Of the many diseases of the urinary system, the pathology with the most unclear etiology and the most difficult to diagnose is interstitial cystitis.
The first description of the disease was given back in 1915 by G. Hunner, who described the case of 8 women with prolonged pain in the suprapubic region, painful urge to urinate, and frequent urination day and night. Cystoscopically, he observed in these patients changes in the mucous membrane of the bladder such as linear defects and even deep ulcerations.
The changes named after him (Hunner's ulcer) were considered pathognomonic for this disease. The clinical picture is formed by a chronic complex of symptoms from the lower urinary tract, consisting of pain in the suprapubic region, frequent urination and urgency.
Pain in the suprapubic region
Routine urine tests, such as urinalysis and culture, do not identify the etiological factor. The Pap smear does not show any pathology. Patient complaints (since the disease is estimated in 90% of women) suggest inflammatory changes. Symptoms continue for a long time and do not disappear with conventional treatment.
There is probably no urologist to whom a patient would not turn, having in her hands a list of all the medications used to treat bacterial cystitis, test results, and a list of doctors who could not cure her.
How common is interstitial cystitis?
The content of the article
Epidemiological studies indicate that this disease is much more common than clinically recognized. For example, uch. Oravisto, studying the population of Helsinki, found the disease in 18.1/100,000 women and 1.2 new cases per 100,000 women per year. Ph. Research Helda and Ph. Hanno showed twice the incidence of interstitial cystitis in the United States.
Direct and indirect costs associated with the treatment of this pathology are approximately $500 million.
Based on questionnaires, these researchers rated patient-reported quality of life as significantly lower, even than that of patients with ESRD. Perhaps this fact sheds light on the influence of the mental factor on the level of IC symptoms.
Symptoms of interstitial cystitis
According to Messing, interstitial cystitis can be described in one sentence as a triad of the following clinical signs:
- the presence of irritating symptoms from the lower urinary tract;
- characteristic cystoscopic image;
- lack of objectively identified reasons.
One of the characteristic clinical features of this disease is the sudden onset of the disease, spontaneous remissions, lasting on average about 8 months. The disease quickly reaches a certain level of severity of illness, constant for a given patient, at which it stabilizes for a long time. Worsening of symptoms is very rare.
Patients report frequent urinary tract infections in childhood (10 times more often than controls).
How is interstitial cystitis diagnosed?
In 1987, a workshop of the National Institute of Arthritis, Diabetes and Digestive and Kidney Diseases was held in Maryland to develop uniform diagnostic criteria for the diagnosis of interstitial cystitis. The developed recommendations made it possible to simplify and increase the efficiency of diagnosis and identification of patients who, until now, could have been unsuccessfully treated with a diagnosis of other diseases with symptoms similar to IR.
It should be emphasized that the diagnosis of interstitial cystitis is based on the exclusion of other diseases, such as carcinoma in situ, chronic bacterial cystitis, tuberculous cystitis or rare inflammations - allergic, eosinophilic, cystitocystic, granulomatous.
The main diagnostic criterion (after excluding the above diseases) is the so-called Hanner's ulcer or small scattered hemorrhages on the surface of the mucous membrane of the bladder after double filling of the bladder under a pressure of about 100 CMH for about 2 minutes.
Petechiae should be present in at least 3 quadrants of the bladder, with a minimum of 10 per quadrant, but lesions in the path of the cystoscope should not be considered. Hanner's ulcers can range from linear defects of the mucosa to irregular bleeding areas of the mucosa that disappear as the bladder fills.
An ulcer can occur in any area, including the triangle. It is most often up to 2 cm in length and has a different color - from white to brown. This change occurs only in the most severe forms of inflammation, the frequency is about 5%. The results of cystoscopy of these changes (ecchymosis, characteristic ulcerations) make it possible to diagnose interstitial cystitis.
Interstitial cystitis
In addition, the so-called positive factors in the diagnosis of the disease are taken into account, including the patient’s subjective sensations - pain accompanying the filling of the bladder immediately after urination, and pain in the suprapubic, perineal, vaginal or urethral areas.
