People with diabetes require periodic urine tests, firstly, to determine the presence of sugar in the urine, and secondly, to exclude urinary tract infections, which are common in patients with diabetes and must be treated.
Urine testing is non-invasive and people often do it at home. However, health care providers may use a urine test if they cannot access a vein for blood testing or if a person has anxiety or fear of needles.
In this article, we'll look at the types of urine tests for diabetes and how to understand the results.
Types of analyzes
A urine test can detect a variety of substances, including glucose, ketones, protein, bacteria, and bilirubin.
Glucose
A urine test can measure levels of glucose, ketones, and other substances.
Typically, glucose is not present in the urine. However, when a person has diabetes, it can be detected in the urine. Some kidney diseases may also cause sugar to appear in the urine.
Pregnancy:
During pregnancy, almost half of women can detect glucose in their urine, even if they do not have diabetes.
A woman who experiences glucose in her urine during pregnancy should be evaluated for gestational diabetes.
This is a type of diabetes that occurs during pregnancy and usually goes away after delivery, but can have negative effects on the fetus, lead to complications during childbirth and a higher risk of developing type 2 diabetes later in life.
Glucosuria is the determination of glucose in urine.
Mechanism of formation of ketone bodies
The most informative when diagnosing disorders are three compounds of this group of substances: β-hydroxybutyrate, acetoacetic acid and acetone.
They are derivatives of acetyl-coenzyme A and are formed during catabolism in the liver. Their role is to provide energy to brain cells, as well as tissues and internal organs in emergency cases. These include increased physical activity, prolonged fasting, and dehydration. In this case, catabolism proceeds along the fat pathway with the formation of fat metabolism products - keto compounds. They are present in blood plasma, as well as in other fluid systems of the body, but in minimal concentrations. Their content in urine fluctuates, but daily excretion with stable functioning does not exceed 50 mg/l. It is impossible to detect such insignificant molarity in conventional analysis. If, however, the results indicate their presence, this indicates metabolic disorders.
Ketones
When a person has diabetes, the glucose in their blood cannot enter the body's cells and it remains in the blood. When this happens, cells don't have enough glucose for energy.
As a result, the body begins to break down fat to use it instead of energy. This produces toxic ketones. If ketone levels rise too high, they can cause your blood to become too acidic. In a person with diabetes, this can lead to diabetic ketoacidosis (DKA), which requires emergency treatment.
Ketones can also pass into the urine, so your doctor may use a urine test to detect DKA. People with diabetes can do a urine test at home if they begin to experience signs and symptoms of DKA.
Symptoms of DKA include:
- "fruity" or acetone odor on breath
- frequent urination
- thirst
- dry or red skin
- labored breathing
- confusion
- abdominal pain
- nausea and vomiting
- high blood sugar
- In severe cases, a person may experience: o loss of consciousness
- o to whom
Anyone who thinks they may have DKA should first have their blood sugar checked. If they exceed 240 milligrams per deciliter (mg/dL), the ADA recommends testing for ketones.
If ketone levels are high, seek medical attention immediately to prevent diabetic coma from developing. This applies to patients with type 1 diabetes.
The risk of DKA is higher when a person with diabetes gets sick with a cold or the flu. During this time, the ADA recommends that they check their ketone levels every 4 to 6 hours.
Knowing about self-testing for glucose and ketones can allow a person with diabetes to better manage their condition.
Why and under what conditions is it necessary to monitor ketone levels?
Deviation from the norm in the content of keto compounds is in itself an alarming sign. The normal value is 0.5 mmol/l. Excess indicates pathological conditions:
1. Exhaustion due to a strict diet with a significant or complete restriction of carbohydrate intake against the background of an excess of protein and fat foods. 2. Diabetes mellitus of the first or second type at various stages: decompensation, subcompensation, hyperosmolation. 3. Infectious diseases accompanied by high fever, as well as sudden changes in body temperature. This phenomenon is especially common in malaria. 4. Neoplasms in the organs of the endocrine system (adrenal glands, pancreas, thyroid glands). 5. Acute intestinal intoxication. 6. Severe injuries, extensive muscle damage, surgeries, brain injuries.
Under these conditions, monitoring the level of acetoacetic acid and β-hydroxybutyrate in urine is required. Analysis of changes is of particular importance for diabetics, since it can signal a worsening of the condition (for example, diabetic coma). In such situations, strict and constant monitoring is necessary, which can only be provided by express methods - test strips for ketones in urine.
Exceedances of standard indicators can also be detected in connection with harmless physiological characteristics. Thus, they are often detected in newborns up to a month old, and in babies against the background of overwork. Almost always - in pregnant and lactating women, as well as in elderly people over seventy years of age. Heavy physical activity also leads to a natural increase in these compounds.
What to expect
Sometimes a urine test is called a dipstick test because it involves dipping strips into the urine and reading the results using a color scale. Home tests are similar to this.
