Structure of the TMJ
The temporomandibular joint (TMJ) is a paired joint projected in the area of the front of the ears, located at the place where the skull and lower jaw connect.
The anatomical structural elements of the joint are: the articular head; glenoid cavity; intra-articular disc dividing the joint cavity into the upper and lower floors, the articular capsule and the ligamentous apparatus.
TMJ pathologies include:
- muscular-articular dysfunction of the TMJ, as a result of internal disorders or joint disorders of the ligamentous-muscular apparatus
- arthrosis
- arthritis
- synovitis
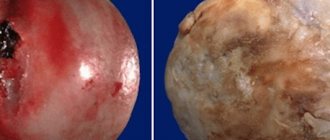
- chondromatosis
- ankylosis
Musculo-articular dysfunction of the TMJ
Muscular-articular dysfunction of the TMJ can cause disturbances in the functioning of such muscle groups as mastication, facial expression, and cervical muscles; or cause intra-articular disturbances in the movement and position of the disc and (or) ligamentous apparatus.
Arthrosis
Degenerative changes in the TMJ are most often described by radiation diagnosticians and manifest themselves in the form of narrowing of the joint space on CT or MRI studies, which is a symptom of other TMJ diseases.
Arthritis
Inflammatory disease of the TMJ, the causes of which can be specific (tuberculosis, syphilis) or nonspecific infectious agents; and autoimmune and connective tissue diseases.
Ankylosis
Acquired or congenital disorder of TMJ mobility. It may be a consequence of hematogenous osteomyelitis as a result of umbilical sepsis, rheumatoid disease, trauma and is characterized by heterotopic bone formation and fusion of articular surfaces.
Temporomandibular joint diseases
Go to:
- Maxillofacial Surgery
Facial pain is one of the most common complaints of patients turning to us for help. At the same time, we observe true facial pain in a third of patients, while secondary facial pain caused by pathology of the ENT organs, ophthalmological problems and dental disorders make up the vast majority of cases. One of the main nosological forms is temporomandibular joint dysfunction syndrome (TMJ) - one of the most difficult and controversial diagnoses in modern medicine. Up to 40% of people experience symptoms of temporomandibular joint disease, but not everyone seeks medical help.
What is temporomandibular joint dysfunction (TMJ)?
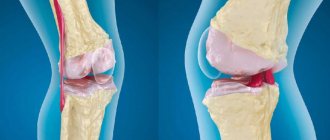
The head of the lower jaw, the articular surface of the temporal bone, the articular disc located between them, the articular capsule, as well as the ligamentous apparatus and masticatory muscles take part in the formation of our joint. The joints are located anterior to the ear canal and work synergistically.
Temporomandibular joint dysfunction means that one of the components of our joint is not functioning properly. This joint is one of the most complex in the human body, it is responsible for the movement of the lower jaw forward, backward and from side to side. Any pathological condition that does not allow this complex system of muscles, ligaments, discs and bones to work properly leads to its dysfunction.
-10% on all MRI and CT scans in the department on Narodnaya Read more
How does the TMJ function?
The temporomandibular joint is a combination joint, representing the functional combination of two anatomically separate joints (left and right). The articulating surfaces of the head of the mandible and the articular surface of the temporal bone are supplemented by a fibrous intra-articular disc located between them, which is attached with its edges to the articular capsule and divides the articular cavity into two sections. Both temporomandibular joints function simultaneously, representing a single combined joint; thanks to the intra-articular disc, movements in three directions are possible in it.
- vertical axis: lowering and raising the lower jaw (opening and closing the mouth) - occurs in the lower part of the joint, between the cartilaginous disc and the head of the lower jaw;
- sagittal axis: displacement of the lower jaw forward and backward - occurs in the upper part of the joint, between the cartilaginous disc and the articular surface of the temporal bone;
- frontal axis: lateral movements (rotation of the lower jaw) during chewing - on one side, the head of the lower jaw together with the cartilaginous disc emerges from the articular fossa onto the tubercle, and on the opposite side, the head of the lower jaw rotates relative to the articular cavity around a vertical axis.