As mentioned earlier, the diagnosis of IC is based mainly on the exclusion of other pathologies of the bladder or pelvis of known etiology (the so-called diagnosis of exclusion). The diagnosis of interstitial cystitis is excluded by the following data:
- Patients' age is up to 18 years.
- Bladder capacity is more than 350 ml.
- Absence of the urge to urinate when filling the bladder with 150 ml of liquid (filling rate 30-100 ml/min) and the presence of involuntary contractions of the bladder during such an examination.
- Daytime urination less than 5/12 hours and no nighttime urination (or less than 2).
- Detection of radiation, tuberculosis and chemical changes in the bladder.
- Lower urinary tract infection in the last 3 months.
- Relief of symptoms after treatment with antimicrobial drugs, antispasmodics.
- Tumor changes in the bladder, urethra.
- Tumors of the genital organs.
- Stone in the lower urinary tract.
- Inflammation of the genital organs, bacterial and viral.
- Urethral diverticula.
Over the past decades, i.e. Since the development of the above-mentioned diagnostic criteria for IC, the number of new cases has increased sharply, and thus the number of patients. People treated for interstitial cystitis lobbied in the US for several years and created the Interstitial Cystitis Association (founded, among other things, by a doctor treated for diagnosed interstitial cystitis), a pressure group that forced the FDA to take action to improve treatment for interstitial cystitis. .
6-day immersion course
We began treating our first patients with a variety of pelvic floor dysfunctions at Stanford University in 1995 during routine medical appointments. In 2003, we opened a private practice as a 6-day immersion clinical course in Santa Rosa, California. The course, designed for 14 patients and open for a year, eventually introduced the Wise-Anderson Protocol. This protocol teaches patients how to restore the function of chronically tight pelvic floor muscles and reduce anxiety. The Wise-Anderson Protocol, performed independently at home by patients who have been trained by us, has helped many return to normal life. Following the protocol helps patients eliminate the need to seek additional professional help. For ten years, research has documented our results in teaching patients to self-administer the protocol. For further information, please follow the link to our blades page.
For questions about cost and eligibility please fill out the form below, email us at or contact our office at +1 (707) 332-1492.
SYMPTOMS OF INTERSTITIAL CYSTITIS (IC)
(Most patients exhibit two or more symptoms)
Urinary frequency and urge to urinate
- Urinary frequency ranges from annoying to debilitating.
- After urinating, patients feel that the bladder has not been completely emptied and they have the feeling that they need to urinate again.
- Patients have to stay close to the toilet.
- Sometimes patients cannot help themselves when they feel the need to empty their bladder.
- Very often, these symptoms disturb night sleep and lead to lack of sleep, because... patients have to get up frequently at night.
- Although the symptoms of interstitial cystitis (IC) are similar to those of a chronic urinary tract infection, the urine usually does not contain bacteria.
- But symptoms can get worse if someone with IC gets a urinary tract infection.
Dysuria (pain or burning when urinating)
- Dysuria (pain or burning when urinating) can be very painful and can make urination an ordeal, leading to further pain.
- Pain or burning when urinating is caused by pelvic floor dysfunction.
- Sometimes people experience pain after, rather than during, urination.
- When the problem with chronic spasms and myofascial tension in the pelvic muscles is resolved, for many patients the pain and burning sensation when urinating also goes away.
Nocturia (frequent urination at night)
- Very often, nocturia (frequent urination at night) leads to nervous exhaustion in patients, because. They don't get enough sleep.
- Chronic fatigue from lack of sleep contributes to a vicious circle: tension, pain, defensiveness and anxiety.
Weakened stream and delayed urination
- It is very important to accurately determine the source of this symptom: whether the weakened flow is caused by an enlarged prostate or something else.
- Some patients with pelvic muscle pain experience delays when starting to urinate.
- Retention may also become worse if the bladder does not empty for longer than usual (tension of the muscles that hold urine leads to a spasm that does not immediately relax when urinating).
- A weakened flow can also affect self-esteem and lead to hypochondria, especially in young people.
- If these symptoms are caused by pelvic muscle pain, then when pelvic floor function is restored, the strength of the jet may improve.
Perineal pain (pain between the anus and scrotum)
- Perineal pain can be excruciating and constant.
