Hypertension (essential or primary hypertension) is a chronic disease associated with a long-term and persistent increase in blood pressure (BP).
There are two forms of hypertension (hypertension): primary and secondary. Approximately 90-95% of patients with hypertension have the primary form. Unlike secondary hypertension, primary hypertension does not have a clearly defined known cause. Therefore, its diagnosis is made after ruling out known causes, which include what is called secondary hypertension. For example, blood pressure may increase symptomatically with kidney disease, and so on.
Blood pressure: Blood pressure resulting from the work of the heart, which pumps blood into the vascular system, and vascular resistance.
Blood pressure readings are usually given as two numbers: for example, 120 over 80 (written as 120/80 mmHg).
The top number is called systolic blood pressure (the higher pressure and the first number recorded) - this is the pressure that blood puts on the walls of the artery when the heart contracts to pump it to peripheral organs and tissues. The bottom number is diastolic blood pressure (the lower pressure and the second number recorded) - this is the residual pressure exerted on the arteries when the heart relaxes between beats.
Normal blood pressure is a relative value, which depends on age, physical activity, psychological state, and even on the use of various medications.
Hypertension occurs when the body's smaller blood vessels (arterioles) narrow, causing the blood to put undue pressure on the vessel walls and causing the heart to work harder to maintain the pressure. In this case, blood pressure reaches or exceeds 140/90 mm Hg.
Diastolic blood pressure is more common in people under 50 years of age. As we age, systolic hypertension becomes a more serious problem. At least a quarter of the adult population (and more than half of those over 60) have high blood pressure.
Causes and risk factors
Despite many years of active research, there is no unifying hypothesis to account for the pathogenesis (mechanism of occurrence) of hypertension. In chronic long-standing hypertension, blood volume and cardiac output are often normal, so hypertension is maintained by increased systemic vascular resistance rather than increased cardiac output. There is also evidence of increased vascular tone. In addition, disturbances in the nervous and endocrine regulation of blood pressure play a role in the development of the disease.
Many factors can affect blood pressure, including:
- Genetic, which play an important role in the occurrence of hypertension.
- How much water and salt is in your body.
- The condition of your kidneys, nervous system and blood vessels.
- Levels of various body hormones.
- Age. Blood pressure gets higher as you get older. This is because blood vessels become stiffer as a person ages.
You are at increased risk of hypertension if you:
- Are you obese?
- Frequently experience stress or anxiety;
- Drinking too much alcohol;
- Consume too much salt;
- Have a family history of the disease:
- Diabetic;
- Smoke;
- You lead a sedentary lifestyle;
- You are experiencing stress.
Opinion of a practicing doctor
A.Yu. Shishonin, a general practitioner with many years of experience, often has to answer the question of how hypertension and hypertension differ from each other. So, he notes that these are just different names for the same condition. Also, both of these names are incorrect. In his opinion, these conditions should be called hypertensive syndrome. Why?
The fact is that hypertensive syndrome is a condition that occurs due to the fact that something else is wrong in the body, that is, there are additional problems. A rise in pressure never occurs on its own. There are reasons for everything. In 5% of cases, hypertensive syndrome is observed in patients with tumors in the glands of the endocrine system (adrenal glands, pituitary gland, thyroid gland, etc.).
It should also be noted that these conditions are easily diagnosed in the early stages in any modernly equipped clinic. In the remaining 95% of cases, high blood pressure in people is associated with complicated osteochondrosis. These are the main factors that provoke the development of hypertensive syndrome. You need to understand that a person’s blood pressure cannot rise on its own.
Note.
More than 90% of recorded hypertension occurs with high blood pressure. In other cases, hypertension (in the early stages of pathogenesis) occurs with normal pressure.
Classification of hypertension
There is no single classification, but the one recommended by WHO is most often used. Hypertension, depending on the degree of increase in pressure, is divided into three stages:
Stage 1 hypertension. Soft or borderline stage. The pressure is 140/90 mm Hg. or higher.
Stage 2 hypertension. Moderate stage. The pressure is 160/100 mmHg. or higher.
Hypertension stage 3. Severe form of hypertension. Clinical systolic blood pressure is 180 mmHg. or higher, and diastolic is 110 mm Hg. or higher.
The disease is also divided into three stages, depending on the degree of development:
Stage 1: slight increase in blood pressure. There are no complaints, the functioning of the cardiovascular system is not impaired.