What are the symptoms of temporomandibular joint disorders?
Painful TMJ dysfunction or TMJ pain dysfunction syndrome has many synonyms: Costen's syndrome, myofascial pain syndrome of TMJ dysfunction, TMJ dysfunction, craniomandibular dysfunction syndrome, mandibular dysfunction, musculo-articular dysfunction of the TMJ, etc.
This symptom complex was first described by otolaryngologist J. Costen, who observed it in patients with missing teeth and in people with low occlusion. Painful joint dysfunction is characterized by the following manifestations:
- headache (fronto-temporo-parietal localization), ear pain, as well as pain and pressing sensations behind the eyes;
- “crunching” or “clicking” when opening or closing the mouth;
- pain when yawning and wide open mouth;
- spasm of the chewing muscles;
- displacement of the center line of the jaw;
- malocclusion.
The variety of clinical manifestations of temporomandibular joint dysfunction is determined by the polyetiology (multiple causes) of the pathological processes developing in it, which complicates diagnosis and treatment.
What Causes TMJ Disorders?
In general, TMJ disorders are a multifactorial process. These factors can be divided into two types: problems associated with the masticatory muscles and problems with the joint itself. Muscle problems are the most common type, especially for young people.
Muscle problems can be caused by:
- Muscle hyperactivity. This can happen if you clench your jaw frequently, especially while sleeping, which is quite common.
- Scar changes in the masticatory muscles
- Increased sensitivity to pain. This may be due to stress, or some other process that affects pain sensitivity
- Joint problems can be caused by
- Degenerative-dystrophic changes in the joint
- Inflammation in the joint (arthritis)
- TMJ injury
How are TMJ disorders diagnosed?
The diagnosis is made based on symptoms and additional examination methods.
Possible examinations:
- Blood tests that may be useful to look for signs of inflammation;
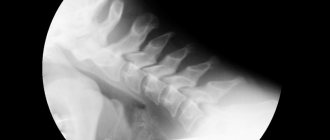
- MRI - this method is used to give a detailed morphological picture of the joint;
- Arthroscopy (using a fiber optic device) to look "inside" the joint);
- Electromyography (EMG) is an objective method for studying the neuromuscular system by recording the electrical potentials of the masticatory muscles, which allows one to assess the functional state of the dental system;
- Densitometry is a method for measuring bone mineral density, that is, the content of calcium, which is its main structural element. The information obtained is subjected to computer processing, the thickness and size of the bones, and their volumetric density are calculated. Such indicators make it possible to judge the resistance of bone tissue to mechanical stress.
What is the treatment for temporomandibular disorders?
Most problems in the mandibular joint can be eliminated using simple procedures, such as painkillers and muscle relaxants, a course of physiotherapy and exercise therapy, and advice on how to relieve the joint, procedures aimed at relaxation and anti-stress therapy. These are the so-called orthopedic methods using mouthguards and bite pads.
In case of more severe disorders in the joint or the ineffectiveness of conservative methods, they resort to injections of botulinum toxin into the masticatory muscles if they are hyperactive and intra-articular administration of steroids.
Arthroscopy is a minimally invasive surgical treatment using endoscopic equipment. A very small percentage of patients may be eligible for open joint surgery. As a rule, these are gross deformations of the joint in the form of ankylosis.
It's great to have all the doctors nearby.
More details
What are the prospects for the treatment of temporomandibular disorders?
Most TMJ disorders improve over time.
Make an appointment with a specialist by phone, online appointment or mobile application.
Treatment
Treatment for TMJ can range from conservative dental and medical treatments to complex surgical procedures. Depending on the diagnosis, treatment may include a short course of anti-inflammatory, painkillers and drugs aimed at muscle relaxation, special mouthguards/plates/splint therapy, consultation with medical specialists on psychological problems and stress.
