Tricuspid regurgitation is the reversal of blood flow from the right ventricle back into the atrium, but is not a diagnosis in itself. This is not even a disease, but a consequence of a malfunction of the tricuspid valve, which closes the passage from the right atrium to the corresponding ventricle.
The condition can be primary or secondary, depending on the origin of the pathological process. Recovery is carried out surgically.
The prospects for a complete cure are good, but only in the early stages, when there are no anatomical defects in the heart or distant systems yet.
Fortunately, the duration of the initial phase is sufficient for a thorough diagnosis. The intervention is planned, except for exceptional cases.
The approximate time frame from the moment the deviation occurs to the formation of a clear clinic is 3-6 years.
Development mechanism
{banner_banstat0}
The essence of the pathological process is the disruption of hemodynamics at the local level and the formation of a persistent anatomical defect.
In the normal state of affairs, blood in the cardiac structures moves strictly in one direction, ending the cycle in the left ventricle and being transported to the aorta, and from there to its branches in a large circle.
The heart is represented by a group of chambers, each separated from the other by valves, which does not allow fluid connective tissue to move in the opposite direction.
The tricuspid structure closes the gap between the right atrium and ventricle. In case of weakness, insufficiency, or defects of the connective tissue, a reverse flow of blood or regurgitation occurs, which is called according to the name of the valve that causes the condition.
The result of the deviation is, firstly, a disruption in the transport of blood in the small circle, and secondly, an insufficient amount of it, which is released into the aorta.
This leads to generalized hemodynamic deviations, tissue hypoxia, and multiple organ failure in the future.
Causes of congenital tricuspid regurgitation
The most common causes of this congenital pathology are:
- underdevelopment of valve leaflets;
- abnormal development (number) of valve leaflets;
- connective tissue dysplasia;
- Ehlers-Danlos syndrome;
- Marfan syndrome;
- Ebstein's anomaly.
Tricuspid regurgitation in the fetus is very rare in isolation; it is usually combined with other heart defects. This valve insufficiency may be part of the mitral-aortic-tricuspid defect.
Forms of violation
{banner_banstat1}
Typing of the pathological process is carried out on two grounds.
Based on the origin of the anatomical defect, they talk about:
- Primary form. It develops spontaneously, against the background of cardiac problems themselves. Including aortic insufficiency, previous inflammatory, infectious conditions and others.
It is characterized by greater complexity from the point of view of cure and prospects for recovery, since correction requires not only the symptomatic component, but also the acquired defect.
This group also includes congenital factors caused by genetic defects and spontaneous deformations of the tricuspid valve.
- Secondary variety. Against the background of current pathologies of distant organs and systems.
Degrees of regurgitation
Another basis for classification is the degree of deviation from the norm. Also called stages of the pathological process.
Accordingly, they distinguish:
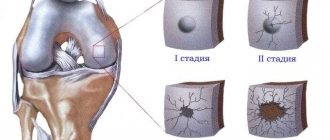
- Weakly expressed type. 1st degree. The amount of blood returning is not known exactly. The volumes of the jet do not exceed 1 cm in diameter. The intensity of manifestations with minimal tricuspid regurgitation is insignificant or completely absent, which makes early diagnosis a matter of luck. This is the best time to start therapy under the supervision of cardiac surgeons.
- Moderate type. 2nd degree. Characterized by disruption of normal blood flow in a volume of 2 cm, no more. Recovery is carried out surgically. The clinical picture is minimal, characterized by chest pain, shortness of breath during intense physical activity. There is a chance for a complete cure, the likelihood of the formation of persistent cardiac and extracardiac defects is present, but it is not yet great. Even if these occur, the likelihood of a high-quality, long life is maximum.
- Expressed type. 3rd degree. A stream of blood more than 2 cm in diameter. Chronic heart failure of congestive type develops. There are prospects for recovery, but they are not complete, and long-term, lifelong maintenance therapy is required.
- Terminal phase. 4th degree. Surgical assistance does not make much sense, since the heart, kidneys, liver, and brain are significantly changed. Recovery is impossible; palliative care is required to ensure an acceptable quality of life for the short remaining period of life. Death occurs from acute heart failure.
Classifications are used to accurately assess the patient’s condition, prospects for treatment, and determine diagnostic and therapeutic tactics.