- The perineum is the place where most of the pelvic floor muscles are attached, and therefore this place is a source of referred pain (the sensation of pain not in the place where it originates, but in another place where the pain is “referred”).
- This pain is worse when sitting or standing, and when riding a bicycle.
- The perineum and anal sphincter are the places where patients experience the sensation of “sitting on a golf ball.”
- About 79% of patients in our 2009 study complained of perineal pain.
- We have proven that the abdominal and pelvic muscles reflect pain in the perineum (rectus abdominis, adductor, coccyx).
Pain while sitting
- When sitting, patients with pelvic pain suffer even more. This symptom complicates all aspects of the patient's life.
- Patients have to sit on something soft
- Pain in a sitting position brings suffering when the patient is forced to sit for a long time while driving or while flying on an airplane.
- Sometimes patients are forced to register for disability, because... they cannot do sedentary work
- Discomfort/pain while sitting may be worse and may be felt in the front or back of the pelvis, or both.
- Pain while sitting usually gets worse towards the end of the day, after sitting all day.
Pain in the genitals
- In women, pain appears on one side of the vagina and is accompanied by pelvic pain.
- Genital pain is usually referred to the levator ani muscle in the pelvic floor.
Pain in the suprapubic region
- Pain in the suprapubic region is a common symptom and occurs in patients with urinary problems
- Sometimes pressure in this area can be felt in the anorectal area or cause pain in the bladder.
- The pain is felt on one side or in the middle.
Coccyx pain/coccydynia
- Pain in the tailbone is a typical symptom.
- Tailbone pain is usually referred from the pelvic floor or the muscles that attach to the tailbone, but not from the tailbone itself.
- Pain in the tailbone can be caused by pain after bowel movements.
Lower back pain
- Low back pain often confuses patients and doctors because... it is reflected from the pelvic floor muscles and does not originate in the lower back itself.
- Discomfort is experienced on one side, but can also migrate.
The appearance or reduction of discomfort after defecation
- The appearance or reduction of discomfort after defecation occurs when tense pelvic muscles relax.
- Discomfort after bowel movements can be especially bothersome if it worsens symptoms throughout the day.
- This symptom, when it appears in the absence of hemorrhoids or anal fissures, has been little studied, but in our opinion it is typical.
- The mechanism of defecation involves filling the rectum with feces, after which the internal anal sphincter and puborectal muscle are commanded to relax, leading to an urgency to defecate.
- After stool passes through the relaxed anal sphincter, the internal anal sphincter reflexively closes.
- We believe that in patients whose symptoms increase after defecation, the internal anal sphincter closes too tightly, i.e. it contracts more than it was before the bowel movement, and this results in a painful spasm.
- In patients whose muscle tension in the pelvis decreases, pain after bowel movements also decreases.
Low libido (low interest in sex)
- Decreased interest in sex is a typical symptom of pelvic pain.
- We believe that low libido is the result of anxiety, low self-esteem and pelvic pain, which interfere with sexual arousal and interest.
- Getting rid of pain and dysfunction of the pelvic muscles also resolves the problem of low libido.
Anxiety and catastrophic thinking
- The worst thing about pelvic pain is the frightening thought that this pain will never go away.
- This fear occupies all the patient’s thoughts, prevents him from living a full life and paints the future in dark colors.
Social isolation and difficulties in intimate relationships
- Social isolation is caused by pain, depriving patients of the opportunity to live a full life.
Violation of self-esteem
- Self-esteem in patients with pelvic pain decreases, because... they worry that people will avoid them.
Sleep disturbance
- Sleep disturbance is a typical symptom
- Many patients wake up anxious, wondering if the pain has gone away and feeling disappointed if it hasn't.
- Patients wake up due to the need to urinate or because of pain and anxiety
- We published an article about increased morning cortisol levels in patients with pelvic pain. Cortisol and Men with Chronic Prostatitis – Poster presented at the Urological Association meeting, 2007
Helplessness and hopelessness
- Helplessness is caused by the patient's inability to stop the debilitating pain.
- Hopelessness occurs when patients begin to think that nothing can help them.
