, treatment for an anal fistula requires surgery, during which it is completely removed if possible. After this, in most cases, healing proceeds without complications.
Forms of rectal fistula according to Parkes' classification
In accordance with the classification created by an English proctologist (a specialist in the field of diseases of the rectum), depending on the course of anal fistulas, as well as their connection with the sphincter, doctors distinguish several forms of anal fistulas:
- Intrasphincteric (intersphincteric) anal fistulas (45 percent): the course of the fistula lies on the surface, passes through the internal sphincter and runs further into the tissue between the internal and external sphincter.
- Transsphincteric (transsphincteric) anal fistulas (40 percent): the course of the fistula runs through both internal and external muscles.
- Suprasphincteric anal fistulas (five percent): An anal fistula lies above the sphincter and breaks through the pelvic floor muscles.
- Extrasphincteric anal fistula (one percent): This is the rarest form of anal fistula. In this case, the fistula passes through the Musculus levator ani (the muscle that lifts the ani) to the pelvic floor and ends in the rectum above the anus. This form is typical of chronic inflammatory bowel diseases such as Crohn's disease or ulcerative colitis.
- Rectovaginal fistula (five percent): In this type of anal fistula, there is a connection between the rectum and the female vagina.
Typical symptoms of rectal fistula
In the presence of an anal fistula, patients complain of various symptoms in the anal area, mainly pain during defecation, and also after that.
In addition, the following symptoms are typical for anal fistula:
- Dampness (wet areas) in the anus.
- Itching in the anus.
- Stool incontinence.
- General painful condition.
- Increased body temperature.
Purulent secretion flows out through the anal fistula, sometimes mixed with stool. Signs of this process are moisture (wet areas) in the area of the fistula outlet. Corresponding traces are found on the clothes and in the feces of patients; Additionally, an unpleasant odor also occurs. Sometimes patients with an anal fistula also experience general symptoms, such as fever or general weakness - however, these symptoms do not always occur.
What causes the formation of rectal fistulas?
In the case of anal fistula, the causes are mainly inflammatory processes that occur in the anal glands (proctodeal glands). Unlike many animals, in humans the anal glands are only a non-functional residual organ due to evolution (vestigial), like wisdom teeth or the vermiform appendix of the cecum. Anal glands are more common in men than in women. They are located on the side of the anus between the internal and external sphincter.
Causes of rectal fistulas
In the case of rectal fistulas, the causes often arise here: The anal glands can cause painful inflammation, during which pus accumulates and cannot be released. This forms a purulent ulcer (abscess). If the pressure inside the pus becomes too great, a fistula breaks out in the surrounding tissue, through which pus then leaks out. Even after surgical dissection of the anal abscess, an anal fistula occurs in two thirds of all cases.
In addition, in the case of anal fistulas, various pathological diseases can be considered as causes - for example, diabetes mellitus and chronic inflammatory bowel diseases such as Crohn's disease or ulcerative colitis. Inverse acne (Akne inversa) can also lead to fistulas in the anal area.
This is how the diagnosis of rectal fistula proceeds
In order to properly diagnose an anal fistula, the doctor first asks the patient several questions regarding the exact symptoms. Based on these data, he carefully examines the anal area. Thus, the doctor can already determine, based on an external examination, whether we are talking about a rectal fistula. Additionally, if necessary, he also performs gentle palpation of the anal canal with a finger (digital rectal examination).
Diagnostic methods for suspected rectal fistula
If the course of an anal fistula is unclear or if it is suspected that the fistula passes through muscle tissue, a more thorough examination of the rectum may also be necessary. As part of the so-called rectoscopy, an endoscope (a rod-shaped or hose-shaped mirror device) is inserted into the anal canal, with which the doctor can examine the anal fistula in detail. This study is painless for the patient.
