It’s no secret that our women sometimes really don’t like to “go to the doctors” - either they don’t have the time, or they don’t have the desire. But everyone considers herself a fool when choosing contraceptive methods, relying on advertising, advice from girlfriends and the Internet. As a result, a woman who seems to be constantly taking contraception suddenly becomes pregnant, cursing modern contraception. It doesn’t occur to her that she has to blame herself.
The selection of contraceptives is the field of activity of a gynecologist. At the same time, the doctor carefully considers the tactics, assessing the results of the examination, tests, age, weight and health of the patient. The result of a wise choice is exclusively desired children and the absence of abortions in the medical record.
The barrier method is not a panacea
The content of the article
Some patients, not wanting to “bother” with contraception, simply buy a package of condoms at the nearest supermarket. In case of casual relationships, such a remedy is, of course, given the green light, but for a couple in a permanent relationship, such protection is archaic.
First of all, during sexual intercourse using a condom, sperm does not enter the woman’s body, which is not very good. The ejaculate contains hormones and substances that improve the condition of the skin, normalize the vaginal flora and even have an antidepressant effect. In addition, condoms break and, which is no secret, reduce the severity of sexual sensations. Because of her reluctance to see a doctor, a woman deprives herself and her partner, who is forced, figuratively speaking, to “smell flowers in a gas mask.”
Most other methods (caps, suppositories with spermicide, diaphragms) are not very popular, which is understandable. They are difficult to use correctly, and partners often feel a foreign body in the vagina. Rarely will a woman want to be distracted in a romantic setting to insert a cap or diaphragm, and then take it out, wash and dry it!
IUD: intrauterine therapy system
The hormonal intrauterine system is unanimously recognized as one of the most effective and safe means of hormonal contraception. Its action is based on the regular release of the progestin levonorgestrel. The Pearl index (the number of pregnancies that occurred during the year when using the drug) is 0–0.2. Duration of validity - up to 5 years. In addition to the contraceptive effect, the hormonal IUD significantly reduces menstrual blood loss (by 75%), so it is used as a treatment for menorrhagia.
Tablets, like Svetka’s
It’s a paradox: Russian women don’t trust their girlfriends with haircuts and manicures, but they don’t trust their own health. When choosing birth control pills, the advice of friends who pass on centuries-old myths to each other is especially effective.
But modern birth control pills are very different: microdosed, low-dose, high-dose. With various hormones that can not only protect against pregnancy, but also treat various diseases. Such diversity is necessary in order to choose the best option for each woman.
Oral contraceptives are:
- Monophasic.
These tablets contain equal amounts of estrogen and progestin. They are considered obsolete but are still used. Their disadvantage is large doses of hormones that do not correspond to natural fluctuations in hormonal levels. Plus - a therapeutic effect when you need to quickly correct the female cycle. - Two-phase
. The estrogen content in them is the same, and the amount of gestagen varies depending on the day of the menstrual cycle. The pills are closer to the actual cycle fluctuations. They are well suited for women with increased androgen levels. - Three-phase
. The doses of hormones in these drugs change three times during the menstrual cycle. These are the most modern pills, most suitable for the cycle, but also the most expensive. By the way, they are not suitable for some women. - Microdosed
. Tablets with a minimum hormonal dose, recommended for young girls under 25 years of age. - Mini-drinks.
They contain only gestagen. They increase the viscosity of cervical mucus, making it difficult for sperm to move into the uterus. Ovulation when taken is blocked in only half of women. Such tablets are prescribed to women breastfeeding - they will not harm the baby.
Contraceptives containing hormones are not forgiving. As a result of “self-preservation,” women “earn” amenorrhea (absence of menstruation), excess weight, and can even become pregnant.
The whole truth about modern methods of contraception
Dobrokhotova Alina Danilovna
Obstetrician-gynecologist
March 26, 2020
Is it possible today to find a modern, affordable and 100% effective method of contraception? And also with a minimum number of side effects? How many more questions does a woman face who wants to reliably protect herself from unwanted pregnancy? The lack of understandable information leads to an increase in the percentage of abortions and unplanned pregnancies. I propose to look into this issue.
Analysis of different types of contraceptives
To begin with, there are several methods of contraception, and each group is assessed by the Pearl Index (PI). This is the number of pregnancies occurring in 100 women during the year using one or another method (the lower the index, the better).