Anterior pain points and muscle tension areas
- In practice, we have seen that in patients diagnosed with IC, pain points are located in the front, in the rectus abdominis muscle, in the anterior levator and in the obturator internus muscle.
- Self-administered exercise therapy and stress reduction can help reduce symptoms.
Dyspareunia (pain associated with sexual intercourse)
- Pain is felt during or after sexual activity, outside or inside the vagina, or in both places.
- When palpating the pain points, the pain can be reproduced.
Increased symptoms after taking certain foods
- In their article in the Journal of Urology, Moldwin et al write: Many patients with interstitial cystitis (IC) experience worsening symptoms after eating certain foods (tea, coffee, alcoholic and carbonated drinks, citrus juices and fruits, artificial sweeteners and hot peppers).
- However, we observed patients without a diagnosis of IC whose symptoms also increased after eating certain foods. Thus, a reaction to a certain food cannot be considered a characteristic sign of IC.
Increased symptoms with stress
- Normal and increased stress lead to increased symptoms.
- When stress causes pelvic pain, it also triggers a tension-anxiety-pain-defense cycle that continues after the stress has passed.
Increased symptoms with concomitant symptoms
- Interstitial cystitis (IC) may be accompanied by irritable stomach syndrome, fibromyalgia, vulvodynia, vulvar vestibulitis, pelvic floor dysfunction, Raynaud's syndrome, migraines, etc. Many patients with IC suffered psychological trauma in childhood and suffer from anxiety.
Histopathological picture
The purpose of a microscopic examination of a biopsy of the bladder mucosa is to exclude intraepithelial bladder cancer and tuberculous cystitis. There may be no changes in the microscopic image of interstitial cystitis, but most often the urothelial epithelium becomes thinner and hemorrhagic foci are visible underneath.
Microscopic image of interstitial cystitis
There is swelling or fibrosis of the lamina propria, an increase in the capillary blood vessels located under the epithelium, the wall of which is thickened. In later stages, fibrotic changes appear within the muscularis propria (sometimes leading to fibrosis).
Within the lamina propria and within the muscle tissue there are lymphocytic infiltrates, plasma cells, eosinophils and mast cell infiltrates. The presence of the latter is an important diagnostic criterion. Demonstration of 20 mast cells per 1 mm2 is a factor confirming the diagnosis of IC, and may be a marker of this disease.
A characteristic feature is also infiltration around the nerve fibers in the wall of the bladder. In the most severe form, Hanner's ulcer, the absence of epithelium is visible, and the infiltration of inflammatory cells covers all layers of the bladder wall (pancystitis). Deposition of immunoglobulin IgA particles in the mucosa and submucosa has been reported, and the presence of Tamm-Horsfall glycoprotein deposits in the mucosa has been demonstrated in some cases of interstitial cystitis.
A histopathological pattern similar to IC can be found in bladder mucosal ulcers and during healing, such as after biopsy.
Possible complications
Constant inflammation and damage to the bladder mucosa lead to the following complications:
- With a long course of the disease, the maximum capacity of the bladder decreases and the elasticity of its walls decreases. A shriveled bladder is formed due to the replacement of healthy tissue with scar tissue.
- Salt deposition and the formation of stones in the bladder due to disruption of the natural process of urination.
- Development of renal failure due to an increased risk of impaired renal filtration function.
- A gradual decrease in quality of life and loss of social roles due to constant severe pain and frequent urination.
- Painful sexual intercourse and related sexual and marital problems.
- Chronic stress and the development of clinical depression due to constant pain and disrupted sleep.
Etiology of I. cystitis - characteristic features of the structure of the bladder epithelium
It has not yet been possible to explain the etiology of this disease. Clinical and histological findings show various changes in the bladder wall. It is not known exactly which of them are primary and which are secondary. The multiplicity and ambiguity of the observed pathological changes inside the bladder have become the source of many theories explaining the cause of the disease.
Perhaps understanding the structure and function of the bladder wall will help explain the source of symptoms and possible causes of IC.
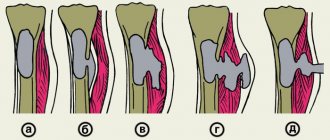
The inner wall of the bladder is the mucous membrane. In an empty bladder, it is highly folded due to the fact that it lies on a thin submucosa. As the bladder fills, the folds stretch, allowing the wall to adapt to the increased volume.