At the doctor's office
If the test strip changes color, ketones, glucose, or another substance may be present.
At the doctor's office, the health care professional will give you a clean, clear container and ask you to do the following:
- Urinate a little first before filling the container, as a mid-flow sample gives the most accurate reading
- fill three quarters of the container and secure the lid
- return the sample to the doctor or place it in a specific location
The doctor will dip the strip into the urine, which will change color according to the levels of different substances in the urine.
Your doctor will compare the strip to a color scale to determine the levels of glucose, ketones, and protein in your urine.
If your urine pH is high, it may indicate the presence of certain bacteria. However, the doctor may also need to send the sample to a laboratory for culture if they are testing for a UTI. This can reveal the type of bacteria present and provide insight into what treatment to administer.
Home testing
The procedure is slightly different if you are already diagnosed with diabetes and perform a urine test at home.
At home, you should follow the instructions in your test kit as they may vary. However, checking your urine ketone, protein, or glucose levels will likely require a colored strip and reference chart.
You should take the test in the morning before breakfast.
It is important to note that urine tests do not show whether blood glucose levels are too low. This may be important for people who are at risk of hypoglycemia (low blood glucose). Those using insulin or other medications may need to monitor their blood sugar for low levels.
Causes of the pathological condition
Ketoacidosis appears in the following cases:
- When a very low dose of insulin is administered.
- Eating large amounts of carbohydrates.
- Missing a dose of insulin.
- Excessive physical activity.
- Severe stress.
- Excessive alcohol consumption.
- The presence of an infectious disease.
- Using ecstasy or cocaine.
When blood sugar levels are significantly higher than normal, hyperglycemia occurs in the body and the number of ketone bodies increases.
results
The test results will determine the level of glucose, ketones and protein in the urine.
Glucose
Your doctor may suggest adjusting your treatment depending on the results.
If a urine test tests for glucose, the doctor will usually do a blood test for glucose and glycated hemoglobin (HbA1c) levels to determine whether the person has diabetes. In controversial cases, a glucose tolerance test (GTT) may be necessary to detect earlier carbohydrate metabolism disorders and help prevent diabetes.
If a person has high levels of glucose in their urine, it may be due to diabetes. If this is the case, they will also have high blood glucose levels (hyperglycemia).
In the short term, uncontrolled high blood sugar can lead to symptoms such as thirst, increased urination, and an increased risk of developing DKA. In the long term, this can lead to the development of micro- and macrovascular complications of diabetes mellitus - kidney damage, eye damage, the development of cardiovascular diseases - myocardial infarction, stroke.
If a person is diagnosed with type 1 diabetes, they will need insulin to control their blood sugar levels. Type 1 diabetes usually develops in childhood or adolescence, but can occur at any time. It may also appear quickly, within a few weeks.
Type 2 diabetes usually appears later in life and takes years to develop. A diagnosis of prediabetes will allow a person to make lifestyle changes that can slow or reverse the progression of the condition.
The ADA recommends screening for type 2 diabetes at age 45 or earlier if a person has risk factors such as obesity.
Ketones
A person with diabetes who detects ketones in their urine should see a doctor to prevent the problem from getting worse.
If ketone levels are high, they may require treatment in the hospital with insulin medications, electrolytes, and fluids.
Some low-carb diets can cause fat to be broken down and create ketones for fuel. A low-carb diet by itself does not cause ketoacidosis and is different from DKA.
However, a person with diabetes should discuss their diet plan with their doctor and seek advice about any dietary changes they wish to make.
Squirrels
Protein in the urine may be a sign of kidney disease.
A person with diabetes should talk to their doctor if they notice the following symptoms:
- swelling due to fluid retention
- sleep problems
- low appetite
- weakness
- difficulty focusing
People with kidney disease often do not notice any symptoms until later stages, when the kidneys no longer work effectively. This can lead to serious complications.
Your doctor may suggest regular urine protein screening as this can help identify kidney problems early, while there is still time to take preventative measures.
People are at higher risk of kidney disease if they have:
- certain genetic factors
- persistent high blood sugar
- high blood pressure
Addressing high glucose and blood pressure may reduce your risk.
Secondary acetone syndrome in the practice of a gastroenterologist
State Institution “Institute of Therapy named after L.T. Small Academy of Medical Sciences of Ukraine", Kharkov
In the practice of a gastroenterologist, diseases accompanied by the clinical picture of acetonemic syndrome are of particular relevance. The etiological structure of diseases, the clinical picture of which in a certain period is dominated by the phenomena of ketonemia and acetonuria, is extremely diverse. At the same time, at the prehospital stage, identifying the cause of ketonemia is difficult, and often impossible, since to establish the genesis of hyperproduction of ketone bodies it is necessary to use data from laboratory and instrumental research methods. Under these conditions, it is necessary to have a clear understanding of the possible causes of the development of secondary acetonemic syndrome, methods of correcting this emergency condition and preventing the development of ketoacidotic coma.
