Macular degeneration of the retina is one of the causes of irreversible loss of central vision in people over 55-60 years of age. In 2007, age-related macular degeneration was responsible for 8.7% of all cases of blindness on the planet. According to the current trend, this number of cases is expected to double by 2021.
The reason for the decline of visual functions is degeneration of the macula - the most significant part of the retina, responsible for the acuity, sharpness and level of central object vision required for visual work or reading text at close range or driving a vehicle, while peripheral vision in patients such as usually does not suffer at all.
Macular degeneration leads to loss of objective vision, a decrease in overall performance and subsequent disability of the patient, which determines the high socio-medical significance of the disease. At the same time, macular degeneration of the retina can provoke both a slow gradual decrease in vision over several years, and rapid, within just a few months, loss of vision, which depends on the form of age-related macular degeneration and the severity of the disease.
What is the essence of age-related retinal degeneration?
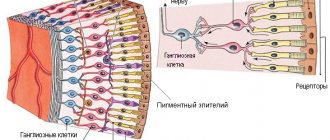
To understand the essence of the pathological process, it is necessary to navigate the structure of the light-sensitive part of the eyeball - the retina. The retina is located at the back of the organ of vision and consists of two main layers. The inner layer is made of special light-sensitive cells - rods and cones. These cells act as receptors - they react to the light signal entering the retina and transmit data about it to the optic nerve. Cones help you see objects in daylight and also form color vision. The rods, in turn, are responsible for twilight vision. The outer layer of retinal cells is made of retinal pigment epithelium, which performs a protective function and is involved in the nutrition of light-sensitive receptors.
| The structure of the retina. Photoreceptors |
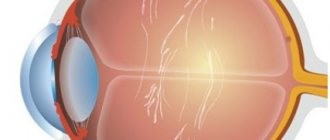
The macula or macula is a small part of the retina that is responsible for central vision. The macular region has the highest density of photoreceptors. In the very center there is a special depression - the central fovea or fovea, made only by cones. It is the central fovea that is the main point responsible for human object vision.
| The structure of the eye. Macula |
Age-related macular degeneration of the retina affects this particular area, which is accompanied by a decrease in central object vision, up to irreversible blindness. Age-related macular degeneration is characterized by the deposition of cellular breakdown products between the retina and the choroid (choroid). This process is also associated simultaneously with morphologically determined hyper- and hypopigmentation of the retina. Such initial changes do not yet cause deterioration and reduction in visual acuity. However, further progression of the disease determines clinically significant changes. There are two forms of age-related macular degeneration of the retina, which will be discussed in detail below.
Diagnosis
Primary diagnosis for macular degeneration consists of taking a medical history and fundoscopy (visual examination of retinal tissue with preliminary expansion using special drops).
Additional diagnostic methods for AMD may include:
- Amsler test (can also be used for self-diagnosis);
- FAG of the retina (fluorescein angiography);
- OCT of the retina (optical coherence tomography);
- ophthalmoscopy.
Dry form of macular degeneration
Atrophic or dry age-related macular degeneration accounts for about 85%-90% of cases of this disease and occurs with equal frequency among male and female patients.
This form of the disease is characterized by the deposition of cellular breakdown products, so-called drusen, between pigment epithelial cells and Bruch's membrane. Bruch's membrane is an acellular formation consisting of 5 layers and acts as a barrier between the retina and the choroid. Nutrients and oxygen necessary for normal functioning diffuse through Bruch's membrane to the pigment epithelium and photosensitive receptors of the retina. Metabolic products, on the contrary, are transported from the retina to the choroid.
With age, Bruch's membrane undergoes significant morphological changes, which include thickening, calcification, and degeneration of collagen and elastin fibers. Incomplete elimination and accumulation of metabolic products of lipid nature also occur. Deposits of metabolic products consisting of lipofuscin are called drusen. Drusen are the earliest indicator of macular degeneration of the retina and come in two varieties - soft and hard.
| Macular degeneration. Dry form |
Hard drusen are small, round deposits with well-defined boundaries. They are often a sign of age-related changes in the retina, but do not cause clinically significant visual impairment. As macular degeneration of the eye progresses, small single deposits accumulate into larger formations - soft drusen.
The appearance of soft confluent drusen is associated with an unfavorable prognosis for maintaining high visual vision. There is a disconnection between the retina and the choroid, which disrupts the nutrition of all cellular layers of the retina, causes degradation of photoreceptors and gradual replacement of damaged retinal cells with scar connective tissue.