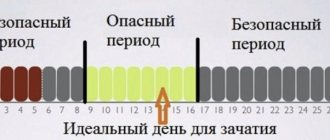
Calendar method (PI = 1-10)
With a regular menstrual cycle, “dangerous” and “safe” days are determined. For example, with a 28-30 day cycle, a couple should abstain from unprotected sex from about days 8 to 19, when the risk of pregnancy is highest.
For free. No side effects. Unreliable. Is it worth it? If you and your partner are ready for all twists of fate, trust each other 100%, you can try it.
Coitus interruptus (PI = 4)
The story is similar to the one described above. Are you ready for your child in case of an “accident”? Practice. There are always many questions about the possibility of pregnancy, even if ejaculation does not occur in the vagina. There have been no large-scale studies, but it has been proven that pre-ejaculate (the clear liquid released from the penis during intercourse before ejaculation) may contain active sperm, although there are men who have virtually no sperm. This fluid is stored in the urethral canal, and the pregnancy rate is higher with frequent sexual intercourse. For many couples, this method of contraception has been successful for a long time. I would also like to draw your attention to the fact that if pregnancy does not occur during PPA (coitus interruptus), this does not indicate problems with conception! You should consult a doctor after 12 months of regular (2 times a week) unprotected sexual activity and ejaculation in the vagina. Does not protect against infections. Be careful!
Condoms (PI = 2-5)
Male and female; latex and polyurethane; with smells/tastes/light effects - whatever your heart desires! Contraceptive effect is almost 100%, the same degree of protection against STIs (sexually transmitted infections). Each package contains instructions, but remember to change the male condom after each sexual intercourse and select the correct size! As for female devices, they can be used for several hours in a row (up to 6 hours!) and only then thrown away. Such a large Pearl index (compared to the same hormonal pills) is due to:
- improper use of condoms,
- using oil-based lubricants (the latex product may tear),
- saving and purchasing low-quality goods (it is better to purchase these types of contraceptives at the pharmacy).
Minimum side effects with a very high degree of protection!
Chemical method (spermicides) (PI = 3)
These are substances that inactivate sperm in the vagina, preventing them from passing into the uterus. The release form is different (foams, jelly, melting candles, foaming candles and tablets, soluble films and sponges). Everything is used topically, that is, inserted into the woman’s vagina. Can be used at any period of sexually active life: by teenagers and breastfeeding women. Some people use the products as an independent method of protection, but most often a combination with a barrier method of contraception is recommended. To some extent they can protect against infections, but there is no evidence in favor of high safety. You should also be clearly instructed, because each form of release implies its own method of use, including time. Well, don’t forget about possible allergic reactions. Lactational amenorrhea
(PI depends on the time elapsed after birth, on average 2-10)
The method is considered very reliable if a woman breastfeeds 24/7, including at night, the break between feedings is no more than six hours, and there is no menstruation. But you should know that even in the absence of bleeding, ovulation can occur and pregnancy can occur. Mothers should contact a gynecologist who will help with choosing the most suitable method. Please note that hormonal contraception is allowed only six weeks after birth, and COCs (combined oral contraceptives) are completely prohibited for the entire period of breastfeeding. You should not completely trust this method of contraception, especially five months after delivery.
Intrauterine device (PI < 1)
Yes, they are both hormonal (with levonorgestrel) and regular, i.e. copper. Both types are also allowed for breastfeeding women, and it is even practiced to install them immediately after childbirth, but then there is a high probability of expulsion (loss). The spiral has the shape of the letter T, at the end of which there is a “tendril”; it is inserted after examination by a gynecologist and the exclusion of acute inflammatory processes. The procedure is almost painless and can reliably protect a woman from unwanted pregnancy for a period of three to five years. The IUD (intrauterine device) is also used to treat endometriosis or heavy menstruation, leading to complications such as anemia. When installing the copper version, unprotected sex life is allowed immediately, after using the hormonal version - after seven days. This device copes with its contraceptive task by thickening the cervical mucus (sperm are unable to pass into the uterus). In the uterus itself, it also prevents the attachment of the embryo. In addition, if we are talking about a hormonal IUD, then levonorgestrel blocks ovulation, and fertilization does not occur. After installation, you need to see a doctor in 3-4 weeks for an ultrasound. This type of contraceptives is also allowed for adolescents and nulliparous women. Everything seems to be fine, but! Not a single spiral can kill an infection.