Brief biochemical information
Acetone (ketone) bodies include three compounds: acetoacetic acid (acetoacetate), β-hydroxybutyric acid (β-hydroxybutyrate) and acetone. Ketone bodies are metabolic products of acetyl-coenzyme A (CoA), which, in turn, is formed from the body’s own proteins, and, under conditions of food deficiency, from fats [6, 10, 11].
In conditions of energy deficiency in the body, restoration of energy reserves is possible due to the activation of gluconeogenesis or the synthesis of ketone bodies (ketogenesis). The processes of gluconeogenesis occur only in the presence of the essential amino acid alanine, which, in conditions of food deficiency, the body can only obtain through the destruction of its own proteins, while ketogenesis does not require the breakdown of proteins. Thus, ketone bodies play an important role in maintaining the body’s energy balance, and activation of ketogenesis is more expedient and optimal for the body under conditions of energy deficiency [6, 10, 11].
Ketone bodies are formed primarily in liver tissue. In case of excessive activation of the synthesis of ketone bodies, when ketogenesis increases to such an extent that the processes of ketolysis in tissues are not able to ensure the breakdown of the resulting ketone bodies, the latter begin to accumulate in the blood (ketonemia) and are filtered into the urine (ketonuria). Accumulating in the blood, keto acids suppress the secretion and activity of glucocorticoids, thereby preventing the destruction of the body’s structural proteins (proteolysis) [6, 10, 11].
Ketone bodies not only preserve the structural proteins of the body, inhibiting the secretion and action of glucagon, a powerful stimulator of gluconeogenesis, but also regulate and limit the intensity of ketogenesis through a feedback mechanism.
However, despite the compensatory-adaptive nature of ketogenesis, there are many clinical situations that can be accompanied by the development of ketosis and ketoacidosis. Long-term stimulation of ketogenesis or disruption of ketolysis processes lead to changes in the buffer capacity of the blood, and when ketone bodies are present in excessively high concentrations, to a decrease in blood pH and the occurrence of ketoacidosis [4–6, 8, 10, 11].
Initially, compensation for ketoacidosis is carried out through hyperventilation, which leads to hypocapnia and vasoconstriction, including of cerebral vessels. An excess of ketone bodies has a narcotic effect on the central nervous system, which is clinically manifested by lethargy, lethargy, up to loss of consciousness and the development of ketoacidotic coma.
Pathogenetic features of secondary ketosis
The most common cause of the development of ketosis, and subsequently ketonuria, is diabetes mellitus. In type 1 diabetes, on the one hand, there is a deficiency of insulin, on the other, an excess of counter-insular hormones (glucagon, catecholamines, cortisol). Under conditions of insulin deficiency, the processes of glycolysis, glycogenolysis, and lipolysis are activated. Massive lipolysis leads to a rapid increase in the concentration of free fatty acids in the blood, from which ketone acids are synthesized in the liver under the influence of glucagon. Inhibition of all anabolic processes under conditions of insulin deficiency leads to a slowdown in ketolysis processes and the development of ketoacidosis [6, 8, 11]. In type 2 diabetes mellitus, there is a relative insulin deficiency, therefore, in the case of decompensation of this disease, an increase in glycemia is observed, and the intensity of the processes of lipolysis and ketogenesis does not change significantly [6, 8].
Intensive formation of keto acids also occurs when so-called ketogenic amino acids (leucine, tyrosine, phenylalanine, isoleucine), some proteins and large amounts of fats are taken with food. Alkaline salts also exhibit a ketogenic effect, which is caused by disruption of the tricarboxylic acid cycle [6, 8, 11].
When maintaining a ketogenic diet, certain metabolic changes occur that provoke the synthesis of ketone bodies: on the 1st–2nd day of fasting, the processes of glycogenolysis in the liver and muscles are activated, on the 3rd–4th day, the production of keto acids increases significantly and reaches a maximum by the end of the 2nd week , in the 1st week the processes of gluconeogenesis intensify, and from the 2nd week the activity of gluconeogenesis decreases and the use of ketones by the brain increases. Thus, due to the predominant use of fats as an energy source, vital protein reserves are preserved [6, 8, 11].
Fasting, fever, and heavy muscular work lead to rapid consumption of carbohydrates and a reduction in glycogen reserves in the liver. With carbohydrate deficiency, the use of CoA in the tricarboxylic acid cycle is inhibited, which leads to the development of ketosis.
A similar mechanism of hyperproduction of ketone bodies is noted against the background of emotional stress, in which, due to activation of the sympathetic nervous system, the body’s carbohydrate reserves are depleted and ketosis develops. In addition, under stress, as a result of increased production of glucocorticoids, increased breakdown of proteins occurs and the formation of ketone bodies from ketogenic amino acids occurs [6, 8, 11].