Geographic atrophy is the final stage of dry macular degeneration, in which large areas of atrophy and death of the retinal pigment epithelium and proliferation of connective tissue are visualized. Such processes lead to significant loss of central vision, which can progress over years. Slow decay of visual functions and a decrease in central vision significantly reduce the patient’s ability to visually work, but not as pronounced as with the wet form of macular degeneration.
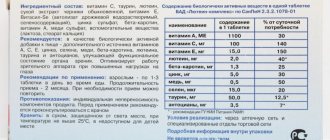
Lutein and zeaxanthin
It is not for nothing that the macula is called the yellow spot; its yellow color is easily explained by the presence of two types of pigment - lutenin and zeaxanthin. These are plant carotenoids, which are found in significant quantities in orange, yellow, and green vegetables. There are many of them in corn, carrots, spinach, cauliflower, etc. This macular pigment is one of the most important factors protecting retinal photoreceptors. Being an effective natural antioxidant and a reliable filter of the blue part of the spectrum, it prevents damage to highly sensitive retinal cells.
As the body ages, the concentration of macular pigment decreases, which can cause damage to the retina and the development of dangerous pathologies, for example, age-related macular degeneration AMD.
Wet macular degeneration
Neovascular or wet age-related degeneration of the macula and posterior pole of the eye is an alternative pathway for the development of a pathological process in which the separation of the retinal pigment epithelium and choroid is accompanied by an increase in the concentration of vascular endothelial growth factor. This biologically active substance stimulates angiogenesis, that is, the ingrowth of newly formed vessels under the retina in the projection of the central macular zone.
Neovascularization processes are accompanied by vasodilation, impaired vascular permeability and migration of endothelial cells. Newly formed vessels, penetrating into the subretinal space, destroy the anatomical barrier in the form of Bruch's membrane between the choroid and the retina and form a kind of vascular network, called the “subretinal neovascular membrane”. The wall of the newly formed vessels is functionally defective, which leads to leakage of fluid, plasma and blood cells under the central zone of the retina and is accompanied by subretinal hemorrhages of varying volumes into the macula.
| Age-related macular degeneration of the retina. Wet form |
The constant presence of blood and fluid under the retina ultimately leads to the separation of Bruch's membrane, pigment epithelium and the photosensitive layer of the retina from each other, with subsequent disruption of the structure and function of photoreceptors, their degenerative degeneration, fibroglial transformation of tissue in the macular zone into a single scar conglomerate. Over time, a specific ridge forms in the area of the macula, surrounded by scar tissue and small hemorrhages.
Clinically, the processes described above are manifested by disturbances in central vision and the appearance of dark spots (scotomas) before the eyes. Thus, choroidal subretinal neovascularization, being a reparative reaction of the body aimed at improving the trophism of the central retina, increasing the supply of oxygen and nutrients to the macula, leads to the progression of the disease and the inevitable loss of objective vision.
The wet form of age-related macular degeneration of the retina often develops in a short time - the disease can greatly impair the patient's quality of life in a few months or even weeks.
Prevention of macular degeneration
If you want to avoid the disease, take timely prevention of macular degeneration of the retina:
- Eat well, don’t go on strict diets;
- take vitamins and antioxidants with lutein and zeaxanthin;
- control blood pressure and cholesterol levels;
- stop smoking. It leads to spasms and decreased elasticity of blood vessels;
- do not overuse tanning;
- wear high-quality sunglasses, as UV radiation actively affects the retina and destroys visual pigment
You should immediately consult an ophthalmologist if you begin to see straight lines with distortion. The disease can develop very quickly, and then the risk of loss of central vision is very high. Take the wet form of age-related macular degeneration especially seriously. It requires constant treatment from a specialist. With timely treatment, you can maintain your vision and high quality of life.
Causes of development of age-related macular degeneration
Until now, scientists have not been able to identify the only reliable cause of age-related macular degeneration of the eyes. However, age-related macular degeneration is believed to have a direct correlation with the age of the patients. Thus, in patients of the middle age group, the disease occurs in only 2% of cases; at the age of 65-75 years, the disease is detected in 20% of patients. And when people reach the 75-year barrier, the risk of developing the disease increases by 35%, that is, age-related macular degeneration of the retina is diagnosed in every third person. That is why, according to most researchers, the main reason for the development of the disease is age.
However, there are a lot of predisposing factors that, when combined with hereditary predisposition, determine the high risks of this pathology. Some of them will be listed below:
- The risk of vision loss associated with macular degeneration in smokers is twice as high as in people without this bad habit.
- Arterial hypertension, various cardiac pathologies, alcohol abuse, obesity, and Alzheimer's disease increase the likelihood of developing degenerative changes in the retina.
