- home
- Helpful information
- Anti-relapse treatment
- Fatty liver degeneration
Fatty hepatosis is a liver disease in which fat accumulation occurs in the liver tissue (an increase in the amount of lipids).
The disease is often associated with alcohol consumption, but it can also be caused by other reasons. Sign up for a consultation
Classification of hepatosis
Depending on the intensity of changes occurring in the liver, hepatosis is divided into acute and chronic. In the acute course of the process, a sharp and vivid appearance of symptoms is noted, while degenerative changes rapidly progress. Acute hepatosis usually develops as a result of intoxication. Chronic hepatosis usually does not manifest itself in any way; it gradually spreads against the background of obesity, diabetes, alcoholism or other diseases associated with metabolic failure.
The source of the problem may be external and hereditary. In the first case, hepatosis appears as an expected result of uncontrolled use of drugs, an unbalanced diet (non-alcoholic medicinal) and alcohol abuse (alcoholic).
Data
· Alcohol damage occurs due to the toxic effects of alcohol on organ cells.
· The most common damage is fat accumulation. In some cases, cirrhosis and ascites develop.
· Up to a certain point, the damaged liver can recover if you stop drinking alcohol or reduce its amount.
· Cirrhosis is a serious chronic disease that has no cure. But its development can be slowed down by avoiding alcohol consumption and drug therapy.
· Treatment of alcohol-induced liver damage involves first stopping alcohol consumption.
Prerequisites for the development of hepatosis
People with a history of the following diseases need to think about liver health:
- diabetes
- decreased insulin sensitivity
- thyroid disease
- alcoholism
- obesity
- visceral obesity
- disorders of carbohydrate and lipid metabolism
- Cushing's syndrome
- protein deficiency
People at risk include people who have been following a vegetarian and vegan diet for a long time, patients taking a long course of antibiotics, as well as pregnant women.
Clinical picture of hepatosis
The initial stages of the disease are accompanied by mild malaise, which is often not associated with the liver. As the problem worsens, the following symptoms may appear:
- rapid weight loss
- lack of interest in food
- vomiting and nausea
- bright vascular pattern appearing through the skin
- so-called “liver palms”
- change in the tone of the skin and mucous membranes to yellowish, especially noticeable in the color of the sclera
- accumulation of fluid in the peritoneal area
When to ask for help
If you or your family think there is a problem with alcohol, talk to your GP or consult a drug specialist . If you suspect that you have developed liver disease, you should inform your doctor and undergo the necessary examinations.
You need to contact a specialist in the following cases:
· Systematic consumption of alcohol for 1 year ( Alcoholism ).
· General malaise: drowsiness, chronic fatigue.
· Previous liver diseases.
· Presence of dyspeptic syndrome: morning sickness, indigestion, vomiting, change in stool.
· Tremor of the limbs.
· Sudden change in body weight (dystrophy or obesity).
· Enlarged parotid lymph nodes (Dupuytren's contracture).
· Signs of hypogonadism. In men, they manifest themselves as a slight expression of secondary sexual characteristics: testicular atrophy, gynecomastia, female type of hair growth.
· Pain in the hypochondrium, heaviness in the stomach.
Why is hepatosis dangerous?
The most common is fatty hepatosis or steatohepatosis - a degenerative change in organ tissues, which is accompanied by the filling of hepatocytes with fatty deposits. The degeneration of cells is provoked by the fact that the liver ceases to properly perform its functions, which affects the body’s intoxication ability, the production of enzymes, etc. In the future, in the absence of adequate therapeutic measures, fibrosis joins the problem, worsening to cirrhosis and the formation of a malignant tumor.
Fatty hepatosis is diagnosed in patients in whom 10% or more of the total liver volume has undergone changes.
Cells can degenerate either by the small-droplet or large-droplet type. In the first case, steatosis does not affect the viability of hepatocytes, but in the second, the cellular structure suffers and the cells die.