The outermost layer of the mucous membrane is a special epithelium of the urinary tract (urothelium) called transitional epithelium. The name comes from the fact that morphologically it is an intermediate form between single-layer and multilayer squamous epithelium. The number of cell layers varies, also depending on the distension state of the bladder, it ranges from 3 to 7 cell layers. As with other epithelium, the cells lie on a basement membrane.
Transitional epithelium of the bladder
Within this epithelium, three zones are clearly defined. The basement membrane is in direct contact with the basal zone, which consists of a single layer of small cylindrical cells (in the contracted bladder and flat in the distended bladder), from which, after successive divisions, daughter cells form more superficial layers.
The intermediate layer consists of 4-5 layers of large cells in the distended bladder and 6-7 contracted bladders. These cells allow these cells to slide past each other due to the fact that their cell membrane has a thin layer of compounds called glycosaminoglycans, of which daughter cells form more superficial layers after subsequent divisions.
The superficial zone is the most important for the proper functioning of the bladder wall as a barrier. The cells that make up this zone have several unique features not found in other tissues, and it is perhaps because of their uniqueness that the urothelial epithelium forms such a rigid boundary to urine components.
Urine reaches the bladder due to the content of many substances, including urea, salt, and proteins that make up a hypertonic solution. The osmotic pressure of urine - depending on the level of hydration of the patient - is 2-4 times higher than in the capillaries of the submucosal membrane of the bladder. Consequently, if the transitional epithelium were permeable to water, it would slip out of the vessels and, on the other hand, would penetrate deep into the wall of the toxic components of the urine.
We do not observe this phenomenon under proper conditions. Physical, chemical and morphological factors of the cell are equally responsible for the density of the surface epithelial layer. Fluctuations in one of these factors may be the cause of symptoms classified as interstitial cystitis.
The cells that make up the surface layer have the structure of large flat hexagons. Most often they have two cell nuclei (sometimes more), as they are formed as a result of the fusion of neighboring cells. This creation is called a syncytium. They are also called umbrella cells because, like a canopy, they cover cells in a deeper layer.
The cell membrane on the lumen side of the bladder is thicker than that covering the rest of the cell surface. Inside it, there are specific cup-shaped areas with a concavity directed outward, and, connecting with thinner fragments of the membrane, they cause its angular bend, characteristic of the urothelium. These segments are called asymmetric unit membranes because the outer portion is thicker than the inner.
Through electron microscopy, the AUM regions have been shown to be composed of multiple subunits, each consisting of 6 smaller elements arranged in a star shape.
Just under the cell membrane in close proximity to the AUM there is a dense network of fibers - the so-called microfilaments. They form ligaments that connect to the AUM segments. The cytoplasmic ends of the microfilaments converge and connect to another unique structure of the urothelial cell. The presence of discoid vesicles (fusiformes on a cross section, FV – fusiforme vesicles) was detected in the layers of the cytoplasm adjacent to the surface of the cell membrane.
The membrane surrounding these vesicles is identical in structure to the AUM segments). Presumably, these bubbles are deposits of plasma on the outer membrane of the cell. When the bladder contracts, the surface area of the urothelium also decreases, both due to its folding and due to a decrease in the area of the epithelium. The cells reduce their surface area facing the bladder lumen, probably in such a way that the previously described microfilaments, contracting, draw the AUM segments into the cell, thereby reducing the temporary “excess” of the cell membrane.
As the bladder fills, these bubbles rupture and become embedded in the outer surface of the cell membrane as flat structures. It is possible that damage to the transport mechanism of the AUM segment may be responsible for the development of symptoms of interstitial cystitis, since, by preventing adequate coverage of the surface of the bladder, they lead to penetration of urine components into its deeper layers.
The surface of the transitional cellular epithelium is covered with a thin layer of specific organic compounds called glycosaminoglycans. A similar layer, called the superficial layer, is found in the intermediate zone of the urothelium. It coats individual cells and allows them to slide past each other, so they can change their position as the bladder fills.