- Hereditary predisposition, especially in combination with smoking, should increase suspicion for age-related macular degeneration of the retina.
All these factors cannot directly influence the condition of the retina. However, the biochemical reactions induced by them are the basis of macular degeneration of the eyes.
The retina is thought to be particularly susceptible to oxidative stress due to chronic exposure to visible light and high oxygen concentrations. The discovery of the role of oxidative stress in the development of macular degeneration determined the possibilities of preventive treatment with antioxidants of individuals with an increased risk of age-related macular degeneration of the retina. This issue will be discussed in more detail in the section on therapeutic options.
Causes
The main causes of the onset of macular degeneration are:
- hereditary predisposition to the diagnosis;
- insufficient oxygen saturation of eye tissues;
- unfavorable environmental conditions - sunlight, radiation rays;
- stressful situations.
Risk factors for progression of macular degeneration:
- Age over 60 years.
- Iris of light shades (blue, green, gray, amber).
- Excess weight, low mobility.
- Hypertension and other cardiovascular diseases.
- Tobacco smoking is the most dangerous factor on the list. Smokers are diagnosed with AMD 3 times more often.
Symptoms of age-related macular degeneration
The initial stages of age-related macular degeneration, especially if only one eye is involved in the pathological process, are most often asymptomatic. There are also no pain sensations that could cause discomfort and prompt a person to visit an ophthalmologist. Age-related macular degeneration of the retina has many symptoms that affect the daily life of patients, the main of which are the following:
- Reduction in varying degrees, up to complete loss, of object vision with the formation of a spot or spots of gray or black colors in the central field of vision. Distortion of the image in the form of metamorphopsia - the objects in question have an elongated shape, a larger or smaller size than they actually are, broken straight lines. These symptoms are the most common and characteristic of pathology of the macular zone.
- Cloudy and defective central vision causes problems with reading, writing, driving, watching TV, and recognizing faces.
| Healthy person's vision | Vision of a patient with retinal degeneration |
- Impaired contrast sensitivity. It becomes difficult for patients to distinguish the textures of environmental objects and their changes. For example, such people may not notice small changes under their feet in the form of a drop in the sidewalk or a step. This increases the risk of falls and injury. Difficulties arise in differentiating colors that are similar in color range.
- Poor tolerance to changes in light levels. Difficulties are caused by walking or driving a car at sunset or dawn, as well as moving from a well-lit room to a darker one.
- Need for more lighting. Patients with age-related macular degeneration need brighter light for reading, cooking, and performing daily tasks.
- Impaired perception of distances. People cannot adequately estimate the distance between objects, skipping steps or tripping over a threshold when walking.
Dry macular degeneration, as a rule, is characterized by a slow decrease in object vision, a gradual increase in symptoms and the development of blurred images when viewing objects both near and from afar. Over time, central vision becomes increasingly blurred, and this area increases in size as the disease progresses.
Wet age-related macular degeneration is characterized by a sharp increase in disease symptoms and causes much more rapid vision loss, sometimes even within a few weeks.
Modern methods of diagnosing the disease
The examination always begins with a conversation, clarifying the details of the disease and complaints of patients who are suspected of age-related macular degeneration of the retina. The symptoms presented by the patient are quite characteristic and typical, which allows one to assume the nature of the pathology, which is subsequently confirmed by standard ophthalmological examinations and instrumental diagnostic methods.
- First of all, a fundus examination or fundoscopy is performed. During visual assessment, characteristic drusen are clearly visible in the form of pale yellow dots. In the wet form of the pathology, abnormal choroidal vessels, as well as foci of local hemorrhage, are well differentiated.
| Fundus of the eye with macular degeneration |
- Amsler grid. The Amsler test is the simplest and most functional test for diagnosing the condition of the central visual field, and is often used for self-monitoring. If a patient has macular degeneration, the visible lines appear broken and wavy, and there are gray or dark spots in the field of vision.
| Normal vision | Dry macular degeneration | Wet retinal degeneration |
- Fluorescein angiography is performed if choroidal neovascularization is suspected. Hypofluorescent changes are usually associated with hemorrhages and pigmentary hyperplasia. The causes of hyperfluorescent changes are more numerous and include soft and hard drusen, a network of newly formed vessels, atrophy of the pigment epithelium, and subretinal fibrosis.
| Macular degeneration with massive subretinal hemorrhage |
- Optical coherence tomography is a highly effective non-invasive diagnostic method that allows you to detect the presence of intra- and subretinal fluid, as well as evaluate the effect of the treatment.
| Optical coherence tomography of the macula of a healthy eye |
| Optical coherence tomography for age-related macular degeneration of the retina |
Age-related degeneration of the macula and posterior pole requires constant monitoring in order to timely identify the progression of the disease or the transition of the disease from a dry form to a more aggressive wet one.
Dynamic instrumental observation 2-3 times a year in patients suffering from age-related macular degeneration of the retina can significantly improve the prognosis and promptly stop the irreversible decline in central object vision.
If the patient has a complicated medical history, but in the absence of clinical signs of the disease, control examinations of the fundus and dynamic monitoring of the results of instrumental examination for early detection of hard or soft drusen 1-2 times a year are usually recommended.
Diagnosis of AMD
Macular degeneration is a serious disease that can cause complete blindness. Therefore, at the age of 45 to 50 years, it is recommended to undergo an ophthalmological examination at least once every 2-3 years, and after 60 years - at least once a year. Modern computerized retinal diagnostic methods make it possible to detect the disease at the earliest stage of the dry form of AMD. For this purpose, as a rule, the method of optical coherence tomography (OCT) is used. With its help, a specialist can obtain detailed information about the changes occurring in the tissue structures of the macula.
If symptoms of the disease appear, such as a blurry spot in the center of your vision, you can test for AMD at home. To do this, you will need an Amsler table, which can be easily found on the Internet. This test is intended to identify pathologies of the macula, as well as assess the dynamics of treatment of a previously diagnosed disease of the central part of the retina. The table must be placed at a distance of 30 cm and one eye must be covered with your hand. Then you should focus on the bold dot, which is in the center of the checkered page. If you have AMD, the cells around the focal point will begin to become distorted. Ophthalmologists recommend marking these deformities on a sheet (sketching) and taking them with you to your appointment. This may be useful during the diagnostic process.
Many people are interested in what factors influence the development of AMD. Currently, doctors identify several reasons that contribute to an increased risk of the appearance and aggressive progression of this disease.
Factors influencing the appearance of macular degeneration:
- Sexual characteristic. In women, the risk of developing the disease is 2 times higher;
- Age. VMB is often diagnosed in people over the age of 50;
- Obesity (overweight);
- Smoking;
- Chronic diseases (atherosclerosis, hypertension, diabetes mellitus);
- Negative professional factors (ionizing radiation);
- Bad ecology.
How to treat dry macular degeneration?
Unfortunately, there is no therapeutic intervention that would be able to stop the progression or cure patients with dry macular degeneration of the eyes. Taking into account the theory of oxidative stress, patients with a large number of drusen, pigmentary changes or geographic atrophy are advised to take antioxidants according to various regimens.
The goal of this treatment for age-related macular degeneration of the retina is to neutralize oxygen free radicals that provoke pathological reactions. Dosages and individual dosage regimens are determined by the doctor. The main components of such therapeutic regimens are vitamin C, vitamin E, zinc oxide, lutein, beta-carotene, vitamin A, copper oxide. Patients are also usually advised to stop smoking and eat foods rich in polyunsaturated omega-3 fatty acids.
Treatment of macular degeneration
If you have been given this unpleasant diagnosis, do not rush to be upset. Treatment tactics depend on the form of the disease. For the dry form, the doctor uses conservative methods, which include:
- injections of drugs to improve retinal saturation;
- taking antioxidants, nootropics;
- physiotherapy.
If a doctor has identified a wet form of the pathology, he usually prescribes laser beam exposure to newly formed vessels or dehydration therapy. There are several effective VEGF inhibitor drugs that are used to treat macular degeneration of the retina. These include Macugen, Lucentis, Eylea, Avastin. All of these drugs help stabilize vision and prevent vision loss. After surgery, there may be an increased risk of eye infection and eye irritation and pain. Sometimes retinal detachment occurs, vision temporarily becomes blurred, and intraocular pressure increases.
Macular degeneration - wet form: treatment of pathology
Treatment of the wet form of age-related macular degeneration of the retina is aimed at inhibiting the processes of subretinal neovascularization, preventing and treating complications.
Angiogenesis inhibitors
Inhibition of angiogenesis is currently one of the most effective treatments for wet macular degeneration of the retina. The basis of the therapeutic effect is the intravitreal administration of antiangiogenic drugs, that is, drugs that block vascular growth factor and, accordingly, suppress the process of subretinal neovascularization.
| Treatment of macular degeneration with angiogenesis inhibitors |
The most commonly used in practice are Pegaptanib (Macugen), Bevacizumab (Avastin), Ranibizumab (Lucentis) and Aflibercept (Aylia). The use of drugs in this group for age-related macular degeneration helps stop the growth of pathological blood vessels, thereby reducing the risk of vision loss. Over the past decade, numerous clinical studies have confirmed their high effectiveness in patients diagnosed with wet age-related macular degeneration.