Progestin-only drugs (PI < 1)
There are also many options:
- Tablets (drink every day at the same time with a maximum allowable difference of +/- 3 hours)
- Injectable forms (in depot form, used four times a year)
- Implantation option (“implanted” subcutaneously on the inside of the shoulder area for three years)
Such drugs are designed for breastfeeding women, as well as for those for whom combined contraceptives with estrogens are completely contraindicated. These include smoking women over 35 years of age who have:
- Arterial hypertension
- Deep vein thrombosis
- History of strokes
- Hereditary thrombophilias
- Migraines with aura
- Past or present breast cancer
- Complications of long-term diabetes mellitus
Let's look at each group in more detail.
Progestin pills , or mini-pills, contain only one group of hormonal substances (progesterone series) and prevent fertilization by suppressing ovulation, increasing the viscosity of cervical mucus, and turning the endometrium into “unsuitable”, thin for embryo implantation. You can start taking it six weeks after birth, continuously. When taking it, there are no periods at all, but you need to keep in mind that there are side effects: menstrual-like bleeding, decreased libido, breast tenderness, slight weight gain. The main word is “happens”, since it is not at all necessary that all of the above will happen to you. The ideal method is when the couple has regular sex life and complete trust (after all, there is no need to use a condom). A few words about the injection method . There is no need to constantly think about when you should take the pill, buy condoms, or run to the bathroom just before sexual intercourse. This is an effective method of contraception with timely repeated injections. You can use it until menopause, but you should know that this method greatly reduces bone mineral density. If this method is still closer to your heart and other organs, get rid of bad habits, add light physical activity and calcium supplements to your daily life. What kind of implant ? A well-prepared device in the form of a pen with a small blade at the end, charged with a “bomb” with a hormone, gets under the skin with one slight movement of the gynecologist’s hand.
The method is completely reversible at any time. Specific side effects: pain at the injection site during the first few days.
Summary for progestin medications:
- Can be given to breastfeeding women as early as six weeks after giving birth.
- It is possible for those for whom estrogen-containing drugs are contraindicated.
- You can choose the most suitable method for each woman and case.
- The most common side effects are slight weight gain, breast tenderness and decreased libido.
- All methods are reversible, and pregnancy is possible already in the next menstrual cycle after discontinuation.
Combined contraceptives (PI <1)
Hormonal patch, vaginal ring and demonized pills (COCs). As the name implies, they are distinguished from the previously described group by their composition: these drugs contain both progesterone and estrogen (ethinyl estradiol, to be more precise).
We glue the patch to the skin, and now you are safe! On the dry skin of the shoulder, buttocks, back or abdomen, once a week on the same day, we attach a flesh-colored patch containing hormones on its inner part. Yes, it can be accidentally washed off with water, it can get caught on clothing and come off, it can be noticed, which violates the privacy of the contraceptive method, and don’t forget about local allergic reactions. The main thing is to notice a defect in the adhesive or loss of the patch in time: a woman has 48 hours to protect herself from an unwanted pregnancy.
There are also advantages, of course:
- The active substance does not pass through the liver.
- Fertility (the ability to become pregnant) is quickly restored.
- Few side effects.
Now to the know-how of contraceptives: the vaginal ring . The woman installs it in the vagina on her own once every three weeks. An original way of receiving a combination of hormonal substances. Within 21 days, the required amount of progesterone and estrogen is absorbed into the body through the mucous membrane of the genital organs. Next, we pull it out and get a menstrual-like reaction.
In my opinion, one of the best methods of protection:
- You will not miss/forget/lose your contraceptive.
- The partner does not feel this adaptation.
- You really are under reliable protection, except for infections, of course. Hormones cannot kill foreign agents.
