Fistula in the rectum: causes
In 95% of cases, fistulas are a consequence of acute paraproctitis. Chronic disease most often develops for one of 2 reasons:
- Spontaneous opening of the abscess.
- Refusal of radical surgical treatment of acute paraproctitis, the operation performed included only opening and drainage, while the internal intestinal opening (entry gate of infection) remained.
Fistulas can also occur as a result of pathologies:
- Severe chronic intestinal diseases (Crohn's disease, intestinal tuberculosis).
- Other infectious diseases: syphilis, AIDS, chlamydia.
In some cases, chronic paraproctitis develops after:
- Birth injuries (with breech presentation of the fetus, rupture of the birth canal).
- Rectal resections.
- Gynecological operations.
A prerequisite for the occurrence of a fistula is the presence of infection.
Postoperative care
In the postoperative period, all patients must undergo local and general anesthesia. Local anesthesia includes ointments and suppositories, which can locally reduce the severity of pain. Tablets, capsules, intravenous drugs are classified as general anesthesia. If the pain is significant, potent drugs (narcotic analgesics) are also used in a hospital setting. Your doctor will tell you the regimen for using painkillers, methods of administration, and specific names of drugs.
The average hospital stay is 1-5 days. It depends on the extent of the operation, the presence of complications and some other individual characteristics. During the postoperative period, you will undergo daily dressing changes and monitoring of wound healing. Antibacterial therapy is not indicated for all patients, but only if there are indications determined by the doctor. Mandatory wound care includes washing it with a stream of water at room temperature 3-4 times a day. This facilitates mechanical cleaning and will reduce the risk of infectious complications. The doctor will also show you how to properly perform dressings so that you can do them yourself at home.
Rectal fistulas: classification
The shape of the fistula can be:
- Complete (have two holes, internal and external).
- Incomplete (only with an internal hole).
According to the location of the internal opening in the rectum or anal canal, fistulas are:
- In front of them;
- rear;
- lateral.
According to the nature of the location of the fistula tract relative to the external anal sphincter, the fistula can be:
- Intrasphincteric (subcutaneous mucous) - does not affect the internal and external sphincters of the rectum, passes through the wall of the rectum (the most direct and short fistulous tract, detected in 25-35% of patients).
- Transsphincteric - passes through the sphincter and the wall of the rectum, diagnosed in 40-45% of people suffering from chronic paraproctitis.
- Extrasphincteric - completely bends around the sphincter, then passes along the wall of the rectum and exits onto the mucous membrane of the rectum, detected in 15-25% of patients.
The exits of all of the above fistulas are located as follows: one is located on the skin next to the anus, the other is in the area of the Morganian crypts.
Extrasphincteric fistulas are classified according to severity:
- 1st degree - there are no abscesses, scars, infiltrates, and the internal opening is narrow.
- Grade 2 – there is no inflammatory process in the fiber, but there are scars on the tissue in the area of the internal exit.
- 3rd degree - a purulent inflammatory process is detected in the tissue, the internal exit is narrow, there are no scars next to it.
- Grade 4 – purulent-inflammatory processes or infiltrates are present in the fiber, the internal exit is wide, and large scars are observed around it.
The appearance of a fistula due to unsatisfactory canal filling
Canal filling is a fairly common dental procedure indicated in the treatment of diseases such as periodontitis, pulpitis and in preparing teeth for subsequent prosthetics. However, in more than half of the cases, the canals are not filled as well as required by the rules. The most common mistake is filling not to the very top of the root.
Due to a mistake made by the doctor, an infection will form in the unsealed area of the canal over time, which sooner or later will go beyond the boundaries of the tooth and lead to inflammation. In addition to filling the entire length of the canal, the substance used to fill the canal during the procedure must be packed tightly: the appearance of voids and the formation of pores is unacceptable.
The main symptom indicating problems with the tooth is pain when biting. If you look carefully, in the immediate vicinity of the diseased tooth you can easily find a small hole through which pus will come out.
The appearance of a fistula on the gum, the treatment of which is not recommended to be delayed, indicates that the tooth will not stop hurting on its own. To treat it, the tooth is unfilled, an anti-inflammatory medicine is placed in the canals, which is removed after a certain period of time, and the canals are then filled again.
If a tooth has a crown or a pin, unfilling the canals becomes a real problem for the doctor. It is not always possible to remove the pin, and the crown will have to be re-installed after the procedure is completed, which is fraught with additional financial costs for the patient. Sometimes, if the canal is not sealed at its very end, the doctor decides to resort to a procedure for resection of the upper part of the root.