Another reason for the overproduction of keto acids is chronic alcohol intoxication. The metabolism of ethanol in the liver under the influence of the enzyme alcohol dehydrogenase is accompanied by stimulation of the synthesis of keto acids, as well as inhibition of gluconeogenesis and the development of hypoglycemia, which, in turn, stimulates the processes of lipolysis, and therefore ketogenesis [9].
Stimulation of ketogenesis during food deficiency, fasting, and prolonged vomiting is a compensatory process during which the energy deficit is replenished by keto acids.
In case of toxicosis of pregnant women, with uncontrollable vomiting, severe dehydration occurs, which disrupts the natural process of self-regulation of the synthesis of ketoacids, which leads to the development of ketonemia and ketoacidosis [8].
The pathogenetic features of ketogenesis in thyrotoxicosis, excess of glucocorticoids, deficiency of gluconeogenesis enzymes are similar to the mechanisms of hyperproduction of keto acids discussed above.
Clinic
The clinical picture of secondary acetone syndrome includes the symptoms of ketosis itself, signs of the underlying disease against which ketosis developed, as well as manifestations of the condition that triggered the pathological process (stress, excessive physical activity, infection, etc.). A striking clinical manifestation of acetonemia is the picture of an acetonemic crisis, which can occur suddenly or after the appearance of its precursors - anorexia, lethargy or agitation, migraine-type headaches. Clinically, ketosis is manifested by repeated or uncontrollable vomiting, which renews when trying to take food or liquid, and the appearance of the smell of acetone in the exhaled air, vomit, and urine (from subtle to extremely intense). During an acetonemic crisis, the patient’s body temperature may increase to 37.5 - 38.5 ° C, and cramping pain in the abdomen may appear. Prolonged vomiting, loss of a significant amount of fluid and electrolytes lead to the development of dehydration and intoxication: upon objective examination, dry skin, tachypnea, tachycardia, muscle hypotension, and severe weakness are noted. When conducting a routine laboratory examination, the phenomena of relative leukocytosis with a shift of the formula to the left, an increase in the erythrocyte sedimentation rate, hypercholesterolemia, hypokalemia, and an increase in hematocrit are diagnosed.
Diagnostics
The content of ketone bodies in the blood serum of a healthy person varies from 34.4 to 430.5 µmol/l in terms of acetone, in urine - 20–54 mg during the day. Such concentrations of ketone bodies are not determined using routine methods in clinical practice, therefore it is generally accepted that ketone bodies are normally absent in the blood and urine [5, 12]. The vast majority of laboratory tests diagnosing ketonuria are based on reactions with acetoacetate and acetone; they do not react with β-hydroxybutyrate. Since the level of acetone in urine is insignificant compared to the level of acetoacetate, routine laboratory tests can be considered to detect almost only acetoacetic acid.
In clinical practice, predominantly qualitative and semi-quantitative samples are used to detect ketone bodies, which make it possible to quickly determine a pathological increase in the concentration of ketone bodies in the urine. According to these methods, the presence of acetoacetate in a clinical urine test can be measured from “one plus” (+) to “four pluses” (++++). Determination of ketone bodies in urine is an indirect indicator of ketonemia, since the severity of acetonuria in “+++” corresponds to an increase in the level of ketone bodies in the blood by 400 times, and “++++” – by 600 times [5, 12]. In addition, the result obtained reflects the level of ketones in the body 2-4 hours before the test, i.e. at the time of receipt of laboratory results, the true severity of ketosis may exceed the established values. The method for determining acetoacetate in urine has one more drawback: the result of the study depends on the amount of liquid taken by the patient (taking a large amount of liquid gives a false negative result, a small amount gives a false positive result). To determine the level of ketone bodies in urine on an outpatient basis, there are special diagnostic tests, the implementation of which does not require prior preparation and special medical knowledge - the appearance of a purple coloring of the “test strip” indicates the presence of acetonemia [4, 5, 12].
A more accurate method for determining ketone bodies is the indication of β-ketones in the blood. This version of the study is a more advanced technology, as it provides accurate quantitative data on the level of ketones, shows the level of β-ketones in the blood at the time of the study, and the result of the analysis does not depend on the drinking regime. The normal content of ketone bodies in the blood corresponds to a level of β-ketones of less than 0.5 mmol/l, an increased level of 0.5–1.0 mmol/l, ketoacidosis is diagnosed when the concentration of β-ketones is above 3 mmol/l [5, 12].
Differential diagnosis
Identification of ketosis in a patient requires a comprehensive differential diagnosis to clarify the cause of its occurrence. Secondary acetone syndrome can complicate the course of many diseases, including diabetes mellitus, insulinoma (hyperinsulinism), chronic alcoholism, Itsenko-Cushing's disease and syndrome, thyrotoxicosis, brain tumors in the sella region, hepatitis, toxicosis of pregnancy, Addison's disease, leukemia, hemolytic anemia, myotonic dystrophy, Huntington's chorea, traumatic brain injury, glycogenosis type I, fasting, febrile states, some infectious diseases, severe intoxications, and consumption of foods rich in fat (the so-called ketogenic diet) [6–11].