COCs (combined oral contraceptives), i.e. they are progesterone + estrogen, which are taken orally daily. At the moment, this is the most studied group of modern contraceptive methods. In the era of the 21st century, the use of high-dose drugs is a thing of the past, along with unwanted side effects. All a woman needs is to find a competent specialist, undergo a small range of examinations and choose the most suitable combination. The price category is comparable to the methods described above. What should you pay attention to? On your life history, existing diseases and the desired effect of taking it. Of course, here we are talking exclusively about contraception, but with the help of pills you can get rid of some symptoms that interfere with a comfortable life (heavy and painful menstruation, acne, hirsutism, increased sensitivity of the mammary glands in the middle of the cycle and before menstruation, etc.). Reliable? Undoubtedly, but only if the woman follows all the recommendations for taking it and carefully reads the instructions for missing pills. COCs should be taken from the first day of menstruation (when bleeding begins) or from the fifth day (no later), and then an additional method of contraception should be used for the first week. Release form: 21, 24, 28 tablets; long-acting preparations are also available. Yes, yes, every woman, together with her gynecologist, can postpone menstruation for a period of rest, a date, for example, or a sports competition. I advise you to use it with a regular sexual partner and will not tire of talking about infections. Be careful! You must understand that hormones do not affect weight gain/decreased libido/hormonal imbalance! The image of the drugs is greatly discredited, which does not allow patients to clearly understand this complex group of contraceptives. There is no specific name in my message, since self-medication is dangerous. Your task is to come to an appointment with a gynecologist, ask all your questions, determine the most suitable method of contraception and leave without fear of multi-colored pills in a pack.
Don't trap yourself in reproductive risks!
Implants, patches and injections
For women who are hesitant to take birth control pills because they are afraid of missing another pill, the doctor will offer several methods to choose from:
- Contraceptive implants
. Installed under the skin of the forearm for up to three years. The hormones they contain suppress ovulation, like pills, but do not require any action on the part of the woman. Efficiency – 98%. Implants need to be changed periodically. If a woman wants to get pregnant, ovulation will resume three months after removing the contraceptive. - Contraceptive patch.
Sticks to any part of the body and does not come off while showering, swimming or taking a bath. The hormones it secretes block ovulation and protect against pregnancy. - Contraceptive injections
. They are done by a doctor once every three months. Before the drug is administered, the woman is examined, because the injection cannot be canceled.
Since all these products have a long period of use, the patient undergoes hormone tests before using them. Incorrect selection threatens the cessation of menstruation, bleeding and increased bone fragility.
What gynecologists say
Of course, gynecologists are against natural contraception. And this is understandable: after all, they are the ones who have to terminate unplanned pregnancies.
The unreliability of natural methods is associated with the characteristics of each woman’s body; the cycle can go wrong even due to mild stress or taking common medications for fever. It will not be possible to quickly trace the problem, so the likelihood of calculation errors increases.
And is there any point in taking such risks when there are many reliable methods of protection. Moreover, many of them are also used for medicinal purposes - normalization of the cycle, hormonal levels, regulation of the volume of menstrual discharge, additional protection against infections. The variety of modern contraceptive drugs allows you to choose a method for a woman of any age, health and with any frequency of sexual activity.
For example, women who are breastfeeding can use a uterine device, which is inserted 6 weeks after giving birth. Progestin-only tablets are also suitable for breastfeeding as they do not have any effect on the composition of the mother's milk.
Progestin is a very gentle drug that does not interfere with lactation and ovulation, and does not disrupt a woman’s menstrual cycle. It only changes the consistency of cervical mucus to very thick, making it an obstacle for sperm. The mucous membrane in the uterus also undergoes changes, causing the inability of the embryo to attach.
For young girls, special mini-pill tablets are suitable. And for women before menopause, a gynecologist-endocrinologist selects pills based on the results of hormone tests.
Gynecologists at the Diana Medical Clinic will select the most suitable method of contraception for you and provide detailed advice on how to use it.
If you find an error, please select a piece of text and press Ctrl+Enter
IUD: put it in and forget it
One of the most popular methods of contraception is intrauterine devices. They are comfortable, do not require distraction before sexual intercourse and do not dull sensations during intimacy.
An IUD is installed for up to 10 years. Some models have a container with hormones that fight genital diseases and thicken mucus to protect against sperm penetration and infections. The two-in-one contraceptive is very reliable.
The effectiveness of the IUD reaches 90%. Where do the 10% of losers come from? These are women who believed in the “almighty infinite power of the spiral.” Having installed an intrauterine device, they do not visit a gynecologist. The spiral moves - the woman becomes pregnant. Some IUD patients don't even remember when their last menstrual period was! This attitude towards one's own health is unacceptable.