Resection is far from the most difficult operation: its duration is no more than an hour. The operation consists of several main stages:
- Preparation, during which the canals are carefully sealed a couple of days before the main procedure.
- Anesthesia. The operation is performed under local anesthesia: the patient does not feel pain during the doctor’s manipulations, but discomfort may occur later when the effect of the injection wears off.
- Gaining free access to the upper region of the root. To do this, the dentist cuts the gum, exposing the bone tissue, in which a hole is then cut using a drill.
- Through the resulting hole, the doctor cuts off the tip of the root, to which, as a rule, the cyst is attached, which causes inflammation.
- After removing part of the root, an empty cavity remains in the bone. The doctor can fill the space with synthetic tissue, which speeds up the growth process of natural bone.
- The final stage is suturing the gums. For intensive outflow of ichor, drainage can be installed for several days.
Fistula in the rectum: symptoms
Characteristic signs of chronic paraproctitis are:
- The fistula opening, located on the skin next to the anus, visually resembles a small wound.
- Discharge with an unpleasant odor from the external fistula tract (pus, ichor), which is why the patient has to regularly perform hygiene procedures or wear pads.
- Itching, burning, wetness (due to discharge from the external opening) in the anus.
- Periodic slight increase in body temperature.
Reference! Pain in chronic paraproctitis is rare. As a rule, they occur when the fistula opening is blocked by dead tissue or pus. This can intensify and aggravate inflammation, as pus accumulates in the fistulous tract.
Anesthesia
For surgical interventions in the perineal area, regional anesthesia is currently used. It includes subarachnoid (spinal) anesthesia at the lumbosacral level, which allows you to block the transmission of sensory and painful nerve impulses to the lower part of the body, including the anorectal area. In this case, the motor function of the lower extremities is not lost. Subarachnoid anesthesia is a fairly safe method and has a low risk of complications from the heart, respiratory system and nervous system. During the operation, for maximum comfort, the patient is conscious or in a state of medicated sleep (sedation). General anesthesia in anorectal surgery is used in individual cases at the discretion of the anesthesiologist-resuscitator.
Complications of chronic paraproctitis
If left untreated, the following complications may occur:
- Regular exacerbations with the appearance of purulent cavities and infiltrates in the soft tissues.
- The appearance of scars in the anal canal, soft tissues near the anus, or the muscles of the anal area.
- Decreased potency.
- Deformation of the anal canal or rectum.
The listed signs may be accompanied by the following symptoms:
- General malaise.
- Increased body temperature.
- Swelling in the anus.
Symptoms and manifestations of pathology
Pararectal fistula symptoms are pronounced, the clinical picture is characterized by wave-like symptoms, alternating stages of exacerbation and remission. Depending on the stage, the symptoms of the disease are as follows:
- the presence of a wound (fistula tract) in the perianal area;
- rectal discharge (purulent, serous-purulent, sanguineous), noticeable on underwear;
- unpleasant odor of discharge;
- hyperemia of the skin around the anus, itching, burning;
- dull pain in the rectum, intensifying during bowel movements and receding after defecation due to the outflow of purulent exudate;
- a significant increase in pain during exacerbation (the appearance of an abscess in the perirectal tissue) - in the pelvis, rectum, lower abdomen, especially during bowel movements, walking, coughing;
- disturbances of urination and fecal excretion;
- temperature increase;
- signs of intoxication;
- headache;
- weakness, decreased motor activity.
After opening the fistula, remission occurs, but the wound does not heal, since the inflammatory process does not stop, the formation and outflow of exudate continues, as a result of which the patient’s sleep is disturbed, loss of performance, and disorder of sexual functions and nervous system occur.
With the development of a transphincteric fistula, the following symptoms are observed during a hardware examination of the patient:
- deformation of the anal canal;
- dysfunction of the sphincter;
- scarring of the sphincter muscles;
- disruption of the process of defecation up to fecal incontinence.
Despite the severity of the clinical picture, an incomprehensible shyness keeps some patients from turning to professional doctors. Self-medication is carried out with local drugs, although in case of perirectal fistula, treatment without surgery does not give a lasting effect and can lead to serious complications.