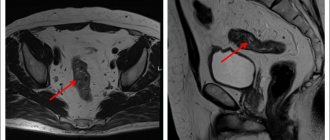
In most cases, these research methods are already sufficient to accurately diagnose an anal fistula. For further treatment planning, the doctor checks the structure and exact course of the anal fistula. To do this, he carefully inserts a probe into the external opening of the fistula (fistula probing). Thanks to this, the doctor can recognize the exact course of the fistula, as well as identify possible branches. If the course of the fistula is very branched or seems very complex, then various imaging diagnostic methods can help in this case - for example, ultrasound examination (sonography) through the anus or magnetic resonance imaging (MRI).
Additional testing may be needed to rule out Crohn's disease or acne inversis as possible causes of anal fistula.
Treatment of anal fistulas: Surgery (surgical treatment) is often considered as a treatment option.
The only effective treatment for anal fistula is surgery, that is, surgical treatment. An anal fistula cannot be cured with medications or ointments. The surgical method used depends on the shape of the fistula.
Surgical treatment of anal fistula using fistula dissection
Superficial anal fistulas (intrasphincteric (intersphincteric) anal fistulas) are dissected by the surgeon, which means that he cuts the tube along its entire length with a scalpel. The entire course of the fistula is removed, and its healing can now proceed from the inside out. It is important, after surgical treatment of an anal fistula, to thoroughly wash the open wound several times a day and bandage it. After each act of defecation, it is recommended to wash the wound with warm water (shower) or take a sitz bath with chamomile. With hard stools, there is a risk of the wound reopening due to straining too much. Therefore, it is advisable to eat mostly fiber-rich foods and drink a lot to keep your stool soft. In some cases, you can also take a mild laxative.
Surgical treatment of anal fistula using plastic closure method
In the case of anal fistulas that pass through the muscle tissue (transsphincteric anal fistulas, suprasphincteric anal fistulas, extrasphincteric anal fistulas), in most cases it is impossible to treat by dissecting the fistula. The muscles, especially the internal and external sphincters, may be damaged only to a minimal extent, otherwise bowel incontinence can easily develop. Instead of cutting the fistula, the surgeon uses a scalpel to carefully remove the entire tubular structure of the fistula from the surrounding tissue. At the same time, he pays attention to touching (damaging) the muscle tissue as little as possible. Finally, the hole in the anal canal is sutured, and the healing process of the fistula proceeds from the inside.
Surgical treatment of anal fistula using ligature drainage method
Often, so-called ligature drainage is suitable for the treatment of an anal fistula. In this case, the doctor pulls a thread (ligature) through the fistula tract and ties a knot from the outside. In this way, secretions and pus can flow out, since the thread prevents premature closure of the external opening of the fistula. In most cases, with the help of ligature drainage, the doctor prepares the ground for further surgery; however, in some cases the suture is left in the fistula tract as a long-term solution (fibrosing suture).
Course of rectal fistula: How to prevent complications
In the case of an anal fistula, the postoperative period, as a rule, proceeds without complications. 95 percent of all fistulas heal over a long period of time, but the healing process can last several weeks, and even months for common fistulas.
In this case, each patient with a rectal fistula can partially take the healing process into their own hands: The decisive factor is the consistent implementation of measures regarding hygiene and wound care.
Complications of rectal fistula: continuity disorders
A relatively common complication of surgical treatment of an anal fistula is incontinence disorders, which means that the patient may have problems holding stool. The more the sphincter is damaged during surgery, the higher the risk of developing stool incontinence. However, thanks to modern methods of surgical treatment, this complication has become less common.
Typically, after treatment of an anal fistula there is no further lasting or permanent damage. The risk of repeated fistula formation (relapse) is very low. The situation is different in patients whose anal fistula is caused by a chronic inflammatory bowel disease, such as Crohn's disease or ulcerative colitis. Since in this case the operation does not eliminate the cause of the disease, new anal fistulas may occur.
How can I prevent rectal fistula?
There are no effective methods to prevent the formation of anal fistulas. A fistula occurs either due to an abscess in the anal area or due to chronic inflammatory bowel disease. These causative diseases are caused by many factors that cannot be directly prevented. However, basic recommendations include a high-fiber diet and good anal hygiene to prevent injuries such as anal fissures and inflammation.