Diabetes.
A positive ketone test in most cases is diagnosed in decompensated type 1 diabetes mellitus, in rare cases - in patients with type 2 diabetes mellitus who are prone to ketosis. A characteristic feature of secondary acetonemic syndrome against the background of diabetes mellitus is the presence of glucosuria and a high level of glycemia. Features such as the acute, sudden onset of the disease in young people with the prevalence of polydipsia and polyuria in the clinical picture of the disease allow us to suspect the correct diagnosis at the prehospital stage.
Pregnancy.
The appearance of vomiting, salivation, the smell of acetone on the breath, food intolerance in women of childbearing age is an indication for diagnostic tests to determine toxicosis of early pregnancy. For this purpose, on an outpatient basis, a rapid test can be used to determine human chorionic gonadotropin in urine, and in specialized medical institutions, a gynecological examination, an enzyme-linked immunosorbent assay to determine the concentration of human chorionic gonadotropin in the blood, and an ultrasound examination of the pelvic organs can be used.
Thyrotoxicosis syndrome.
A persistent increase in the level of thyroid hormones and the resulting extreme activity of ketogenesis processes can lead to the development of ketosis and the appearance of acetonemic syndrome. The phenomena of thyrotoxicosis, as a rule, dominate the clinical picture of diseases such as diffuse toxic goiter, toxic thyroid adenoma, and autoimmune thyroiditis. More rare causes of thyrotoxicosis may be neoplastic formations: a pituitary tumor that secretes thyroid-stimulating hormone, a hormonally active tumor that synthesizes T3, T4 (ovarian teratoma, metastases of follicular thyroid cancer) or human chorionic gonadotropin (chorionepithelioma, hydatidiform mole). It is necessary to take into account that signs of thyrotoxicosis can occur against the background of an overdose of iodine-containing medications, dietary supplements, iodized salt, and thyroid medications. Uncontrolled intake of thyroxine for the purpose of weight loss can also cause the development of thyrotoxicosis. At the first stage of diagnosing secondary acetonemic syndrome, a screening determination of serum concentrations of thyroid-stimulating hormone, T3, T4, and ultrasound examination of the thyroid gland are carried out. Further research is carried out if indicated using specific research methods - enzyme immunoassay (human chorionic gonadotropin), radiography, computed tomography (CT) or magnetic resonance imaging (MRI).
Hepatitis.
The liver is the main and practically the only organ where ketone (acetone) bodies are formed from fatty acids. Almost any pathological process that affects the liver parenchyma leads to disruption of fat metabolism, intensification of ketogenesis processes and an increase in the concentration of ketone bodies in the blood. The development of acetonemic syndrome can accompany both acute damage to liver tissue and chronic hepatitis. The clinical picture of the disease at the time of identifying signs of ketosis varies from asymptomatic, latent to the presence of obvious, full-blown manifestations (hepato- and splenomegaly, signs of cholestatic, edematous-ascitic syndromes, protein-synthetic deficiency, etc.). Detection of altered laboratory parameters (levels of aminotransferases, bilirubin, alkaline phosphatase, γ-glutamyl transpeptidase, protein fractions, thymol test) and instrumental data (ultrasound examination of the abdominal organs) suggests a diagnosis of acute or chronic hepatitis. Further diagnostic search aimed at verifying the cause of liver tissue damage will allow us to establish the genesis of hepatitis and quickly stop the phenomena of ketonemia.
Insulinoma.
Stimulation of ketogenesis under conditions of hyperinsulinism is due to the activation of lipolysis processes against the background of prolonged hypoglycemia. Features of the clinical picture of the disease (the occurrence of an attack of hypoglycemia in the morning, when skipping the next meal, physical or mental stress), a positive hunger test (the development of an attack of hypoglycemia with a sharp decrease in blood glucose levels), high insulin levels, changes in the insulin/glucose ratio (more than 1), detection of a neoplasm in the pancreatic tissue during CT is in favor of insulinoma, which confirms the secondary genesis of acetonemic syndrome.
Itsenko–Cushing's disease and syndrome.
Secondary acetone syndrome may be the first clinical manifestation of hypercortisolism, when obvious “Cushingoid” signs of the disease have not yet formed. In this case, it is mandatory to determine the overproduction of glucocorticoids: an increase in the level of adrenocorticotropic hormone (ACTH), an increase in the concentration of cortisol in the blood or its metabolites in the urine (17-hydroxycorticosteroids in the urine or neutral 17-ketosteroids - dehydroepiandrosterone in the blood).