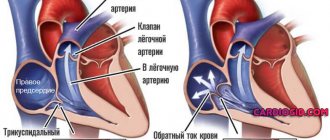
Stage 2: constant increase in blood pressure and associated enlargement of the left ventricle of the heart.
Stage 3: increased blood pressure affects the functioning of the heart, brain and kidneys.
general information
Hypertension is a pathological condition that affects the functioning of all organs and systems in the body. It is quite problematic to completely get rid of the signs of this disease. The etiology of the disease is mainly associated with impaired fat metabolism, as well as changes associated with the aging of the body.
Most often, hypertension is observed in people over 50. The main factors that provoke the development of pathology include the following:
- bad habits (alcohol, drugs, nicotine);
- excessive addiction to caffeine;
- lack of physical activity;
- poor nutrition.
Interesting. The classic features of hypertensive patients include: hyperirritability, short temper, increased emotionality. In residents of large cities and modern megalopolises, hypertension is diagnosed four times more often than in people who live in small cities, towns and villages.
Against the background of hypertension, signs of other diseases are often observed:
- thyroid pathology;
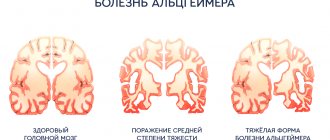
- encephalopathy;
- acute renal failure;
- cerebrovascular dysfunction.
Hypertension is often recorded in pregnant women, as well as in those patients who take hormonal contraceptives. In this case, high blood pressure occurs against the background of other pathological changes that are not related to the functioning of the cardiovascular system.
You can get more information about this and many other aspects of health related to blood pressure, osteochondrosis, atherosclerosis, ask your questions to Dr. Shishonin and just chat by joining our community - the Club of Former Hypertensive Patients
.
Course of hypertension
The risk associated with increased blood pressure is continuous, with each 2-3 mmHg increase in systolic blood pressure. Art.
Hypertension increases the risk of mortality from coronary heart disease by 7% and the risk of mortality from stroke by 10%. The most common immediate cause of death associated with hypertension is heart disease, but death from kidney failure is also common.
Complications arise directly from increased blood pressure (cerebral hemorrhage, retinopathy, left ventricular hypertrophy, congestive heart failure, arterial aneurysm and vascular rupture), from atherosclerosis (increased coronary, cerebral and renal vascular resistance), as well as from decreased blood flow and ischemia ( myocardial infarction, cerebral thrombosis, infarction and renal nephrosclerosis).
If your blood pressure is not well controlled, you are at risk of:
- Bleeding from the aorta, the largest blood vessel,
- Chronic kidney disease,
- Heart attack or heart failure,
- Poor blood supply to the legs,
- Vision problems
- Stroke,
- Disturbance of cerebral blood supply.
Causes
In approximately 90% of cases, the cause of a stable increase in blood pressure is hypertension. This diagnosis is made to the patient when no other diseases accompanied by hypertension are found during the examination. Among the latest:
- kidney pathologies – pyelonephritis, glomerulonephritis, polycystic disease, diabetic nephropathy, renal artery stenosis;
- endocrine disorders - neoplasms of the adrenal glands, pancreas or pituitary gland, hyperfunction of the thyroid gland, Cushing's disease or syndrome, pheochromocytoma;
- obstructive sleep apnea syndrome;
- valve defects or atherosclerotic lesions of the aorta.
Regular use of some medications can also cause high blood pressure.
These include oral contraceptives, non-steroidal anti-inflammatory drugs, amphetamines, corticosteroids, drugs containing erythropoietin, cyclosporine, cocaine. The likelihood of developing cardiovascular diseases, including hypertension, is closely related to the following risk factors:
- unhealthy diet, including excess amounts of table salt, saturated fats and trans fats, lack of leafy greens, vegetables and fruits in the diet;
- obesity;
- pathologies of the heart and blood vessels in close relatives;
- age over 65 years;
- sedentary lifestyle;
- chronic stress;
- bad habits – smoking, excessive alcohol consumption.
Treatment of hypertension at the Innovative Vascular Center
Our clinics employ experienced cardiologists who can accurately determine the causes of high blood pressure and prescribe therapy appropriate to the causes and stage of the disease.
In case of hypertension, we always conduct a thorough diagnostic search, identifying all possible causes of secondary hypertension, especially those related to vascular damage (vasorenal hypertension, increased blood pressure due to narrowing of the carotid arteries, in the presence of adrenal tumors).