Lipids accumulate in the liver in different ways. When fat is evenly distributed, hepatosis is classified as a diffuse form of the disease. The zonal form is characterized by separate lesions in single areas. If hepatosis is disseminated, then cells throughout the entire tissue mass of the organ undergo changes; in a focal scenario, the disease is localized in a specific lobe.
Causes, risk factors
The main reason for the development of ALD is alcohol abuse, but a direct relationship between the doses of regularly consumed alcoholic beverages and the occurrence of the disease, the degree of its progression and prognosis has not been established1,3. The main risk factors for the development of ALD are:
- Daily long-term consumption of alcohol in toxic doses: more than 30 g of ethanol for men10 (this is 75 g of vodka or 600 ml of beer), and for women - 20 g (about 200 ml of wine) per day1. The amount of alcohol allowed for daily consumption, regarded as a “safe dose,” varies: in European recommendations for the diagnosis and treatment of ALD10, for example, the “safe dose” for women is considered to be 12 g of ethanol per day and 24 g/day for men. The type of drink also influences: there is evidence that among consumers of red wine, the risk of developing alcoholic cirrhosis of the liver is lower than when drinking beer or spirits4. However, you should not take such news as a guide to action. In any case, alcohol is a factor of toxic damage, so you should be careful about drinking alcoholic beverages even in the smallest doses.
- Heredity. Predisposition to the development of alcoholic liver disease is explained by genetically determined differences in the functioning of enzyme systems responsible for neutralizing ethanol1.
- Ethnicity. Insufficient activity of the ethanol metabolizing enzyme occurs in 50% of the Asian population.1
- Overweight or obese. Is an independent risk factor for the development of ALD.1
- Alcohol dependence in people with viral hepatitis (especially B and C) is associated with more pronounced pathological changes in the organ, as well as a higher mortality rate compared to patients who do not suffer from viral hepatitis.1
- Autoimmune processes. Abnormal immune responses can cause further organ damage even after the effects of alcohol have stopped.1
Mechanism of development of ALD
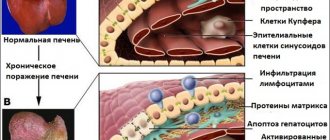
Ethanol in the stomach and liver is oxidized to acetaldehyde, a very reactive compound that damages proteins and disrupts their functions, which in turn interferes with the normal function of liver cells and stimulates lipid peroxidation by free radicals.
This disrupts fat metabolism and the deposition of fat droplets in liver cells. The toxic effect of acetaldehyde also leads to damage to cell membranes and, ultimately, their death.1
Diagnosis and prognosis
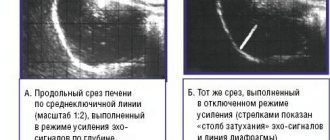
Detecting the problem can be quite difficult, since the symptoms of chronic hepatosis are usually mild. The key diagnostic method is ultrasound examination of the liver; hepatosis is manifested by a change in the echogenicity of the organ and an increase in its size. Additionally, other instrumental studies are prescribed: angiogram, MRI. As well as laboratory tests: blood tests for liver enzymes, which often increase in response to what is happening to the organ. The final diagnosis is made based on the results of studying a tissue sample - a biopsy.
In the first stages, hepatosis is controlled by observing dietary restrictions - this is often enough to restore metabolic processes in tissues and return cells to their functionality. If the disease has already progressed, then diet alone is not enough; comprehensive measures must be taken. In this case, a tactic is used that combines nutrition, drug therapy and a strict regimen, which should become not just a temporary measure, but a way of life.
Fatty liver: symptoms
It happens that fatty liver occurs in an asymptomatic form, or the symptoms of this disease are disguised as other endocrine diseases: thyrotoxicosis, diabetes, diseases of the gastrointestinal tract, etc. In general cases, fatty liver is characterized by symptoms of indigestion, as well as: - general weakness; - dull pain in the right hypochondrium; - heaviness and feeling of pressure in the abdomen; - mild jaundice appears; - when palpating the liver, painful sensations occur. The acute form of fatty liver is manifested by intoxication of the body, jaundice and symptoms of severe dyspepsia. Among other things, the following symptoms are likely to occur: - nausea; - loss of appetite; - flatulence. As a rule, upon diagnosis, an enlarged spleen and an increase in the level of lepidins in the blood are observed.