Surgical contraception
Female sterilization can take place using a wide variety of methods.
- Laparoscopic tubal ligation is a reversible surgical contraception. Can be performed under local anesthesia. There are practically no scars on the abdominal wall, and postoperative recovery takes no more than a day.
- A minilaparotomy is performed through an incision in the abdominal wall, which involves a small scar. Moreover, the operation does not require expensive equipment and is accessible to all social strata of the population.
- Sterilization with colpotomy access is performed from the perineum. The fallopian tube is removed from the rectal-uterine space into the vagina, ligated, compressed and sutures are applied. This method provides a high aesthetic effect, affordable cost due to the use of standard surgical equipment and a short recovery period.
Despite the radical nature of the surgical method of contraception, additional attention is required to the timing of the intervention. In particular, the operation cannot be performed immediately after childbirth.
Male sterilization
- Vasoresection - ligation of the spermatic cord. The operation is reversible and does not subsequently require microsurgical operation to stitch the duct. In addition to the sterilizing effect, this method of contraception can be used to naturally increase libido, as well as to relieve the inflammatory process after removal of a prostate tumor.
- Vasectomy is cutting of the vas deferens. Until recently, the operation was irreversible and was performed only if there were serious indications or if there was at least 1 child. Today, thanks to the development of technical equipment, in 90% of cases it is possible to completely restore the patency of the spermatic cord.
In most cases, the operation is reversible (recovery will require precise microsurgical intervention), but this approach is still considered the most radical way to protect against unwanted pregnancy. Therefore, before making a final decision, it is recommended to carefully consider and justify your choice in favor of this method of contraception.
Preparing for insertion of the IUD
Before installing a gynecological spiral, you need to be examined in detail by a gynecologist. Diagnostics includes:
- gynecological examination with taking smears to determine the degree of vaginal cleanliness and oncocytology;
- examination of the mammary glands;
- general blood analysis.
At the time of the procedure, the woman should not have inflammatory or other diseases of the female genital area that could cause complications. All pathological conditions are first treated, and then, after a follow-up examination, the gynecologist decides whether to insert an IUD or not.
If you can still use this method of contraception, then immediately the day before the insertion procedure you should stop using intimate hygiene products and sexual intercourse.
What needs to be done to decide on the choice of hormonal contraceptive?
- Visit to the gynecologist. During the interview, the doctor will be able to find out what exactly the woman wants to get from hormonal contraception and suggest the optimal drug for her. The doctor also determines contraindications for taking certain hormonal contraceptives.
- During the visit after the interview, the doctor examines the woman in a chair and takes swabs. First of all, you need a cytology smear from the surface of the cervix and from the cervical canal (the so-called cervical cancer screening, Pap test).
- Ultrasound of the pelvic organs and ultrasound of the mammary glands/mammography in the first phase of the cycle.
Life in the first time after insertion of the IUD
Immediately after placing the contraceptive, the following side effects may occur and should go away on their own:
- cramping pain in the lower abdomen (only the first two days);
- spotting spotting (first two weeks);
- heavier menstrual flow (first two to three months);
- swelling of the mammary glands and acne (caused by hormonal IUDs).
- During the first ten days after installation of the spiral, the following rules must be observed:
- refuse sex;
- do not use sanitary tampons;
- do not douche;
- do not take a bath (it is also prohibited to visit the pool and sauna);
- Do not perform heavy physical work.
- For severe nagging pain, you can put a suppository with indomethacin or take a No-shpa tablet.
COC: both treatment and prevention
The results of studies from 20 countries around the world showed that women currently taking COCs, as well as those who have taken them for the past 1-4 years, have a slightly increased risk of developing breast cancer. It is assumed that COCs may potentiate the underlying cause of breast cancer.
Under the capacious and even slightly ridiculous abbreviation COC, very serious drugs are hidden - combined oral contraceptives. They are radically different from their progenitor, which contained horse doses of hormones: 150 mcg of estrogen mestranol and 10 mg of the gestagen norethinodrel. Modern oral contraceptives contain 20–35 mcg of estrogen (most often in the form of ethinyl estradiol) and an extremely low dosage of gestagens.