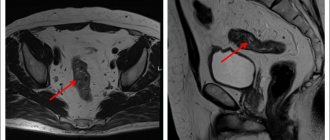
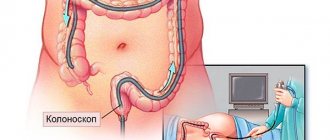
Diagnostics
Diagnosis of fistulas is carried out during an examination by a proctologist.
The patient is positioned on a gynecological chair. The external fistula opening in the anal area is determined visually. The presence of scar tissue along the fistula can be detected using digital examination. However, this method is suitable for intrasphincteric and transsphincteric fistulas. Extrasphincteric fistulas are not easy to diagnose using this method.
Also used to diagnose fistulas are:
- Sphincterometry is a hardware diagnostic method used to assess sphincter tone.
- Probing the fistula - determining the direction of the fistula tract.
- Sigmoidoscopy – assessment of the condition of the rectal mucosa.
- Fistulography is an x-ray examination using a contrast agent.
- Ultrasound of the rectum.
Fistula due to root perforation
Working with canals requires the dentist to be careful, attentive, and precise, controlled movements. The slightest carelessness can lead to the formation of a non-physiological hole (perforation), which will subsequently cause inflammation and, as a consequence, the appearance of a fistula.
A common mistake that leads to perforation and inflammation is the fixation of the pin when it is installed not along the canal, but its removal into the bone tissue.
With perforation, treatment of the fistula is the most problematic of all cases of its formation. Moreover, the main difficulty is not in medical procedures, but in the behavior of dentists who do not inform patients about the complication that has arisen, so as not to question the professionalism of themselves and their colleagues. As a result, a person who goes to the hospital for dental treatment returns again due to pain and inflammation: often the process becomes so advanced that it is no longer possible to do anything other than remove the tooth.
But still, perforation is not a death sentence, and the tooth can be saved. The sooner the patient applies, the greater the chance that the treatment will be completed successfully. True, this requires expensive materials (Pro Root MTA is often used), with the help of which the perforation area is sealed. Sometimes filling is performed directly through the canals, sometimes a surgical incision is required to gain visual access to the damaged area.
Rectal fistula: treatment
Treatment of rectal fistulas can only be surgical. Conservative therapy will not give the desired result. There are several types of operations used for this disease. However, the main goals of all methods are:
- Elimination of the fistula tract along with the external and external exits (if purulent leaks are detected, they are opened and drained during the operation).
- Preservation of the function of the muscle that compresses the anus (this is impossible only in the case of radical surgery).
When choosing a treatment method, be sure to take into account:
- Location of the fistula tract.
- The presence of infiltrates, purulent cavities, scars.
- General condition of the patient.
Modern methods involve closing the internal outlet of the fistula using the patient’s own tissue. They are taken from the wall of the rectum located above the opening.
As a rule, complex preparation for surgery is not necessary. I usually perform a cleansing enema the night before and the morning before surgery. Before surgery, the patient does not eat or drink. But in especially severe cases, mechanical bowel preparation is necessary, during which special solutions of laxatives are used.
The postoperative period usually lasts 2-3 weeks, during which complete recovery occurs. Thanks to the effectiveness of modern painkillers and antimicrobial medications, already on the 2-3rd day the patient can be released for further treatment on an outpatient basis. Working ability returns within 1-1.5 weeks. Rarely, the rehabilitation period can be 1.5-2 months, subject to reduced tissue regeneration.
Rehabilitation after fistula removal
The recovery period depends on the patient's condition. Complete rehabilitation occurs after a month and a half, but during this time you can lead a normal life, excluding strong physical activity.
You must stay in the hospital for 2-3 days after excision of the fistula. Our medical staff will monitor the change of antibacterial dressings, the condition of the wound, and the administration of medications.
During recovery, the patient must follow a diet - exclude foods containing coarse fiber, eat mostly soft milk porridges, drink juices and water.
After surgery, you need to listen to the doctor's recommendations. Professional personal hygiene and diet promote rapid healing of the postoperative suture.
Fistula on the gum: what to do?
The most important thing that a person who has pain in the gums should understand is that they need to see a doctor as soon as possible, and not wait for the symptoms to disappear and not use various gels and other means. Yes, they can bring relief, but it will be a temporary relief of symptoms, not healing.
There are several treatment options for fistula.
Endodontic method for treating gum fistula
The method is applicable if the following conditions are met:
- the dental canal and its branches are visible;
- it is clearly visible in the tooth canal whether there are cracks or not.