Contact us
In order to make an appointment, get a second opinion from a specialist in the gastroenterology department, undergo diagnostics and treatment at the University Hospital Solingen, contact us by email or phone number. We organize consultations and treatment at the Department of Gastroenterology and the Gastrointestinal Center, including an appointment with Professor Boris Pfaffenbach. You will be accompanied by a translator from German into your native language.
Email: [email protected] Tel.: +49 212 5476913 Viber | WhatsApp: +49 173-2034066 | +49 177-5404270 For your convenience, please save the phone number in your phone book and call or write to us for free on WhatsApp, Viber or Telegram. Applications made on weekends or holidays will be processed on the first business day. In urgent cases, request processing is carried out on weekends and holidays.
Source - https://www.lifeline.de/krankheiten/analfistel-id41133.html
Types and stages of the disease
Rectal fistulas can be complete, incomplete, or internal.
- Complete ones
have two openings - located inside and opening into the rectum, as well as external, usually located next to the anus. - An incomplete fistula
has only an internal opening that opens into the rectum. There is an opinion that this is a transitional phase, because sooner or later the external opening will open and the fistula will become complete. - An internal fistula
has two internal openings that extend into the lumen of the rectum.
According to their location relative to the anal sphincter, fistulas are divided into:
- Intrasphincteric
, or marginal. The most common ones usually have a straight course without scars and an external opening near the anus. - Transsphincteric
- the course of such a fistula goes through the anal sphincter at different depths. The higher the course, the more it branches and the more often purulent streaks form, and scar tissue forms around the fistula itself. Scars can deform the anal sphincter and interfere with its function. - Extrasphincteric
- differ in the location of the internal opening - on the surface of the intestinal crypt. The stroke itself passes high and goes around without affecting the outer pulp. The incidence of such fistulas is 15-20% of the total incidence.
Extrasphincteric fistulas are usually tortuous and have a long course. With them, purulent leaks form and scars form around the fistula canals. With repeated exacerbations, new external openings appear. There is a classification that distinguishes four degrees of complexity of fistulas of this type:
- – there are no scars around the internal opening, the course is straight, infiltrates and purulent streaks do not form in the perirectal tissue.
- – scars appear around the internal opening, there are still no ulcers or infiltrates.
- – the entrance to the fistula canal is narrowed, there are no scars, there are ulcers and inflammatory infiltrates in the perirectal tissue.
- – the inlet is enlarged, surrounded by multiple scars, and there are ulcers and infiltrates in the tissue.
Types of extrasphincteral fistulas
There are several types of extrasphincteral fistulas according to the degree of complexity:
| Degree of difficulty | Characteristic |
| Fistulas 1st degree | There is a narrow opening inside and a straight course of the rectum. There are no purulent accumulations, scars or cracks in the tissue. There are no infiltrates. |
| Fistulas 2nd degree | The inside of the anus is surrounded by cracks and scars. There are no inflammatory or infectious processes. In general, the patient's condition is satisfactory. |
| Fistulas 3rd degree | There are no scars in the narrow internal opening. A purulent-inflammatory process is observed in the fiber. The patient suffers from itching and burning in the anus. |
| Fistulas 4 degrees | The internal opening of the purulent fistula is surrounded by scars. A large number of inflammatory and infectious infiltrates and purulent streaks appear in the tissue. |
Each stage of the disease is dangerous in its own way, so it is worth starting treatment immediately.
Methods for diagnosing rectal fistulas
In the vast majority of cases, the diagnosis is not difficult to make. The proctologist is based on the patient’s complaints, examination and palpation data. Usually, during a digital examination, the doctor discovers holes in the anal area, from which pus comes out when pressed.
When diagnosing and subsequent treatment of rectal fistulas, the determination of the fistula tract is of fundamental importance. For this purpose, digital and mirror examination of the rectum, probing and examination of the fistulous tract with a dye solution, anoscopy or sigmoidoscopy, fistulography, ultrasound, CT, MRI are used Source: Seidova K.R. Etiopathogenesis and diagnosis of pararectal fistulas. Literature review / K.R. Seidova // Bulletin of surgery of Kazakhstan. - 2011. - No. 4. - P. 23-27. .
