There are a number of diseases of the vaginal mucosa. One of them is atrophic colpitis. It is characterized by an inflammatory course, the presence of degenerative changes in different parts of the reproductive system and frequent relapses.
Most often, various forms of atrophic colpitis are diagnosed in women within several years after menopause. However, the incidence is not limited to this age group. Due to various hormonal changes, previous sexually transmitted infections and other factors, the vaginal mucosa can become inflamed in young girls.
Causes of atrophic colpitis
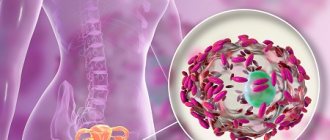
Every woman has a certain vaginal microflora. Normally, the majority of it consists of the so-called Doderlein bacilli - symbiotic bacteria that produce lactic acid. This substance inhibits the proliferation of pathogenic microorganisms.
But the population of these symbionts can sharply decrease due to various reasons. Most often these are hormonal changes, decreased immunity, poor hygiene of intimate places, allergic reactions to contraceptives and medications, as well as other factors.
Atrophic colpitis in women occurs due to the proliferation of different types of pathogenic microflora:
- fungi of the genus Candida;
- genital herpes virus;
- mycoplasma, ureaplasma;
- streptococci and staphylococci;
- coli;
- a group of opportunistic microbes (Proteus, Haemophilus influenzae vaginalis, Escherichia).
But sometimes the disease can develop in the opposite scenario - first, due to mechanical damage or exposure to various agents, inflammation appears, and then infectious agents penetrate the mucosa. To diagnose the pathogen, the doctor may prescribe a smear test using the PCR method (costs from 300 rubles for 1 indicator), an analysis to determine serological markers (this blood test for antibodies costs from 750 rubles). A microbiological study is also possible, its price starts from 1,600 rubles.
Content:
- Risks for the female body
- Causes of the disease
- Manifestation of the disease
- Diagnostics
- Treatment of the disease
Risks for the female body
Inflammation of the vaginal mucosa, represented by stratified squamous epithelium, is called colpitis (vaginitis). Colpitis can be of an infectious nature, and the so-called atrophic one is caused by a non-inflammatory nature. Since female sex hormones influence the state of the epithelium, when their concentration in the body decreases, the vaginal mucosa undergoes dystrophic changes. The disease develops after menopause and is included in the concept of menopause syndrome, often combined with kraurosis (the same atrophic process of the external genitalia). Long-term atrophic changes in the mucosa can progress over time, and they can be joined by secondary bacterial or fungal infection. If you do not take any action, it will be quite difficult to cure the disease. Preventing the development of a disease is always easier than treating the process once it has started.
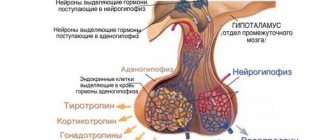
Causes of the disease
The main reason for the development of mucosal atrophy is an insufficient amount of estrogen in the body. Various factors can lead to this, primarily physiological menopause. Removing the ovaries in young women also leads to the development of artificial menopause and a decrease in hormone levels. This situation may arise in the postpartum period due to the slow restoration of hormonal status in lactating women. Some diseases and drug interventions can also cause atrophic colpitis: primary disorders of the endocrine regulation of the ovaries, radiation or radionuclide therapy, chemotherapy for cancer, neurotic disorders (hysterical and anxiety-phobic neuroses often lead to gynecological problems), diseases of the endocrine organs and many others . The renewal of the epithelium is disrupted, the number of cells decreases, and their sizes also change downward. It undergoes changes in pH, which is very important for maintaining certain conditions for the survival of the necessary microflora. Lactobacilli die at high pH levels, opportunistic bacteria begin to actively multiply and cause an inflammatory reaction in certain areas. epithelium. Predisposing factors for secondary infection are non-compliance with hygiene rules, weakening of the body's defenses due to a chronic disease, frequent sexual intercourse (the mucous membrane becomes very vulnerable, regeneration processes are disrupted), wearing tight underwear, the use of intravaginal drugs and irritants, chronic inflammatory phenomena in the pelvic organs.
Manifestation of the disease
The manifestations of colpitis are pronounced and cause significant discomfort to the woman. First of all, there are sensations of tightness and dryness in the vagina, burning, and there may be severe itching when bacterial inflammation is associated. Due to a decrease in the secretion of fluid that moisturizes the internal genital tract, there may be severe pain during sexual intercourse. This symptom is called dyspareunia. Bloody discharge after sexual intercourse is also not uncommon; it is caused by trauma to the thinned, easily vulnerable mucous membrane. Discharge in an uncomplicated process is normal - it is transparent and presented in small quantities. When infected, leucorrhoea (discharge) can take on any character, which will be determined by the specifics of the pathogen. In this case, discomfort in the vaginal area increases, severe itching and burning appear.