Mitral regurgitation
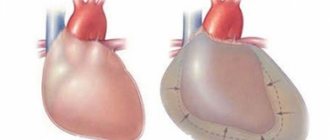
Mitral regurgitation is clearly observed with valve insufficiency or prolapse. At the moment of contraction of the left ventricular muscle, a certain volume of blood returns to the left atrium through an insufficiently closed mitral valve (MV). At the same moment, the left atrium fills with blood flowing from the lungs through the pulmonary veins. This flooding of the atrium with excess blood leads to overdistension and increased pressure (volume overload). Excess blood during contraction of the atria enters the left ventricle, which is forced to push more blood into the aorta with greater force, as a result of which it thickens and then expands (dilatation).
For some time, disturbances in intracardiac hemodynamics may remain invisible to the patient, since the heart, as best it can, compensates for blood flow due to the expansion and hypertrophy of its cavities.
With mitral regurgitation of the 1st degree, there are no clinical signs for many years, and with a significant volume of blood returning to the atrium, it expands, the pulmonary veins become filled with excess blood and signs of pulmonary hypertension appear.
Among the causes of mitral regurgitation, which is the second most common acquired heart defect after changes in the aortic valve, we can highlight:
- Rheumatism;
- Prolapse;
- Atherosclerosis, deposition of calcium salts on the valves of the mitral valve;
- Some connective tissue diseases, autoimmune processes, metabolic disorders (Marfan syndrome, rheumatoid arthritis, amyloidosis);
- Coronary heart disease (especially infarction with damage to the papillary muscles and chordae tendineae).
With mitral regurgitation of the 1st degree, the only sign may be the presence of a murmur in the area of the apex of the heart, detected by auscultation, while the patient has no complaints, and there are no manifestations of circulatory disorders. Echocardiography (ultrasound) can detect slight divergence of the leaflets with minimal disruption of blood flow.
Mitral valve regurgitation of the 2nd degree accompanies a more pronounced degree of insufficiency , and the stream of blood returning back to the atrium reaches its middle. If the amount of blood return exceeds a quarter of the total amount located in the cavity of the left ventricle, then signs of stagnation in the small circle and characteristic symptoms are detected.
The third degree of regurgitation is said to occur when, in the case of significant defects of the mitral valve, the blood flowing back reaches the posterior wall of the left atrium.
When the myocardium cannot cope with the excess volume of contents in the cavities, pulmonary hypertension develops, leading, in turn, to overload of the right half of the heart, resulting in circulatory failure in the systemic circle.
With grade 4 regurgitation, characteristic symptoms of severe disturbances in blood flow inside the heart and increased pressure in the pulmonary circulation are shortness of breath, arrhythmias, and the possible occurrence of cardiac asthma and even pulmonary edema. In advanced cases of heart failure, signs of damage to the pulmonary bloodstream include swelling, cyanosis of the skin, weakness, fatigue, a tendency to arrhythmias (atrial fibrillation), and pain in the heart. In many ways, the manifestations of severe mitral regurgitation are determined by the disease that led to damage to the valve or myocardium.
Separately, it is worth mentioning about mitral valve prolapse (MVP), quite often accompanied by regurgitation of varying degrees. In recent years, prolapse has begun to appear in diagnoses, although previously such a concept was quite rare. This state of affairs is largely due to the advent of imaging methods - ultrasound examination of the heart, which makes it possible to trace the movement of the valves of the MV during cardiac contractions. With the use of Doppler, it became possible to determine the exact degree of blood return to the left atrium.
MVP is typical for tall, thin people; it is often discovered accidentally in adolescents during examination before conscription into the army or undergoing other medical examinations. Most often, this phenomenon is not accompanied by any disturbances and does not in any way affect the lifestyle and well-being, so you should not be alarmed right away.
Mitral valve prolapse with regurgitation is not always detected; its degree in most cases is limited to the first or even zero, but at the same time, this feature of the functioning of the heart can be accompanied by extrasystole and disturbances in the conduction of nerve impulses through the myocardium.
If low-grade MVP is detected, you can limit yourself to observation by a cardiologist, and treatment is not required at all.
How dangerous is the disease?