Glycosaminoglycans play an important role in protecting the surface of the bladder wall from the harmful effects of urine components. They prevent adhesion to epithelial cells and infiltration of the walls by microcrystals, proteins, bacteria and even cancer cells. Thus, they have antibacterial and anticancer properties and prevent the formation of urinary stones.
These properties are due to the binding of water molecules on its surface. It is this aqueous layer that creates the environment that separates the cells from the hypertonic urine. This feature is a result of the special structure of these compounds.
Glycosaminoglycans are a group of complex organic compounds that play an important role in the structure and function of cells. They are part of the cell membrane, including a signaling role, and are also part of the extracellular matrix. They are long polyanionic chains consisting of disaccharide subunits (one of them is hexozuronic acid, the other is hexosamine) with attached sulfate groups, to which they owe a negative charge (the ability to bind water molecules with ionic bonds).
There are three groups of glycosaminoglycans:
- Polyuronides: GAGs without sulfate residues - for example, hyaluronic acid.
- Sulfopolyuronides: GAGs containing sulfate moieties - for example, chondroitin 4-sulfate and 6-sulfate, dermatan sulfate, heparan sulfate and heparin.
- Polysulfates; GAGs containing only sulfate residues - for example, keratan sulfate.
With the exception of group 1 glycosaminoglycans, all of them are in the form associated with the protein core, these compounds are called proteoglycans. They are synthesized by epithelial cells of the urinary tract. The high content of sulfate and carboxyl groups determines the negative charge of GAGs. It is thanks to these polyanionic properties that water molecules are connected by ionic bonds, and a special barrier is created on the surface of the urothelium.
Structure of extracellular matrix proteoglycans (scheme)
In addition, they are involved in cell proliferation, differentiation, and mutual recognition, for example, during embryonic development and the creation of new tissues (for example, adhesive particles). Some growth factors are also proteoglycans. The layer covering the epithelium of the bladder contains representatives of each of the discussed groups of glycosaminoglycans.
Another very important factor determining the integrity of the epithelium of the urinary tract and its functioning as a waterproof barrier to urine and water is the specific connections between the cells of the surface layer - umbrella cells.
In every tissue, to maintain its structure, cells communicate using certain molecules located on the surface of the cell membrane. In addition, neighboring cells create structures that close the space between neighbors, others create “gates” that allow only certain substances to pass through. Based on the electron microscope image, connections were identified in which cell membranes are in direct contact with each other, closing joints and a type where the space is 15-35 nm (adhesive type connections - desmosomes).
Some tissues have communication junctions (2 nm wide gap junctions), such as synapses.
Between adjacent cells of the superficial layer of the urothelium there is a connection called a tight junction. It is so dense that it allows you to maintain an ion concentration gradient. The junction surrounds the entire chamber, resulting from the fusion of the cell membranes of contacting cells and forms a 500 nm wide band located close to the outer surface of the cell.
Cell membrane proteins also bind to each other, sealing the junction. This entire structure also prevents water from the body from entering the hyperosmotic environment inside the bladder.
As can be seen from the above description, there are many elements, damage to which can lead to structural and functional damage to the mucous membrane and deeper layers of the bladder wall, which can lead to symptoms associated with interstitial cystitis.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Diagnosis of the disease
First, the urologist examines and interviews the patient at the appointment. The woman is indicated for a gynecological examination. It is important to tell your doctor about all problems in the body.
Specialists prescribe laboratory tests. A nonspecific inflammatory process, an increase in antibodies to any cells, and possibly a hormonal imbalance are detected in the blood. When analyzing urine, laboratory technicians find a large amount of protein, also indicating inflammation. If the disease is severely developed, experts determine the presence of stones in the urine.
The most informative instrumental diagnostic methods are:
- X-ray with contrast agent;
- Cystoscopy;
- Ultrasound of the bladder;
- Measuring intravesical pressure (cystometry).
Doctors usually rule out other pathologies of the genitourinary system using various tests used in the Russian Federation, Europe, and the USA.
Sometimes urologists diagnose bacterial cystitis or any other disease of the genitourinary system of viral or fungal origin in a patient. If long-term therapy with antibiotics, antiviral or antifungal drugs does not bring results, an interstitial type of inflammation can be suspected.