It should be noted that the determination of dehydroepiandrosterone in the blood replaces the determination of 17-ketosteroids in 24-hour urine. This eliminates errors associated with incomplete collection of a urine sample, impaired renal function, and the interference of many drugs with 17-ketosteroids. X-ray examination of the head in most cases is uninformative due to the presence of pituitary microadenomas. MRI of the head and CT scan of the abdominal organs in most cases make it possible to verify the diagnosis of Itsenko–Cushing’s disease/syndrome.
Pituitary adenoma.
The clinical picture of pituitary adenoma is polymorphic and is represented by different groups of symptoms. Tumors with pronounced endocrine symptoms can occur in Itsenko-Cushing's disease, acromegaly, thyrotoxicosis, which are more often diagnosed at the stage of microadenomas or small endosellar tumors. Prolactin-secreting pituitary adenomas can also cause the development of secondary acetone syndrome. Clinically, prolactinomas at the “endocrine” stage of development in women are manifested by menstrual irregularities, lactorrhea, infertility; in men there is a decrease in libido and potency, and gynecomastia. MRI of the brain occupies a leading position in the diagnosis of pituitary adenomas; CT and radiography of the skull can also be used, the information content of which is lower than that of the specified “gold” standard for diagnosing neoplasms in the area of the sella turcica.
Addison's disease.
In some cases, the manifestation of the disease may coincide with the development of acute adrenal insufficiency (adrenal crisis), the clinical picture of which includes manifestations of secondary acetonemic syndrome: abdominal pain, diarrhea, nausea, vomiting, smell of acetone from the mouth, acetonuria, in rare cases against the background of severe dehydration – the occurrence of clonic convulsions and the appearance of meningeal symptoms. Skin hyperpigmentation and a history of long-term depression may prompt the doctor to conduct a diagnostic search in the right direction.
In the diagnosis of Addison's disease, it is fundamental to determine the level of ACTH (increased concentration, sometimes 7-8 times), cortisol and its metabolites - 17-ketosteroids, 17-hydroxyketosteroids (decreased levels). Data from additional biochemical and instrumental studies (hyperkalemia, hyponatremia, hypoglycemia, changes in the size of the adrenal glands) are integral criteria in diagnosing the disease. Diagnosis of adrenal insufficiency requires further differentiation of the diagnosis and the exclusion of bilateral hemorrhage in the adrenal glands, embolism of the adrenal arteries or thrombosis of the adrenal veins (when conducting X-ray contrast studies), tuberculous lesions of the adrenal cortex, sarcoidosis, acquired immunodeficiency syndrome (AIDS).
Chronic alcoholism.
The alcoholic etiology of secondary acetonemic syndrome can be established on the basis of anamnesis regarding the amount, type and duration of alcohol consumption, the presence of markers (stigmas) of chronic alcoholism: characteristic appearance (puffy purplish-bluish face with a network of dilated capillaries in the area of the wings of the nose, cheeks , auricles, venous congestion of the eyeballs), tremor of the fingers, changes in behavior and emotional status (swaggering, familiarity, depression, emotional instability), Dupuytren's contracture, signs of hypogonadism. Identification of the companions of chronic alcoholism - concomitant diseases of internal organs and the nervous system, as well as characteristic laboratory data (pronounced activity of transaminases, β-glutamyl transpeptidase and alkaline phosphatase) can confirm the correctness of the diagnosis of chronic alcoholism and explain the cause of overproduction of ketone bodies.
Traumatic brain injury.
Mechanical damage to the integrity of the skull and intracranial formations (brain, blood vessels, meninges) may be accompanied by a sudden increase in ketogenesis and the appearance of ketone bodies in the urine. The presence in the medical history of information about a traffic accident, a fall, an industrial, sports or household injury, characteristic changes in the neurological status, a violation of the integrity of the bone structures of the brain, the presence of meningeal symptoms, a change in the level of consciousness make it possible to quickly establish the genesis of ketosis.
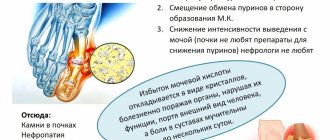
Ketogenic diet (Atkins diet).
The desire to have an ideal body weight forces many patients to follow various diets, excluding carbohydrates from the daily diet and additionally saturating it with fats. Lack of information about the side effects of the chosen diet leads to the appearance of clinical manifestations of ketosis. The accumulation of ketone bodies helps reduce feelings of hunger and thirst, promotes increased excretion of calcium and phosphorus, and the accumulation of uric acid. Thus, the appearance of signs of acetonemia against the background of rapid weight loss in the absence of any other pathological changes may be due to the predominance of fats in the patient’s daily diet. A correctly collected anamnesis and establishment of the fact of adherence to a ketogenic diet do not exclude the need to conduct a detailed laboratory and instrumental examination in order to diagnose possible concomitant pathology that provokes the intensity of ketogenesis.
Huntington's chorea, myotonic dystrophy.