{banner_banstat2}
Complications arise starting from the third, less often the second stage of the pathological process. Tricuspid valve regurgitation determines the following consequences for health and life:
- Acute heart failure. Disruption of the normal functioning of cardiac structures. It is characterized by a triad of signs: a decrease in blood output, a drop in local and generalized hemodynamics, and arrhythmic processes. It has a short period of development in an acute case; in a latent course, the duration of formation of a full-fledged picture is 2-4 weeks; death occurs as a result of stopping the work of a muscular organ.
- Cardiogenic shock. The condition is lethal in almost 100% of cases. There is no prospect of cure. Even with partial recovery, there is a guarantee of a repeat episode.
- Heart attack. Myocardial nutritional disturbances, acute tissue necrosis and, as a result, decreased functional activity. Heart failure develops with all its consequences.
- Stroke. Cerebral ischemia.
- Dangerous forms of arrhythmia leading to cardiac arrest.
Minor regurgitation provokes fatal complications in 0.3-2% of cases, often the result of a random coincidence.
Hemodynamically significant forms determine the risk of death in a wide range: from 10 to 70% and higher.
The main cause of death is not regurgitation, but organic defects of the heart and systems developing against its background.
Causes of acquired tricuspid regurgitation
Acquired tricuspid valve regurgitation is much more common than congenital regurgitation. It can be primary and secondary. The primary causes of this pathology include rheumatism, drug addiction, and carcinoid syndrome.
- Rheumatism is the most common cause of this pathology. In 20% of cases, it is recurrent rheumatic endocarditis that leads to deformation (thickening and shortening) of the valve leaflets, and the tendon threads also change in the same way. Very often this pathology is accompanied by stenosis of the right atrioventricular orifice. This combination is called combined tricuspid defect.
- Rupture of the papillary muscles can also lead to tricuspid regurgitation. Such ruptures occur during myocardial infarction or may have a traumatic origin.
- Carcinoid syndrome can also lead to this pathology. It occurs in certain types of cancer, for example, cancer of the small intestine, ovaries or lungs.
- Taking hard drugs very often leads to infective endocarditis, which, in turn, can cause tricuspid regurgitation.
The most common causes of secondary tricuspid insufficiency are the following diseases:
- dilation of the annulus fibrosus, which occurs with dilated cardiomyopathy;
- high degree of pulmonary hypertension;
- weakness of the right ventricular myocardium, which occurs in the so-called cor pulmonale;
- chronic heart failure;
- myocarditis;
- myocardial dystrophy.
Causes
{banner_banstat3}
Formation factors are divided into primary and secondary, according to the main forms of the pathological process.
Primary factors
{banner_banstat4}
- Burdened heredity. Leads to the development of tricuspid valve insufficiency. Problems arise during the prenatal period. In this case, there is a genetic predisposition. The exact mechanism, however, is not known.
One thing has been proven: in the presence of a sick parent, children are born with the defect in question and regurgitation in 12-15% of cases. Spontaneous defects of the perinatal period are possible, caused by internal and external factors.
- Spikes in the heart. These are small fibrin strands that disrupt the normal anatomical structure of the organ. They develop as a result of inflammatory processes of any type, especially infectious. This is a kind of protective mechanism, as well as further deposition of calcium salts to isolate the affected area.
- Previous heart attack. It ends with the replacement of functionally active tissues with weak, scarred ones, incapable of contraction, signal transmission, or spontaneous excitation.
If the process affects the tricuspid valve, the following options are possible: its complete fusion, stenosis, or functional failure, immediately leading to severe regurgitation. Recovery is urgent, surgical.
- Inflammatory pathologies of the heart (myocarditis and others). Accompanied by rapid destruction of tissue of cardiac structures. Treatment is urgent, in a hospital, with the use of antibiotics and NSAIDs, as well as steroids and diuretics.
- Rheumatism. Inflammatory pathology of a chronic nature, with frequent relapses and short periods of remission. Therapy is lifelong, using supportive tactics. If necessary, surgical correction of the consequences is performed.
Secondary factors
{banner_banstat5}
The secondary pathological process is caused by cardiac problems and extracardiac issues:
- Pulmonary hypertension and the development of specific abnormalities in the anatomical development of the heart. Requires urgent treatment in the early stages, since in the later stages there is no longer any sense. The main risks are smokers, alcoholics, asthmatics and patients with long-term COPD.