One of the main methods for studying pararectal fistulas is probing. With the help of probing, along with the internal opening of the fistula, it is possible to determine the depth of the fistula tract, its connection with the intestinal lumen, the relationship of the fistula to the anal sphincter, and by the movement of the tip of the probe in the canal, bay-shaped expansions and additional branches.
Examination of the rectum using a speculum and proctoscopy allows one to distinguish between altered crypts and the internal opening of the fistula. Injecting a dye into the external opening of the fistula allows you to more clearly distinguish the internal opening. For this purpose, a 1% aqueous solution of methylene blue, iodine, ink, manganese and other solutions are used.
Restoromanoscopy is an endoscopic technique that involves inserting a special tube equipped with optics into the anus. The doctor can assess the condition of the mucosa and do a biopsy to rule out a tumor if one is suspected.
Fistulography is a radiopaque technique. A contrast agent is injected into the anus, and then x-rays are taken. X-ray examination reveals the presence of pockets, cavities, extensive bays, additional branches and curved fistula tracts.
Transrectal ultrasound allows us to trace the fistula tract in the pararectal tissue, the presence of additional cavities along the course, the relationship of the fistula to the anal sphincter, determination of the internal opening of the fistula, differentiation from pararectal neoplasms. Ultrasound examination is also informative in determining anal sphincter insufficiency after surgery in patients with perirectal fistulas.
Women must receive a referral to a gynecologist for examination to rule out a vaginal fistula.
Treatment methods for paraproctitis
Complete cure is only possible through surgery. Physical therapy, antibiotics, and ointments are used in preparation for or after surgery. Drug therapy can also relieve symptoms and speed recovery. Main recommended pharmacological groups:
- painkillers;
- systemic antibiotics;
- healing ointments.
A course of physiotherapy may include ultraviolet irradiation and electrophoresis.
SM-Clinic specialists diagnose and treat complex pathologies. To make a diagnosis, the doctor collects the patient’s complaints, medical history and objective examination. To clarify the diagnosis and carry out differential diagnosis, additional instrumental studies are performed, such as anoscopy and sigmoidoscopy. These studies are carried out after cleansing the intestines by performing cleansing enemas and taking laxatives.
Surgical treatment of pararectal fistulas
The only indication for surgery is the presence of a fistula.
Contraindications:
- general serious condition of the patient;
- liver and kidney failure;
- chronic diseases in the stage of decompensation;
- blood clotting disorder;
- acute infections in the body.
The operation is usually carried out as planned. In case of exacerbation, the abscess is opened, and the fistula itself is removed after 1-2 weeks.
Preparation for surgery includes standard preoperative examination: blood tests, urine tests, ECG, fluorography. Additionally, rectal examinations and/or ultrasound may be prescribed.
There are several types of operations. A specific type is selected depending on the complexity of the pathology:
- ligature technique;
- excision of the fistula along its entire length with or without subsequent suturing;
- plastic surgery of the internal opening of the fistula;
- laser cauterization of the fistula tract;
- filling the fistula tract.
The surgical intervention is performed in a hospital; from 3 to 10 days after it it is necessary to remain under the supervision of doctors. The effectiveness of the operation reaches 90%.
Postoperative period
In the first days in the hospital, a gas tube is installed, antibiotics are prescribed, and dressings are performed. The pain syndrome is relieved with analgesics. It is important that there are no stools in the first 2-3 days, so a liquid diet is prescribed.
From the second or third day you can eat pureed, easily digestible food, you need to drink a lot. It is necessary to prevent constipation, which can cause the seams to come apart. Sitz baths with antiseptic solutions are prescribed, and, if necessary, laxatives and analgesic ointments.
After discharge, the patient should listen sensitively to his body and, if the following symptoms occur, immediately consult a doctor:
- excessive gas formation;
- fecal incontinence;
- a sharp increase in body temperature;
- constant abdominal pain;
- discharge of blood and/or pus from the anus;
- pain when urinating or defecating.