The course of these hereditary neurodegenerative diseases may be accompanied by destruction of pancreatic β-cells and the development of secondary ketonemia and acetonuria. The predominance of muscle tone disorders, hyperkinesis, and psychopathic disorders in the clinical picture is an indication for consultation with a neurologist to exclude a possible genetic cause of nervous system pathology.
Glycogenosis type 1 (Gierke's disease).
As a rule, Gierke's disease is diagnosed in early childhood. However, with a mild course of glycogenosis, the patient’s condition somewhat stabilizes during puberty, and with further progression of the disease, secondary acetonemic syndrome may develop.
The presence of hypoglycemia, hyperlactic acidemia, hyperlipemia, ketosis phenomena against the background of hepatomegaly and nephromegaly may indicate a hereditary pathology caused by a lack of enzymes involved in glycogen metabolism. Carrying out a biopsy of the liver and muscles, followed by histochemical determination of glycogen in tissues and determination of the activity of the enzyme glucose-6-phosphatase, is a fundamental method in confirming the diagnosis of Gierke's disease.
Hereditary metabolic disorders.
Clinical manifestations of secondary acetonemic syndrome can be observed with hereditary metabolic disorders - mitochondrial pathology, organic aminoacidurias. The chronic intermittent form of organic aciduria can manifest itself at any age in the form of attacks of “ketotic hypoglycemia”, occurring with transient neurological disorders expressed to varying degrees. Aminoacidopathies are diagnosed by analyzing amino acid concentrations in serum or urine using gas chromatography and mass spectrometry. During a metabolic crisis provoked by the consumption of “banquet food” or an infectious onset, examination of the patient may reveal ketonemia, ketonuria, hypoglycemia, and possibly the presence of hyperglycinemia, hyperlactatemia, hypertriglyceridemia, and a moderate increase in the level of ammonia in the blood. In some cases, the course of celiac enteropathy can also complicate secondary acetonemic syndrome.
Treatment
The most effective correction of secondary acetonemic syndrome is possible only with combination therapy aimed at leveling the manifestations of the underlying disease, which led to overproduction of ketone bodies, and symptomatic treatment of ketosis. However, etiological therapy in most cases is delayed due to laboratory and instrumental examination of the patient, so emergency treatment of acetone syndrome begins with symptomatic treatment (non-drug and pharmacological).
A necessary condition for the treatment of acetonemic syndrome is the correction of the diet in accordance with the principle of aketogenicity (lack of fats, purine bases, extractives). Patients should consume a significant amount of fluid with a predominance of alkaline drinks (non-carbonated low-mineralized alkaline water, lemon drinks, green tea, non-concentrated dried fruit compote) [4]. Nutritionists advise excluding from the diet concentrated meat, bone, fish and mushroom broths, meat of young animals and birds, fatty meats, offal, sour cream and fermented baked milk, tomatoes, eggplants, boiled cauliflower, legumes, chocolate, oranges, drinks containing caffeine, cold and carbonated drinks, as well as modified foods (freeze-dried and transgenic). The diet of a patient with ketosis should be dominated by buckwheat, oatmeal, semolina porridge cooked in water, vegetable (cereal) soup, mashed potatoes, baked apples, biscuits, milk and dairy products [4].
Drug therapy is aimed at inhibiting ketogenesis and accelerating the elimination of ketone bodies. Replenishment of pathological fluid losses is carried out using oral rehydration with electrolyte solutions (Rehydron, Oralite), as well as infusion therapy. In order to quickly restore fluid deficiency, replenish circulating blood volume, and improve microcirculation, it is recommended to use Reosorbilact
at the rate of 10 ml/kg body weight [3].
Sorbitol, which is part of the drug, is quickly included in metabolism, utilized in the liver and accumulates in hepatocytes in the form of glycogen. Renewal of glycogen reserves in the liver inhibits the processes of ketogenesis and helps reduce the severity of ketonemia. Another component of Reosorbilact
, sodium lactate, helps correct metabolic acidosis by replenishing the bicarbonate buffer and increasing the alkaline reserve of the blood.
A 5–10% glucose solution has antiketogenic properties, the administration of which must be combined with the addition of the required amount of insulin, based on the glycemic profile, as well as Ringer’s solution.
A relatively new drug that has the most pronounced anti-ketogenic properties compared to other carbohydrates (glucose, sugar alcohols) is the drug xylate [2], the two main components of which are the pentahydric alcohol xylitol and sodium acetate. The metabolism of xylitol is independent of insulin levels and the activity of the enzyme fructose-1,6-biphosphatase. Xylitol inhibits the processes of ketogenesis due to its rapid absorption in the liver and restoration of glycogen and energy reserves. Correction of metabolic acidosis due to the presence of sodium acetate in the preparation occurs more slowly compared to sodium bicarbonate solutions and is not accompanied by sharp fluctuations in blood pH. In the literature there are various recommendations regarding the dosage of xylate: from 10 to 20 ml/kg body weight per day [1, 2].