- Cardiomyopathy.
- Endocrine pathologies: hyperthyroidism, excess of adrenal hormones, their deficiency, diabetes mellitus and others.
Risk factors
{banner_banstat6}
They do not directly cause tricuspid regurgitation, but lead to the onset of the pathological process:
- Long-term smoking.
- Consuming alcohol in immoderate quantities.
- A long period of immobilization, without the possibility of vigorous activity. Development takes a long time, from six months or more.
- Drug addict.
- Excessive use of “dangerous” drugs: glycosides, antiarrhythmics, progestin agents, also hormonal medications, broad-spectrum antibiotics.
- Harmful working conditions affect chemical, hot production, and mines.
The reasons are considered as a whole; a system of development factors is possible.
Modern methods of treating tricuspid valve insufficiency in children in Israel
The pediatric cardiology department at Hadassah is headed by Dr. Azariah Rein. After receiving higher medical education at the Hebrew University, he trained at the Shaare Zedek Clinic. After receiving his degree, he became a university professor in Jerusalem and Harvard. Permanent member of the Academic Council of Israel, engaged in scientific research.
Cardiac surgery is under the direction of Professor Eldad Erez, holder of two higher qualifications, specializing in the treatment of congenital defects in children. The future doctor of medicine's internship took place in Haifa and Beilinson, his residency in Atlanta (USA), where the doctor mastered the technology of heart transplantation. Erez teaches medical students in Tel Aviv and Jerusalem, and is the author of scientific works.
The first day after hospitalization in the hospital is reserved for examination, medical history, and documentation in Hebrew. Throughout the entire stay in the hospital, the little patient and his parents are accompanied by a Russian-speaking consultant.
Treatment for tricuspid valve insufficiency in children is selected strictly on an individual basis and depends on the degree of regurgitation of blood flow (1, 2, 3 or 4):
- 1 - subtle throw or touch of the tricuspid valve;
- 2 — reverse ejection is determined at a distance of 2 cm from the atrioventricular opening;
- 3 — return of blood from the right ventricle to a distance of more than 2 cm;
- 4 - regurgitation in the right atrium over a significant extent.
The first stage may be limited to medical observation or conservative therapy. Starting from the second, the nature of the intervention will depend on the intensity of casting, complications caused by the defect, and the presence of combined anomalies.
Elimination of the defect and the consequences of improper functioning of the heart is carried out through medication or surgery.
Drug therapy
The conservative approach includes drugs that ease the work of the heart and reduce pulmonary hypertension. This list includes diuretics, anticoagulants, b-blockers, glycosides, drugs that increase metabolism, and ACE inhibitors.
Surgical intervention
The main types of surgical techniques are repair of the patient's own valve or prosthetics using a bioprosthesis or a mechanical analogue.
Indications for prosthetics are considered to be severe changes in the valves. The material for the manufacture of a biological prosthesis is the aorta of an animal (pig). Unlike a mechanical one, a bioprosthesis significantly reduces the development of thromboembolism, but lasts only 10 years, requiring repeated replacement.
Preference is given to plastic correction, but only if no pronounced changes in the structure of the valves are detected. The obvious advantages of this procedure are minimal postoperative complications and a reduction in the rehabilitation period. In addition, restoration using one’s own, normally functioning tissues increases resistance to infections and eliminates the need for constant use of special medications.
Characteristic symptoms
Manifestations depend on the stage of the pathological process. A hemodynamically insignificant variety has no signs at all.
Typical signs in other situations include:
- Liver lesions. They make themselves known in the later stages. They are determined by pain in the right hypochondrium, an increase in the size of the organ, and yellowness of the skin due to excess bilirubin. A gradual formation of insufficiency is possible.
- Abdominal pain of unknown localization. Wandering, radiating to the iliac regions. Acute discomfort is not typical, therefore it is impossible to confuse it with the clinical picture of appendicitis.
- Shortness of breath for no apparent reason. It develops first against the background of intense physical activity, then occurs in a state of complete rest. Significantly reduces quality of life.
- Polyuria. As a result of developing renal failure. At later stages (3-4), with primary damage to the excretory system, it is replaced by a reverse process. Daily diuresis is 500 ml or less.