Basic recommendations for the rehabilitation period:
- eat small portions 6 times a day;
- drink at least 2 liters of water per day;
- do not consume foods that irritate the intestines - carbonated drinks, alcohol, chocolate, hot spices, fatty foods, foods with flavoring additives, etc.;
- give preference to vegetables and fruits as sources of fiber, eat cereals, grain bread and dairy products.
Focus on rapid recovery
In order for rehabilitation to be completed as quickly as possible, you will need to adhere to bed rest for the first few days. You will have to spend a little more than a week following the rules of individual antibacterial therapy.
After successful neutralization of the lesion, you will have to work on holding the stool for about five days. A special diet aimed at preventing the formation of toxins will help with this. If increased peristalsis is observed, the doctor will prescribe appropriate medications to relieve symptoms.
The first dressing occurs on the third day. Here you should prepare for the fact that the process itself is quite unpleasant, so doctors prefer to relieve pain with painkillers for the first time.
Tampons previously placed on the wound surface are first soaked in hydrogen peroxide and then removed. The wound itself is also treated with hydrogen peroxide along with antiseptics, and then loosely filled with fresh swabs with ointment. To speed up healing, a strip of ointment is inserted into the rectum itself.
And after a four-day quarantine, the use of specialized candles is allowed. If you cannot have a bowel movement the next day, then you need to use a cleansing enema.
The list of permitted products for the first postoperative period includes:
- semolina porridge cooked in water;
- broths;
- steamed cutlets;
- boiled fish;
- omelette.
But there are no special restrictions on drinking. But all dishes served to the table should not be salty or include seasonings. After a few days, while maintaining positive dynamics, it is allowed to include some more products in the main menu:
- mashed boiled potatoes and beets;
- fermented milk products;
- fruit puree and baked apples.
Still, soda, raw vegetables and fruits, legumes, and alcoholic drinks are still prohibited.
After each trip to the toilet, you will have to take sitz baths to relieve the condition and provide additional disinfection. The proctologist selects the solution for them individually. He will be the one to tell you exactly when the stitches can be removed, but the average period is often about a week. It will take a few more weeks until the healing is complete.
Partial incontinence of feces and gases over the next couple of months is a standard reaction of the body, so this is not a reason to sound the alarm. To improve the clinical picture, it is necessary to train the sphincter muscles using a special set of exercises.
The main risks associated with paraproctitis
Deep fistulas of the extra- and transsphincteric types often recur.
Long-term progressive fistulas, which are complicated by the process of scarring of the walls of the rectum and purulent leaks, can lead to secondary functional changes.
Periods of new exacerbations are dangerous due to the appearance of fresh foci of inflammation and the involvement of an increasingly larger array of the anal sphincter in the inflammatory process. All of the above inevitably affects the general condition of the patient. Often there are complaints of weakened immunity, headaches, sleep problems, decreased performance, and irritability.
In addition to the above complications, a long-existing fistula can lead to pectenosis, namely a cicatricial change in the wall of the anal canal with decreased elasticity and cicatricial stricture. With a long-term illness, in some cases, malignancy of the fistula tract is possible.
Causes
According to medical statistics, 95% of fistulas located in the rectum are the result of acute purulent paraproctitis. A dangerous infection penetrates deep into the walls of the rectum, which surrounds the tissue. A perirectal abscess forms. Over time, it opens, and as a result, a fistula forms. A rectal fistula is formed if the patient does not consult a doctor on time and ignores the symptoms that appeared in the early stages of the disease.
The cause of acute paraproctitis is also non-radical surgical intervention, which was performed by incompetent doctors.
In some cases, neoplasms appear after injury or after surgery. Occur due to resection of the rectum. In women, proctological pathology is diagnosed much more often. Fistulas that connect the rectum and vagina are the result of birth injuries. This occurs with pelvic recumbency of the fetus, with ruptures of the birth canal, with prolonged labor, and with the use of obstetric aid.
Acute paraproctitis occurs in people who suffer from rectal cancer, tuberculosis, chlamydia, AIDS, Crohn's disease, diverticular intestinal disease, actinomycosis and other diseases.