If non-surgical treatment is unsuccessful or if there is obvious joint damage, surgery may be recommended. Surgery may involve arthroscopy and arthrolavage (a technique identical to orthopedic procedures used to examine and treat large joints such as the knee) or removing damaged tissue and replacing it with implants.
After diagnosing and making the correct diagnosis for problems with the temporomandibular joint, our specialists will provide the appropriate treatment necessary for a particular case.
MRI of the temporomandibular joints in the diagnosis of TMJ diseases
An integral component of dental and, as a result, general health is the normal function of the temporomandibular joints (TMJ). Today, the prevalence of TMJ diseases in the population is quite high.
The most common cause of TMJ dysfunction is internal damage and disruption of the normal anatomical relationships of the articular disc and the mandibular condyle.
Clinically, dysfunction manifests itself as impaired mouth opening, crunching when moving the lower jaw, tension in the muscles of the head and neck, the appearance of “trigger points,” headache (and the pain can be so severe that it is often confused with migraine).
The exact localization of the articular disc is very important in assessing TMJ damage and can be easily determined using MRI.
In this case, the anterior displacement of the articular disc is determined in 34% of healthy volunteers, and the normal position of the articular disc is detected only in 16-23%.
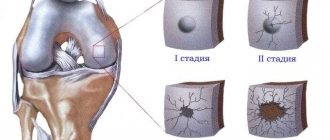
At an early stage, the disc retains its shape. Over time, the damaged disc becomes deformed.
More often, the deformation occurs in the form of thickening of the posterior zone and thinning of the anterior and intermediate zone.
Each study performed must be done in 2 positions - with the mouth closed and open.
Oblique sagittal view with closed mouth. Normal TMJ.
The articular disc is not dislocated; its posterior part is located at 12 o'clock on the condyle dial.
Normal disk mobility
Open mouth position. The condyle has shifted ventrally, to the level of the glenoid fossa. At the same time, the articular disc maintained its normal interposition position, preventing the bone structures from directly contacting each other.
Disc displacements.
There are anterior, anterolateral, anteromedial, lateral, medial and posterior displacements; The most common diagnosis is anterior disc displacement.
Disc dislocations – fixed and intermittent (subluxation).
With a fixed dislocation, the disc is displaced anterior to the condyle in both the open and closed mouth position; with intermittent dislocation (subluxation), the disc is displaced anteriorly only when the mouth is closed. When the mouth is opened, the disc returns to its normal position of interposition between the condyle and the articular tubercle. At the same time, a characteristic click is heard.
Intermittent (reducible) dislocation/subluxation.
A. Closed mouth. Anterior disc displacement. B. The mouth is open. The disc returned to its normal position between the condyle and the temporal bone.
Fixed (irreducible) dislocation.
A. The mouth is closed. Anterior disc displacement. B. The mouth is open. The disc remains displaced.
"Stuck" disk.
"Stuck" disk. PD sag images with the mouth open (A) and mouth closed (B) - the posterior edge of the disc (arrow) remains in the mandibular fossa of the temporal bone. For this reason, mouth opening is greatly limited. The probable cause is the formation of adhesions.
Posterior disc displacement.
Posterior disc displacement (accounts for less than 0.01% of all TMJ pathologies). A. Closed mouth position. The articular disc has shifted dorsally. B. Open mouth position. Return of the articular disc to the level of the mandibular condyle. Jaw movements are very limited in this case.
Synovitis.
In addition to articular disc pathology, there are other causes of temporomandibular joint dysfunction.
A small amount of effusion in the joint cavity.
Osteoarthritis of the TMJ.
Mouth closed. The flattening of the mandibular condyle is determined.
Pathology of retrodiscal tissues.
Both images (different patients) show a tear in the fibers of the dorsal (posterior superior and inferior discotemporal) ligaments.
Traumatic changes.
Bilateral fracture of the condylar processes, hemarthrosis, changes in the pterygoid muscles.
In patients with clinical manifestations of internal disorders of the TMJ, the leading method of radiological examination is functional MRI. The most informative are Pd- and T2*-weighted images in the oblique-sagittal planes.