- Tachycardia. The heart rate reaches 120-150 beats. They are full-fledged, regular. Type - sinus. Less often paroxysmal.
- Weakness, lack of ability to work.
- Feeling of constant cold. The patient freezes because the intensity of peripheral circulation decreases.
- Increased pressure in the veins. Objectively, the symptom is manifested by swelling of the cervical vessels, their intense pulsation, and visible tension. Not only the doctor, but also the patient himself or the people around him can determine the sign. However, blood pressure drops in most cases. Not significant, however, clinical significance is present.
- Swelling of the lower extremities. As a logical continuation of increasing renal failure.
- Breathing problems.
As a result, the patient has a whole range of symptoms from both distant organs and systems, and the cardiac structures themselves. The reason for all the sensations lies in the disruption of blood circulation, both in the large and in the small circle.
What causes regurgitation of blood through the tricuspid valve?
The normal movement of blood through the right parts of the heart is ensured by the ability of the tricuspid valve leaflets to move synchronously with the phases of systole and diastole of the myocardium.
Valve defects, depending on the morphological substrate and functional disorder, are divided into:
- stenosis, which develops due to calcification, an inflammatory lesion. The pathology is characterized by a narrowing of the lumen of the orifice, which reduces the volumetric velocity of blood flow from the atrium to the ventricle;
- regurgitation (in the old terminology - insufficiency) - elongation of the chords, damage to valve structures by infectious processes contributes to the expansion of the lumen and pathological movement of blood during ventricular systole not only into the pulmonary artery, but also into the atrium;
- combined defect.
Pathologies of the tricuspid valve are rare acquired defects and most often develop as secondary changes against the background of decompensation of the condition.
The most common causes of tricuspid regurgitation:
- infective endocarditis is a bacterial pathology characterized by the entry of the pathogen into the blood and selective damage to the endocardial tissue. Involvement of the valves of the right half of the heart most often develops in injection drug users;
- chronic rheumatic heart disease is a consequence of an infection with beta-hemolytic streptococcus, which has cross-antigens with valve structures;
- systemic connective tissue pathologies: Ellesre-Danlos syndrome, Marfan syndrome, undifferentiated dysplasia syndrome;
- Ebstein's anomaly is a congenital valve malformation in which the leaflets develop not from the connective tissue of the fibrous ring, but from the myocardium of the right ventricle. The first signs of disorders are diagnosed during examination of the newborn in the maternity hospital;
- dilated cardiomyopathy. The resulting regurgitation is considered relative, since an increase in the size of the right atrioventricular orifice is associated with a pathological expansion of the cavities of the heart;
- carcinoid syndrome is a specific reaction of the body to malignant tumors of various locations. It is formed in response to the release of the metabolic product of cancer cells into the bloodstream: diarrhea, nausea, hot flashes (as during menopause), abdominal pain.
Most often, grade 1 tricuspid valve regurgitation is diagnosed in patients with decompensated mitral valve disease. Impaired blood outflow from the left atrium increases pressure in the pulmonary circle (pulmonary vessels), and secondarily in the right ventricle.
Diagnostics
{banner_banstat7}
The examination is carried out under the guidance of a cardiologist, and if the process is proven, the specialized surgeon continues to work. He is also responsible for prescribing treatment.
Scheme of events in the correct order:
- Oral questioning of the patient regarding complaints, their duration, as well as collecting anamnesis. This way the doctor understands the direction of further examination.
- Blood pressure measurement. Usually it is slightly reduced. Heart rate is higher than normal. The rhythm is correct; as it progresses, spontaneous premature beats (extrasystoles) occur.
- Listening to sound (auscultation). A sinus noise of reverse blood flow is detected. Tones can be either normal or dull.
- Daily monitoring. To record cardiac performance indicators over 24 hours in dynamics. It is most often used as the first method, after a routine examination. Provides comprehensive information about the movement of blood pressure and heart rate during the day.
- Electrocardiography. Assessment of the functional state of the heart.
- Echocardiography. Method of visualization of cardiac structures. It is carried out as a matter of priority, since it allows one to detect organic abnormalities on the part of the tricuspid valve.
- MRI or CR (much less often). It is carried out to detail the image of the heart and surrounding tissues.
- Pulmonary artery pressure measurement.