By the way, about gestagens. In recent decades, scientists have been able to synthesize new progestins that have a pronounced therapeutic effect. Thanks to this, COCs have become full-fledged therapeutic drugs used both in monotherapy and as part of complex treatment of various diseases.
Thus, for acne, combination drugs are prescribed containing cyproterone acetate, drospirenone or desogestrel as a progestin. Women suffering from hirsutism are advised to use COCs with antiandrogenic properties - combinations of estrogen and cyproterone acetate or drospirenone.
All COCs significantly reduce the duration and severity of menstrual blood loss. Particularly effective in such cases are drugs containing estradiol valerate and dienogest. The real scourge of most women is premenstrual syndrome (PMS), which develops in 70–90% of cases [2]. The use of combined hormonal drugs can significantly reduce chest discomfort and pain, and combinations of drospirenone and ethinyl estradiol also improve the psycho-emotional state. It is this complex that is recognized as the most effective for correcting PMS symptoms [3].
Particular attention today is paid to the ability of COCs to reduce the risk of developing benign and malignant neoplasms in the pelvis. It has been proven that the use of modern combinations can reduce the likelihood of ovarian cancer by 40%, and endometrial cancer by 50% [4]. Moreover, the protective effect persists for 15 years after discontinuation of the drug.
Follow-up with a doctor
If a woman feels well, then a follow-up examination by a gynecologist should be done 10-14 days after the insertion of the IUD. If you experience a high or low-grade fever, severe bleeding and pain, or an unpleasant odor from the vagina, you should immediately run to the doctor.
An examination by a gynecologist is also necessary in the following cases:
- if you feel a spiral in the vagina;
- you suspect pregnancy;
- menstruation did not occur within 4-6 weeks;
- pain and bleeding appeared during sexual intercourse.
If the spiral is installed correctly and the procedure has a good outcome, observation by a gynecologist should be carried out as usual (once a year).
Contraindications to hormonal contraception
- Woman's age. Age over 35 years increases the risk of thrombosis. This factor becomes especially important in the presence of additional risk factors for thrombosis, such as: smoking, obesity, frequent long-term flights, and a hereditary predisposition to thrombosis.
- Smoking
- Obesity
- Presence of arterial hypertension (increased blood pressure)
- Hereditary predisposition to thrombosis (cases of heart attacks, strokes, thrombosis and thromboembolism in close relatives at a relatively young age - up to 50 years).
- Liver diseases (cholelithiasis, cholestasis of pregnancy)
- History of complicated pregnancy (abnormalities in liver function during pregnancy; placental abruption, development of preeclampsia/preeclampsia: increased blood pressure, edema, abnormal urine tests)
When should an IUD be removed?
The service life of intrauterine gynecological devices ranges from 1 to 7 years. At the request of the woman or after the time of using them has expired, you need to consult a doctor again to have them removed. Removing the spiral on your own is impossible and is fraught with dire consequences.
Before the removal procedure, the woman is examined in the same way as before the insertion of an IUD. The restrictive rules are the same and are followed during the first week after extraction. Changes in the menstrual cycle are noted only if a hormone-containing IUD was used. The cycle should return to normal within six months. Restoration of reproductive function after removal of the IUD occurs within one year. Although you can plan a pregnancy after two months.
Where it all began
The path to the creation of hormonal contraceptives was long and thorny. The first attempts by scientists to find a relationship between the level of reproduction and the function of the corpus luteum began at the end of the 19th century. In 1921, Ludwig Haberlandt, a professor of physiology at the University of Innsbruck (Austria), transplanted the ovaries of a pregnant rabbit into a female rabbit and thereby demonstrated an example of hormonal contraception. It is Ludwig Haberlandt who is considered the father of the hormonal method of preventing unwanted pregnancy.
By 1930, scientists had determined the structure of steroid hormones, isolated them, and even discovered that high doses of androgens, estrogen and progesterone prevented ovulation. It took pharmacologists almost a quarter of a century to come up with the creation of the first hormonal contraceptive. It turned out to be a drug with two active ingredients norethinodrel + mestranol.
Interestingly, the drug was first approved as a treatment for menstrual disorders. Only three years later (in 1960) the American FDA gave the green light to the use of the drug as a contraceptive. And this was just the beginning of a long journey.
Hormonal contraceptives are divided into the following types: