Mark Anatolyevich, what could be the reason for liver enlargement?
- In general, liver enlargement itself is just a symptom of the disease. It is necessary to first find out the cause of the disease, and then eliminate it.
Diseases that contribute to liver enlargement are cirrhosis and fatty hepatosis (fatty liver).
These diseases are chronic and are caused by various factors, including malnutrition, alcohol abuse, or infectious viral hepatitis.
What is the treatment?
— One of the most common causes of liver disease is viral hepatitis. In this case, antiviral therapy is prescribed.
If it is toxic, alcoholic hepatitis, then you need abstinence from alcohol, medication support and diet.
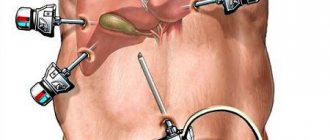
In case of fatty hepatosis associated with excess body weight, measures aimed at reducing excess body weight, diet, drug treatment, and surgical intervention if necessary are prescribed.
In the case of cirrhosis, that is, more severe liver damage, treatment is more difficult, but it is possible. First of all, therapy is aimed at eliminating the causes of cirrhosis.
The next step will be treatment with various medications that allow the liver to function more optimally. Well, the last resort treatment for cirrhosis is liver transplantation.
Treatment of NAFLD, fatty hepatosis
Currently, there is no standard treatment for NAFLD, so the main goal is to improve the biochemical parameters characterizing cytolysis (destruction of liver cells) and inflammation, slowing down and blocking fibrosis.
In any case, treatment begins with lifestyle changes, which means both a change in diet and an increase in physical activity.
Physical exercise increases sensitivity to insulin, helps reduce fatty tissue in internal organs, and reduces the level of liver steatosis.
To achieve these goals, 3-4 sessions of aerobic exercise per week are considered sufficient. It has been proven that a decrease in body weight by 8-10% is accompanied by an improvement in the histological picture of NAFLD. The most physiological is considered to be a decrease in body weight by 500–1000 g per week, which is accompanied by positive dynamics of clinical and laboratory parameters, a decrease in insulin resistance and the degree of liver steatosis. Losing weight too quickly leads to worsening of the disease.
Drug treatments as a standard include insulin sensitizers (drugs that increase tissue sensitivity to insulin), hepatoprotectors and antioxidants. It is important to correct metabolic disorders by overcoming insulin resistance using insulin sensitizers (metformin). In addition, the use of ursosan is indicated to normalize metabolic disorders and as a hepatoprotector to improve the histological picture of the liver.
up
Are there any measures to prevent liver disease?
— Quitting the harmful use of alcohol is one of the most important and effective measures in the fight against liver diseases.
Secondly, this is a diet that should not contain too much fat and easily digestible carbohydrates.
You need to control your body weight and prevent it from growing beyond the norm.
Prevention will also include protection with a condom during sexual intercourse, because hepatitis B and C are also transmitted through sexual contact.
It is necessary to stop using drugs, which are associated with a very high risk of contracting viral hepatitis, since blood is another route of transmission.
In addition, there is a vaccine against hepatitis B, which I recommend for everyone.
Who is at risk of developing fatty liver disease?
NAFLD is a multifactorial disease resulting from exposure to a number of risk factors:
- abdominal obesity (waist circumference more than 94 cm in men and 80 cm in women);
- an increase in the level of triglycerides in the blood more than 1.7 mmol/l, cholesterol and a decrease in high-density lipoproteins;
- increased blood pressure more than 130/85 mm Hg;
- impaired glucose tolerance, prolonged hyperglycemia (type 2 diabetes mellitus);
- insulin resistance.
up
What cases from practice related to liver disease do you remember?
— Severe liver damage occurs with viral hepatitis, when a person for a long time did not know that he had a virus, for example, hepatitis C. This hepatitis can be asymptomatic for many years, ultimately leading to cirrhosis of the liver.
That is, a person lived a normal life and suddenly he began to develop symptoms of cirrhosis. Upon further examination, it turned out that the patient’s liver functions were impaired, the disease was already at a serious stage, and the person was on his way to the operating table for a transplant. We have to fight such cirrhosis, and we are talking about survival, not about cure.
Hepatomegaly
Symptoms of liver enlargement are determined by the underlying disease. Moderate hepatomegaly, which develops during acute viral infections and malnutrition in children, may not manifest itself in any way. When the liver reaches a significant size, there may be discomfort in the right hypochondrium, painful sensations that increase with movement. Skin itching, rashes, dyspeptic complaints (nausea, stool problems, flatulence), and bad breath are also typical.
In the case of hepatomegaly against the background of viral hepatitis, compaction of the liver parenchyma is determined, which is easily detected even by palpation. An enlarged liver is accompanied by yellowness of the sclera and skin, and symptoms of intoxication. With timely effective treatment, the syndrome can regress. Hepatomegaly in liver cirrhosis occurs due to damage to hepatocytes and the formation of connective tissue in their place. Characterized by significant compaction of the organ, constant pain in the right hypochondrium, sallow skin tone, and a tendency to bleed.
Liver enlargement due to primary neoplastic lesions occurs quite rarely, with the leading symptoms being: hepatosplenomegaly, pain, dyspeptic disorders, jaundice, edema and ascites. With secondary (metastatic) lesions, the symptoms of hepatomegaly are usually less pronounced than the signs of primary tumor growth. In the case of benign liver tumors, organ enlargement is usually the first and leading sign. When the formation reaches a significant size, an asymmetrical enlargement of the abdomen and signs of compression of neighboring organs are possible.
A feature of hepatomegaly with degenerative changes (fatty liver disease) is scanty symptoms and the rare development of severe damage. Typically, this disease is a diagnostic finding when a patient presents for other reasons. With amyloidosis, the liver can reach significant sizes, its structure is dense, the edge is smooth, and there is no pain on palpation.
Hepatomegaly in heart disease develops in the case of right ventricular failure; the syndrome progresses rapidly, which leads to stretching of the organ capsule and severe pain. The size of the liver is variable and decreases with successful treatment of the underlying disease.
In the case of toxic damage to hepatocytes, liver enlargement may be the only sign; less often it is combined with itching, jaundice of the sclera and skin, and moderate changes in laboratory parameters. In case of traumatic damage to the liver tissue, hepatomegaly against the background of the patient’s severe general condition is accompanied by signs of intra-abdominal bleeding and hemorrhagic shock. Arterial hypotension and tachycardia, hypoxia progress; On palpation the liver is sharply painful.
Why does the liver enlarge?
Abnormal enlargement of the largest gland in our body can occur for various reasons. This is the result of some disturbances in the body:
- liver diseases (hepatitis of various natures). First of all, swelling of the organ occurs, after which inflammation develops. If the pathogenic factor is defeated, the original size of the liver is restored, but voids in the place of dead hepatocytes may be replaced by fibrous tissue. This process leads to re-enlargement of the organ;
- metabolic disorders (hemochromatosis, etc.);
- fatty liver;
- blockage of the hepatic veins;
- cancer or other neoplasms.
An increase may occur for no apparent reason. In such cases, a comprehensive examination is indicated, which is based on laboratory and hardware techniques. It is important to find out the root cause of the abnormality in order to treat the original disease.
A case from the practice of an expert on the website Pokhmelye.rf, gastroenterologist Daniela Purgina.
A mother and her 15-year-old son came to the appointment. An abdominal ultrasound revealed hepatomegaly. All possible examinations were carried out to look for liver diseases, but no pathology was identified. It turned out that the ultrasound diagnostic doctor did not take into account the fact that the boy at 15 years old was much taller and larger than his peers. She compared the size of his liver with the average size that is typical for childhood and adolescence - and according to these data, the boy’s liver was larger than normal. However, when we compared its size with the normal size of an adult male liver, all parameters turned out to be normal. That is why, when assessing the size of an organ, it is necessary to pay attention to the constitutional characteristics of the patient.
CAUSES OF HEPATOMEGALY, RISK FACTORS
The cause of the development (etiotropic factor, impetus for the occurrence) of hepatomegaly can be a variety of diseases. In clinical practice, hepatologists (the so-called specialists whose profile is focused on the management of patients with a diseased liver), as a rule, note hepatomegaly caused by the following pathologies:
- Oncological diseases of the liver - both benign and malignant. Moreover, the enlargement of the liver will most likely be uneven;
- Hepatitis of a very different nature - viral, toxic, autoimmune, alcoholic;
- Polycystic disease;
- Parasitic diseases, for example - echinococcosis (echinococcus is a worm that, when it enters the liver, forms a large cavity filled with a toxic liquid);
- Chronic infectious diseases accompanied by liver damage;
- Severe intoxication, in which the effect of toxic substances extends to the entire body;
- Liver cirrhosis (this disease in the early stages of development leads to hepatomegaly, and in the terminal stage of cirrhosis, on the contrary, the liver decreases in size).
Metabolic disorders in the body and various cardiovascular diseases can also provoke the occurrence of hepatomegaly (for example, with chronic cardiovascular failure of the 2nd stage, stagnation in the pulmonary circulation is formed, the outflow of blood from the liver is disrupted, as a result of which its size increases).
Can hepatomegaly develop in only one lobe of the liver?
The liver consists of two lobes, each with its own innervation, blood supply, and bile ducts (central artery, vein, bile duct). Isolated hepatomegaly of the right lobe of the liver is observed more often than the left. Functionally, the right lobe is loaded more, performing 60% of the organ’s work, so any violations primarily affect it.
The left lobe is rarely affected; it is located closer to the pancreas; therefore, pancreatic disorders can cause an increase in the lobe
The examination usually reveals damage to the gallbladder and ducts, and the spleen.
With uneven enlargement of the organ, they speak of partial hepatomegaly. The lower edge of the liver rarely changes, so ultrasound is necessary for detection. A characteristic echo sign is a change in the homogeneity of the tissue structure. Usually found in tumors, cysts, and abscesses.
Possible complications
Hepatomegaly in itself is not so dangerous. The consequences of chronic liver diseases, which are reflected in hepatomegaly, are dangerous.
One of the most undesirable outcomes of liver disease is cirrhosis. There is a slow destruction of hepatocytes (working liver cells). Empty places where cells have died are overgrown with connective tissue scars. Connective tissue cannot perform the same functions because it is made up of other cells. Due to cell death, the liver ceases to efficiently cope with its functions. Because of this, cirrhosis develops.
Results of treatment of fatty hepatosis
Patient review:
» Dear Bella Leonidovna! Dear Nelly Nikolaevna Tsurikova, Mushinskaya Kira Vladimirovna, girls at the reception, ultrasound diagnostic doctor, thank you all so much for organizing the treatment of my illness. You guys work wonders as a team! High-level professionals and people with a capital “P!” I am grateful to fate that I found your clinic, which really saved my life and changed it 180 degrees. Thanks to your efforts, qualifications and attention, I have become a completely healthy person. I lost 23.5 kg in 9 months, my liver has become a real factory that now works perfectly!
In general, I wish your team all the best. Do not stop! You really do a great job for people, help overcome serious illnesses.
On the eve of the New Year 2021, I would like to wish you health, family joys and love too! with best wishes, your patient from Kazan" >>> - Rustem 12/05/2018
Diagnostics
To detect a change in the shape of the liver, a competent specialist only needs to perform percussion or palpation. Instrumental diagnosis is carried out in a hospital and usually begins with an ultrasound of the internal organs.
To establish the real cause of hepatomegaly, several additional tests need to be performed.
Differential diagnostic tests will help confirm or exclude the viral nature of the pathology of internal organs. Patient diagnosis consists of the following procedures:
- medical history collection (hemodialysis, results of blood transfusions, epidemiological nature of organ tissue damage);
- prescription of PCR (helps detect specific immunoglobulins);
- determination of aminotransferase activity;
- puncture biopsy (checking histological activity).
To exclude the autoimmune nature of the disease, it is necessary to analyze circulating autoantibodies. Lesions of this type are typical for women after menopause. The pathology causes pain in the joints, and in some cases glomerulonephritis is detected.
Cirrhotic etiology makes it possible to identify liver damage caused by excessive alcohol consumption. They are characterized by a high amount of gamma globulins and a low content of prothrombins in the serum. Ultrasound of the abdomen can reveal changes in the liver parenchyma and its heterogeneous structure.
Pathologies of the vascular system (as a possible cause of hepatomegaly) are detected using Doppler ultrasound. The following studies can also be additionally carried out: radioisotope scanning, lower cavagraphy and puncture biopsy. To exclude the possibility of neoplasms, it is necessary to perform MSCT of internal organs.
How is an enlarged liver and spleen combined?
An enlarged spleen (splenomegaly) may accompany hepatomegaly. It has been noticed that these two signs of pathology support each other. A simultaneous increase is expressed in hepatolienal syndrome. It is more typical for children, since it is aggravated by the anatomy and physiology of the growing organism.
It is provoked by hereditary diseases, infections, congenital anomalies. The syndrome is observed:
- for vascular diseases of the arteries and veins of the liver, spleen (vasculitis, thrombosis);
- chronic focal and diffuse liver pathology;
- hemochromatosis;
- liver amyloidosis;
- Gaucher's disease;
- hepatocerebral dystrophy.
Chronic parasitic and infectious diseases always, in addition to the liver, affect the spleen (intestinal tuberculosis, alveococcosis, malaria, infectious mononucleosis). Both organs are significantly enlarged with pathology of lymphoid tissue and blood (leukemia, lymphogranulomatosis, hemolytic anemia). Heart disease is less likely to promote spleen growth.
The main task of diagnosis is to identify the common cause that caused hepatomegaly and splenomegaly.
Organs have a pronounced functional connection