- Load tests. At an early stage, later not used due to significant danger.
The methods are aimed both at establishing the fact of an anatomical defect and at verifying the alleged diagnosis.
Treatment methods
{banner_banstat8}
Therapy is carried out under the full supervision of a cardiac surgeon. Methods of exposure depend on the stage of the pathological process.
Grade 1 tricuspid regurgitation is the best time to start therapy. But there are no symptoms yet, identification is incidental (random), and does not pose any difficulties during a targeted search.
At this stage, dynamic observation for 3-5 years is indicated. In the absence of progression, with stagnation of the process, there is no need for treatment. Sometimes patients can live a quality life without knowing about their condition, without major restrictions.
Tricuspid regurgitation of grade 2 and higher is corrected strictly surgically. There are several intervention options.
But before the treatment stage, it is necessary to stabilize the patient’s condition, if there is time for that (planned operations).
Drugs used:
- Antiarrhythmics in the minimum dosage to restore an acceptable heart rate (Amiodarone, Hindin).
- Beta blockers (Metoprolol).
- Glycosides. In order to normalize myocardial contractility.
- Cardioprotectors.
- Anticoagulants. To prevent the formation of blood clots, which cause frequent premature death of patients.
- Diuretics in the treatment of early manifestations of renal conditions.
The duration of the preparatory period varies from 2 to 4 months, possibly more.
By the time of surgery, the rhythm should be stable, correct, blood pressure within the reference value or close to it.
Depending on the stage of the pathological process and the nature of the changes, plasty or prosthetics of the tricuspid valve is indicated. Both methods are generally equivalent.
Correction of pathologies and defects of distant organs is carried out under the supervision of specialized specialists. The list of techniques is wide and is determined based on the severity of the process.
Attention:
The use of folk remedies is impossible. Since the effect of them in case of organic deviation on the part of the cardiac structures is zero.
Changing your lifestyle will also not play a key role. It makes sense to give up smoking, alcohol and drugs. When carrying out severe therapy for third-party pathologies, correction by a treating specialist is recommended.
Diagnosis and treatment of pathology
The diagnosis of tricuspid regurgitation is made according to the following data:
- clinical examination: edema, ascites, increase in liver size, hepatojugular syndrome (liver pulsation). Auscultation reveals a systolic murmur along the left edge of the sternum, weakening of the fundamental tones;
- electrocardiogram (ECG): signs of hypertrophy of the right sections, often – atrial fibrillation, blockade of the right bundle branch;
- X-ray of the chest organs - expansion of the cardiac shadow due to the right parts;
The verification method is echocardiography (echo-CG), with the help of which the degree and stage of disorders are established, pressure in the cavities, blood flow speed and volume of regurgitation are measured.
Echocardiography is used to safely diagnose Ebstein's anomaly in a fetus in the third trimester of pregnancy.
To correct the patient's condition, conservative and surgical treatment methods are used.
Pharmacological support is aimed at eliminating signs of right ventricular failure:
- diuretics (diuretics) – Furosemide, Torsid to remove excess fluid from the body;
- antihypertensive drugs to reduce systemic pressure in blood vessels;
- cardiac glycosides - Digoxin, Korglykon - to maintain the strength and frequency of myocardial contractions;
Surgical correction is prescribed to patients with moderate regurgitation and involves complete replacement of the valve with installation of a prosthesis (biological or mechanical) or plastic surgery of the right atrioventricular orifice (narrowing of the lumen using sutures). Patients who have undergone surgical correction of regurgitation are not suitable for military service.
Forecast
{banner_banstat9}
Depends on the stage and nature of therapy.
- At the first stage, the survival rate is 100%, especially if there is no progression of the condition.
- The second is associated with a probability of 85%.
- Third - 45%.
- The fourth or terminal puts an end to the patient, giving no chance. The median is 1-2 years, often even less.
When carrying out complex therapy, it is possible to stabilize the conditions of even the most severe patients, prolonging life for several years.
Favorable prognostic factors:
- Period of youth.
- Absence of somatic pathologies, bad habits, complications after the operation.
- Good family history.
- Response to treatment.
- Reduction of symptoms.
Determining the possible outcome falls on the shoulders of the cardiologist. In order to say anything concrete, you need to at least carry out a full diagnosis.