Treatment is carried out under a microscope. The apical part is sealed with modern high-quality materials that are biocompatible with natural tissues. Canal therapy is performed, which allows the fistula to be eliminated.
Mixed treatment
If the lesion is quite severe, the therapist will need the help of a surgeon.
The therapist cleans the canals and seals the apical part of the root. The surgeon's job is to polish this area of the root. Polishing is carried out using ultrasonic nozzles, which allows you to achieve an ideal result.
Surgery
If the inflammatory process has gone too far, the tooth will have to be removed. The source of inflammation is eliminated along with the tooth and root.
In the future, an implant can be installed in this place at the request of the patient: this is a rather expensive procedure, so it is not recommended to delay the treatment of the fistula. The earlier the patient consults a doctor, the easier and cheaper it will be to cure the disease.
Autotransplantation
This is a type of surgical treatment. In this case, the implant is another tooth of the patient (as a rule, it is a wisdom tooth, which is a kind of reserve, since it is not involved in chewing food).
The advantage of the method is that the person’s own tooth is transplanted, which negates the risk of tissue rejection.
Symptoms of appearance
The process of fistula formation is difficult to track; it can take several days, as happens with acute pancreatitis, or several months, as with post-radiation tissue changes.
Manifestations at the initial stage of fistula formation are due to its root cause, as a rule, a local inflammatory process resulting in purulent melting of tissue with pain and infiltration, often intoxication and fever.
Without an exacerbation of the inflammatory reaction, the fistula can be felt as a cord. The size of the compaction around the fistula tract is due to inflammatory infiltration and branching of the fistula tracts themselves, cicatricial changes in the surrounding tissues, previously involved in the inflammatory conglomerate.
A formed fistula has an entrance and, sometimes, an exit, the tissues around it are compacted, and discharge can be squeezed out of the hole: pus, bile, pancreatic juice, and so on. With a fistula, feces may leak from the intestine into the vagina from the genital organs; when there is an anastomosis of the intestine with the bladder, urine leaks from the anus. The discharge from the intestinal fistula has a fecal smell, and the purulent secretion from the vagina also has a specific smell. The smell of a discharged fistula, leading from the zone of disintegration of a malignant tumor, seems especially heavy to others.
Inflammation causes pain ranging from slight discomfort to unbearable pain. Tumor fistulas do not hurt because they form inside a disintegrating tumor.
When the infection activates with the formation of streaks of purulent contents, a general reaction occurs: intoxication, high temperature, sweating and pallor, palpitations and rapid breathing.
Prevention of fistulas
Not all diseases can be prevented, especially fistulas, which complicate the course of purulent paraproctitis. However, it is possible to adequately treat the diseases that lead to paraproctitis - hemorrhoids and fissures, and this is precisely what will prevent the formation of fistulas.
Complicated childbirth cannot be prevented, but high-quality and timely obstetric care, attentive attention to the woman and a thorough postpartum examination are available preventive measures.
The high incidence of post-radiation tissue damage and fibrosis progressing over time forced oncologists to abandon high doses of radiation therapy and even change approaches to the treatment of malignant tumors of the genital area.
Particular importance is attached to the correct choice of method of surgical treatment of diseases of the hollow organs and adequate management of the postoperative period.
In our clinic, a complicated course of the disease is very rare, because we not only know about prevention methods, but also actively use them.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Shelygin Yu.A., Blagodarny L.A. /Handbook of coloproctology// -M.: Litterra; 2012.
- Becker A., Koltun L., Sayfan J. /Simple clinical examination predicts complexity of perianal fistula// Colorectal Dis.; 2006; 8.
- Gaertner WB, Hagerman GF, Finne CO, et al. /Fistula-associated anal adenocarcinoma: good results with aggressive therapy// Dis Colon Rectum; 2008; 51.
- Genadry RR, Creanga AA, Roenneburg ML, Wheeless CR /Complex obstetric fistulas // Int. J. Gynaecol. Obstet.; 2007; Vol. 99; Suppl. 1.
- Ommer A., Herold A., Berg E. / S3-Leitlinie: Rektovaginale Fisteln (ohne M. Crohn) // Coloproctology; 2012; Vol. 34.
- Sahni VA, Ahmad R., Burling D. / Which method is best for imaging of perianal fistula?// Abdom Imaging.; 2008; 33.
- Zoulek E., Karp DR, Davila GW/ Rectovaginal fistula as a complication to a Bartholin gland excision // Obstet. Gynecol.; 2011; Vol. 118; N 2.