5-HT3 receptor antagonists and 5-HT1D receptor agonists can be used as abortive therapy for secondary acetone crisis and to inhibit the vomiting center. For this purpose, intravenous administration of granisetron at a rate of 10 mg/kg or ondasetron at a dose of 0.3–0.4 mg/kg every 4–6 hours, as well as sumatriptan up to 20 mg per day, is used.
In order to normalize liver function and indirectly inhibit ketogenesis, it is recommended to use hepatoprotectors (ursodeoxycholic acid, a combination of arginine and betaine) in standard dosages.
Many authors recommend the use of pancreatic enzymes and cofactors of carbohydrate metabolism (cocarboxylase, thiamine, pyrodoxine) to increase tolerance to enteral nutrition and normalize the absorption of nutrients.
Of the possible detoxification methods based on natural physiological processes, gastric and intestinal lavage can be used to correct secondary acetone syndrome in clinical practice. The use of sodium bicarbonate solutions for detoxification purposes in patients with acetone syndrome is limited due to the lack of influence of this drug on the intensity of ketogenesis, as well as the high likelihood of developing metabolic alkalosis and hypernatremia.
Extracorporeal detoxification methods may be indicated to clarify the genesis of secondary acetonemic syndrome, namely, with withdrawal syndrome, chronic hepatitis and cirrhosis of the liver, pathology of the thyroid gland, myasthenic syndromes, toxicosis of pregnancy, and decompensated diabetes mellitus.
Understanding the mechanisms of development of secondary acetonemic syndrome and identifying the most likely causes of the formation of ketosis will make it possible to determine the genesis of the disease, prevent the development of acetonemic crisis and ketoacidotic coma, normalize the patient’s condition and prevent relapse of overproduction of ketone bodies.
Summary
If a person detects ketones in their urine, they should contact their doctor for advice. If a doctor finds high levels of glucose, ketones, or protein in a person's urine, they may order further tests.
Depending on the results, additional testing may be required.
Often, lifestyle choices such as a healthy diet and exercise are key to reducing the risk of further complications. However, the doctor may also prescribe treatment or recommend hospitalization in some cases.
Effective ways to normalize metabolism
When ketoacidosis or ketonuria is detected, it is necessary to identify, eliminate the cause, and take measures:
1. Diabetics need to normalize glucose levels. 2. In case of intoxication and food poisoning, absorbents, enemas that cleanse the intestines, as well as salt solutions that restore water balance (Rehydron, Orsol) are indicated. 3. In case of severe exhaustion, an intravenous infusion of glucose will be required. 4. If the cause is an infectious disease and fever, you need to use drugs against the pathogen, and also stabilize the temperature.
General recommendations are to avoid overload and dehydration. In the first case, a special diet will help, in the second, plenty of fluid intake.
Source: Pharmindex.ru for the newspaper "Pharmacy"
Mechanism of development of diabetic ketoacidosis
If there is a lack of insulin, the body cannot convert glucose into the energy it needs. Fat consumption begins. When they are used, ketone bodies accumulate in the body, the content of which rapidly increases. Ketone bodies cannot enter the blood due to the lack of insulin. They pass through the kidneys into the urine. A high content of by-products quickly poisons the body and leads to complications.
A patient who knows about the causes, symptoms, methods of prevention and treatment can avoid the occurrence of diabetic ketoacidosis.
What urine test is needed for cystitis?
If cystitis is suspected, you must first undergo a general urinalysis (UCA). The results of OAM in cystitis will reveal an increased content of leukocytes, bacteria, and an increased content of erythrocytes and protein may occur.
Additionally, the attending physician may recommend conducting bacterial culture of urine to determine antibiotic sensitivity to identified pathogenic microorganisms, PCR diagnostics for sexually transmitted diseases, and a number of studies for the diagnosis of viral infections (since cystitis is not always caused by bacteria).
From instrumental studies, the doctor can refer the patient to an ultrasound of the kidneys, CT/MRI of the pelvis to exclude tumors and stones in the urinary system, kidney and prostate diseases in men.
Prevention of exacerbations of cystitis
- Regularly perform thorough toileting of the external genitalia
- Use barrier methods of contraception
- Timely treatment of gynecological and urological diseases
- Urinate immediately after intercourse
How to properly collect a urine test for cystitis
The average portion of urine during the first morning urination is collected in a sterile container (the first and last portions are flushed into the toilet).
Urine collection is possible at any time during the day with prior agreement with the attending physician.
When collecting urine, it is advisable not to touch the container to your body.
Before urinating, women need to spread their labia with their fingers so that foreign impurities do not get into the urine from the skin of the external genitalia.
The volume of urine for testing should be ¾ of the volume of the container. The minimum volume of urine for testing is 30 ml.
It is advisable to deliver the container with urine to the medical office within 2 hours after collecting the biomaterial.