At the Innovative Vascular Center, it is possible to correct the causes of arterial hypertension using endovascular methods (stenting of the renal arteries, radiofrequency denervation of the renal arteries).
What causes arterial hypertension
WHO classifies hypertension as a psychosomatic disease, that is, its occurrence is based on psychogenic factors. The biggest culprit in raising blood pressure is the stress hormone cortisol. It is secreted by the adrenal glands in stressful situations. Its main task is to help the body cope with the danger that has arisen, even if it is fictitious. As a result, the heart rate increases, which helps blood move through the vessels faster. If a person is constantly under stress, this leads to a stable increase in blood pressure.
Other causes of hypertension:
- heredity;
- excess weight;
- inactive lifestyle;
- excessive addiction to alcohol;
- taking certain medications, such as hormonal contraceptives;
- smoking
Arterial hypertension does not always act as an independent disease. Sometimes high blood pressure can be a symptom of another medical condition. This condition is called secondary hypertension. Her reasons:
- kidney disease, including injury and kidney infection;
- lead poisoning;
- endocrine diseases;
- congenital anomalies of the vascular system;
- damage or malignant neoplasms of the brain;
- atherosclerosis.
Only a doctor can determine the exact cause after examination and passing the necessary tests.
The term “hypertension” or “essential hypertension” means an increase in blood pressure from unknown causes. According to the latest recommendations of WHO and the International Society of Hypertension (1999), several levels of blood pressure are distinguished
Classification of arterial hypertension by blood pressure level (mm Hg)
| Categories | SBP, mmHg | DBP, mm Hg. |
| Optimal | <120 | <80 |
| Normal | <130 | <85 |
| High normal | 130-139 | 85-89 |
| Hypertension: 1st degree (mild hypertension) | 140-159 | 90-99 |
| Subgroup: borderline | 140-149 | 90-94 |
| 2nd degree (moderate hypertension) | 160-179 | 100-109 |
| 3rd degree (severe hypertension) | ≥180 | ≥110 |
| Isolated systolic hypertension | ≥140 | <90 |
In accordance with this classification, arterial hypertension is considered to be an increase in SBP to 140 mmHg. and higher or DBP up to 90 mm Hg. and higher, if such an increase is stable, that is, confirmed by repeated blood pressure measurements (at least 2-3 times on different days for 3-4 weeks).
Clinical picture
In the initial stages of the disease, the patient begins to complain of the following neurotic disorders: episodes of headache (it is often localized in the back of the head or forehead and intensifies when moving or trying to bend down); dizziness; intolerance to bright light and loud sound for headaches; feeling of heaviness in the head and pulsation in the temples; noise in ears; lethargy; nausea; palpitations and tachycardia; sleep disorders; fast fatiguability; paresthesia and painful tingling in the fingers, which may be accompanied by pallor and complete loss of sensation in one of the fingers; intermittent claudication; pseudorheumatic muscle pain; coldness in the legs.
With the progression of the disease and a persistent increase in blood pressure to 140-160/90-95 mm. Hg Art. The patient experiences: pain in the chest area; dull pain in the heart; shortness of breath when walking fast, climbing stairs, running and increasing physical activity; chill-like tremor; nausea and vomiting; feeling of a veil and flickering of flies before the eyes; nosebleeds; sweating; facial redness; puffiness of the eyelids; swelling of the limbs and face.
Diagnostic scheme for arterial hypertension
Mandatory studies: medical history, complaints; mandatory examination; measuring blood pressure in the arms and legs; blood: complete blood count, creatinine, sugar, cholesterol, Na, K; urine: general urine analysis, tests according to Zimnitsky, Nechiporenko; ECG; X-ray studies of OKG; ocular fundus.
Additional studies (according to indications): ultrasound of the kidneys and adrenal glands, echocardiography, triglycerides and HDL cholesterol, uric acid levels, radioisotope studies of the kidneys, excretory urography, angiography of the renal vessels, computed tomography or MR tomography of the brain, kidney biopsy with histology, urine: adrenaline, norepinephrine, 17-OX, vanillylmandelic acid, aldosterone
Risk factors for cardiovascular diseases:
I. Main risk factors
- Age (for men over 55 years old, for women over 65 years old)
- Smoking
- Total cholesterol > 6.5 mmol/L (250 mg/dL)
- Family history of early cardiovascular disease
II. Other risk factors that worsen prognosis
- Reducing HDL cholesterol
- Increased LDL cholesterol
- Microalbuminuria in diabetes mellitus
- Impaired glucose tolerance
- OBESITY
- Sedentary lifestyle
- Increased fibrinogen
- Belonging to a high-risk socioeconomic group
- Belonging to a high-risk ethnic group
- Belonging to a high-risk geographic group
Treatment of hypertension
Treatment of hypertension begins with lifestyle modification. Regularly perform dynamic and physical exercises, relaxation exercises, and carry out psycho-emotional relief.