Treatment with angiogenesis inhibitors allowed them not only to stabilize, but also to improve visual function. Significant disadvantages of this type of treatment are the invasive nature of the intervention, a decrease in the effect of treatment if it is abandoned, and the significant cost of treatment, especially taking into account the need for a course of intravitreal injections to achieve a clinically significant result.
Laser coagulation for macular and posterior pole degeneration
Laser treatment methods are indicated for the presence of subretinal neovascular membrane in patients who have been diagnosed with age-related macular degeneration. Treatment consists of laser coagulation of the neovascular membrane located extrafoveolar to the central fovea of the retina.
| Laser treatment for retinal degeneration |
The purpose of laser coagulation is to stop blood flow in newly formed vessels due to the coagulating effect of laser radiation on their wall. The main disadvantage of this treatment for macular degeneration is the presence of an undesirable damaging effect on the photoreceptors of the retina, which significantly limits the indications for the use of laser treatment, both in terms of the localization of the pathological process and the magnitude of object vision.
Photodynamic therapy
When treating the wet form of age-related macular degeneration of the retina, photodynamic therapy is a worthy alternative to laser treatment. Often, photodynamic therapy is an even more effective way to combat the phenomena of wet degeneration of the macula and posterior pole of the eye compared to the above treatment methods.
The clinical result of treatment is due to the laser effect on newly formed vessels and blocking blood flow in them. The light-sensitive drug “Visudin” used in photodynamic therapy accumulates only in areas of neovascularization. Laser irradiation of "Visudin" accumulated in newly formed vessels leads to the formation of a blood clot in them and obliteration of the lumen, as a result of which blood flow in the neovascular vascular network completely stops.
| Photodynamic therapy for macular degeneration |
The undoubted advantage of photodynamic therapy compared to laser treatment is its exclusive effect only on newly formed vessels without damaging the photoreceptor cells of the retina. It is also necessary to note the possibility of combined use of photodynamic therapy in combination with other methods of treating the wet form of age-related macular degeneration of the retina.
Transpupillary thermotherapy
Transpupillary thermotherapy is one of the safe and effective methods of treating age-related macular degeneration of the retina, which has proven itself in the wet form of macular degeneration with the presence of hidden choroidal neovascularization of any type, including subfoveal localization.
Carrying out transpupillary thermotherapy in the macular region of the retina does not lead to coagulation and photochemical damage to photoreceptor cells, since the main objective of the method is to reduce blood flow in the choroid as a result of irradiation with an infrared laser.
Transpupillary thermotherapy, as a rule, is an alternative to photodynamic therapy when there is no positive therapeutic effect of the latter.
Review of retinal treatment at the Excimer Clinic
Sh. Svetlana, Moscow
Thank you for the prompt and high-quality work. Today we did a comprehensive examination and strengthened the retinas of both eyes. Many thanks to the doctor, a man of his profession (unfortunately I forgot to ask his last name) received me in room 307a. I was left with a pleasant impression;) After a while I will undergo vision correction. Thanks to all!
A. Alexander Isakovich, Moscow
I, Alexander Isakovich Alterman, am simply shocked by the attention and sensitivity of Dr. Kalashi Zurab Yusupovich and Irina Srgeevna Yusupova. I am a disabled person of the 2nd group, a labor veteran born in 1938.
Pilipchak Snezhana, Moscow
On Saturday (May 16, 2015) I had laser coagulation (strengthening the retina), done by Olga Aleksandrovna Plyukhova!! I express my deep gratitude to her for her HUMANITY, for her understanding and patience... it was a bit painful for me, but if you compare the coagulation 9 years ago , Olga Alexandrovna has golden hands!!!! Next Saturday, May 23, there will be laser correction, I'm terribly afraid)) And about the clinic. Before the consultation in Excimer, I had a consultation at the Moscow Eye Clinic (Moscow, m. Semenovskaya), earth and sky!!! At the MGK they did not find a retinal dehiscence during the examination and immediately recommended me to do a correction (and what would have happened to me???!!!!) I wonder!! Yes, Excimer is several times more expensive, but I’m not buying sausage, I’m buying good eyesight!! You can't regret it!!! Thanks everyone! I don’t understand where the bad reviews come from, everyone is so nice, the equipment is at the highest level, as is the qualifications of the nurses and doctors!
All reviews on the topic