Principles of nutrition
No matter how much you would like to take a magic pill and restore liver health forever, the key point in its treatment is diet.
The most commonly recommended diet by doctors is diet No. 5, created by Pevzner. As part of the therapeutic menu, it is recommended to choose lean meat, poultry without skin and fat, and low-fat varieties of white fish. Bread should be limited; from this category of products, it is permissible to eat only dried rye or wheat; a strict ban is imposed on any baked goods and baked goods. As an exception, you can treat yourself to dry crackers or biscuits. Dairy products should be replaced with fermented milk, giving preference to low-fat cottage cheese, kefir, and fermented baked milk. All grains should be cooked until fluffy, limit white rice. Despite the obvious benefits of fresh fruits and vegetables, patients with hepatosis need to choose what comes to their table. For example, you will have to give up everything sour, as well as tomatoes, radishes, sorrel, legumes, garlic and onions. Among these products, it is easy to create a meal plan according to personal preferences. You need to strictly monitor not only the quality of food, but also the balance of nutrients. The main limitation concerns the amount of fat.
Drug therapy for hepatosis
Medicines and dietary supplements in the fight for liver health are not the main, but important factor for achieving positive dynamics. Specialists use antioxidants, vitamin complexes, and selenium-based preparations in their treatment regimens. But the main emphasis is on drugs that have hepatoprotective properties. This group of drugs includes a wide range of names; the drugs differ in their principle of action and active substances. Some hepatoprotectors are based on one component, others combine several, the same applies to the effect they provide, in addition to the regeneration of hepatocytes, the drug can additionally improve the movement of bile, relieve inflammation, relieve nausea, and improve appetite.
Hepatoprotectors based on phospholipids - that is, substances related to the cell membranes of the organ. Phospholipids are indicated for long-term course use, only in this case they give a noticeable effect. These drugs include Essentiale, Essliver, Rezalut and Phosphogliv. Undesirable effects include allergies and digestive disorders.
Medicines based on ornithine - Ornithine, Hepa-Merz - are prescribed for the treatment of alcoholic hepatosis; they are contraindicated for pregnant and lactating women.
Some patients experience hepatosis combined with bile stagnation, in which case medications based on ursodeoxychoic acid are effective: Ursoliv, Ursosan, Usordez, Livodex. All of the above remedies ensure proper flow of bile and prevent the formation of stones. This category of medications also requires long-term use.
Another active substance included in hepatoprotectors is ademetionine. In addition to detoxifying the organ, drugs containing it have antidepressant properties, which is why they are prescribed to people whose liver has been damaged as a result of alcoholism. This group includes Heptor and Heptral.
A huge number of hepatoprotective agents are produced based on milk thistle flavonoids. These include Gepabene, Sibiktan, Silimar, etc. Milk thistle shows good results in improving the condition of the liver, restores appetite, but often does not give the desired effect in the treatment of hepatosis of alcoholic etiology.
Another active substance is thioctic acid. Drugs containing it are included in the drug therapy regimen for hepatosis in patients with diabetes mellitus and alcoholism, but it is not recommended for pregnant women. In the assortment of pharmacies you can find Octolipen, Thiogamma, Berlition.
The latest development in the field of stimulating liver regeneration, enhancing its own ability to neutralize poisons and toxins, and improving the permeability of cell membranes are low molecular weight sugars that have affinity for human hepatocytes. The drug Geptrong is a unique innovative development that shows impressive results in the fight against hepatosis. The injection method of administering the drug allows it to achieve its goal in the shortest possible time. The product is as convenient to use as possible - one injection per day and no pills during the day, and the course has a relatively low price. The high bioavailability of Geptrong guarantees the achievement of the desired result after the first few applications. Heptrong can be used during pregnancy, the drug is completely natural, the only possible side effects are individual intolerance.