Drug treatment
Drug treatment is necessary for all patients with moderate hypertension (BP more than 160/90 mm Hg, as well as patients with mild hypertension for whom drug treatment was insufficient or there was a risk of complications). On the basis of the therapeutic department of the inpatient unit No. 2 of the Road Clinical Hospital at the Voronezh-1 station of JSC Russian Railways, we can offer the most advanced diagnostic methods and treatment regimens for hypertension.
We will be glad to see you in our department
contact number +7(473)265-54-97
Symptoms
Often, an increase in blood pressure is not accompanied by a deterioration in health and may go unnoticed by the patient, which is why it is so important to regularly measure blood pressure, especially for middle-aged and elderly people.
Manifestations of hypertension may include the following symptoms:
- headache, mainly in the morning after waking up;
- nosebleeds;
- hemorrhage under the mucous membrane of the eye;
- heart rhythm disturbance;
- blurred vision, flickering spots;
- tinnitus.
A sharp jump in blood pressure to high numbers, accompanied by a pronounced deterioration in well-being, is called a hypertensive crisis. Most often it occurs when systolic pressure rises to more than 180 mm Hg. Art. and/or diastolic over 120 mm Hg. Art. In this case, the patient experiences weakness, nausea, vomiting that does not bring relief, impaired consciousness, anxiety and fear, muscle tremors, and chest pain.
Diagnostics
There are a number of signs that require examination of the patient to exclude symptomatic arterial hypertension:
- Age younger than 20 and older than 60 when hypertension occurs at this age
- Islanded blood pressure
- High blood pressure numbers
- Frequent sympathoadrenal crises
- Hypertension during pregnancy, history of kidney disease
- Minimal changes in urine sediment
Mandatory studies:
- UAC and OAM
- Fasting plasma glucose
- Blood plasma content of total cholesterol, cholesterol, HDL, TG, creatinine
- Creatinine clearance
- ECG
Additional research:
- Uric acid, potassium in blood serum
- EchoCG
- Fundus examination
- Ultrasound of the kidneys and adrenal glands
- Chest X-ray
- Daily blood pressure monitoring
- Determination of pulse wave speed
- Glucose tolerance test (for plasma glucose >5.6 mmol/l)
- Quantification of proteinuria
In-Depth Research:
- Assessment of the condition of target organs - brain, myocardium, kidneys, great arteries
- Detection of secondary forms of hypertension
- Determination of catecholamines and their metabolites in 24-hour urine and blood plasma
Story
The history of the study of arterial hypertension dates back to the 40s of the 18th century. Then the Englishman S. Hales determined the height of the blood column in a glass tube inserted into the carotid artery of animals and humans. 100 years later, Karl Friedrich Wilhelm Ludwig invented a mercury manometer for recording blood pressure, and Goldblatt created a model of chronic arterial hypertension in a dog. In 1922, G. F. Lang created the neurogenic theory of arterial hypertension, and in 1948 he also proposed the term “hypertension.” Diagram of a pressure gauge by Karl Ludwig. copyright Farzan Filsoufi. Arterial hypertension is a socially significant disease and the most important risk factor for cardiovascular complications. The frequency in the Russian Federation is 39% in men and 46% in women. At the same time, in men, arterial hypertension is more often observed under the age of 40, and in women over the age of 50. A. L. Myasnikov called hypertension “a disease of the twentieth century,” there is some truth in this, because in areas of the modern world where primitive features of the economy, there is a low prevalence of hypertension.
Clinic
- Often asymptomatic and turns out to be an incidental finding during a visit to the doctor
- Frequent subjective manifestations are headaches in the occipito-parietal and temporal regions
- Cerebrovascular disorders are also possible - dizziness, tinnitus, spots before the eyes, decreased memory and mental activity
- Neurotic disorders - irritability, discomfort, fatigue, depression, sleep disturbance, uncertainty, anxiety
- 20-40% have cardiac pain syndrome
- Visual impairment
- Accent 2 tones over the aorta, hard pulse, tachycardia
- Changes in the boundaries of the heart, high apical impulse