Diagnostics
Diagnosis and treatment of atrophic colpitis is carried out by a gynecologist. there is no need to conduct numerous examinations. A conversation with the patient can already provide the necessary information - characteristic symptoms, a statement of menopause or other conditions that are accompanied by a decrease in estrogen levels. When examined in the speculum, changes characteristic of this disease can be noted - the vaginal mucosa is pale, thinned, with possible hemorrhages and injured areas. The symptom of contact bleeding can be pronounced - touch causes capillary bleeding. If during the examination the doctor identifies pathological leucorrhoea, then a smear is taken for microflora. A study of pH levels indirectly indicates changes in microflora and the presence of inflammation. Colposcopy and colpocytology are also important methods. Depending on the stage of the menstrual cycle and the level of hormones in the body, the composition and other qualities of mucus change. These methods allow us to judge the level of hormones in the body. Other methods are used according to indications.
Treatment of the disease
The main treatment method is drug replacement therapy. Synthetic drugs and more gentle herbal remedies are used systematically. Estrogens can also be used topically to enhance the effect. If a woman has contraindications to the administration of estrogens, then solutions of plants and herbs with an anti-inflammatory effect are used locally.
When is it necessary to contact a specialist?
The symptoms of atrophic colpitis appear quite clearly, causing significant discomfort, pain and general deterioration of the condition. Therefore, the disease almost never goes away without a trace.
The main symptoms of the disease include:
- purulent and mucous discharge, periodically with blood impurities;
- redness and itching of the external genital organs, as well as the mucous membrane;
- pain, discomfort during urination and sexual intercourse;
- impaired performance, feeling of drowsiness and weakness.
If at least two of the listed manifestations occur, you should urgently contact the specialists of the Academy of Health. Our doctor will conduct a visual examination to assess the degree of development of the inflammatory process, and will also take various samples for laboratory tests. Further diagnostics will determine the type of pathogen and prescribe appropriate treatment. Also, the type of disease determines further preventive measures.
Diagnosis of the disease
At the initial appointment, the specialist will collect anamnesis, ask the necessary questions and listen to complaints. He can determine the presence of an inflammatory process through a routine examination. “Senile” colpitis has quite typical signs: pallor of the mucous membrane, the presence of microcracks, pinpoint bleeding, and sanguineous discharge. The presence of purulent inclusions, redness of the vaginal walls and their swelling indirectly indicate the presence of a secondary infection. White plaque and curd-like discharge may indicate the presence of candidiasis. To confirm or refute the assumptions, the doctor will take a smear, the material is sent to the laboratory for cytology and microscopic examination. You will also need to assess the acid balance of the vagina and perform colposcopy: examination of the vaginal surface using optical magnification.
Based on the results obtained, the doctor develops an individual treatment regimen and correction of the condition.
What methods help clarify the diagnosis?
To diagnose this pathology, in addition to examining the vagina, a number of methods are used. To accurately determine the pathogen, methods of sowing discharge from the vagina, urethra and cervical canals are used. An important stage of the examination is microscopy of vaginal smears. Colposcopy is used - examination of the mucous membrane through a lens system. By enlarging the image several times, the doctor will be able to identify mild signs of inflammation and dysplasia, which is important in the early diagnosis of tumors. Atrophy of the integumentary epithelium of the cervix after 40 years is a normal colposcopic picture.
A cytological examination is carried out. It is based on determining the morphology of vaginal cells. During menopause, an atrophic type of smear is often found. It implies the presence of epithelial cells from its various layers with signs of atrophy. The results of the cytogram may also contain such a concept as pseudokeratosis. Inflammatory infiltration indicates the activity of the process. These types of smears do not occur in women of reproductive age, but can be detected in those under 16 and over 55 years of age.
Back to contents
Danger
If treatment is prescribed correctly, there is no threat to the woman’s health. But self-medication, as well as complete ignorance of the symptoms of the disease, can cause inflammation of the fallopian tubes, uterus, cervix, and ovaries. This negatively affects reproductive health, leading to recurrent miscarriage or infertility.
The presence of dangerous complications of colpitis is indicated by:
- disruptions of the menstrual cycle;
- amenorrhea;
- difficulties associated with conceiving a child;
- severe pain in the lower abdomen;
- vaginal bleeding.
Treatment of colpitis
Proper treatment should include not only eliminating disturbing symptoms, but also getting rid of the cause of the pathology. The latter falls within the purview of etiotropic therapy. It is based on the use of antifungal, antibacterial or antiviral drugs.
To treat nonspecific colpitis, combination medications are prescribed to kill several types of infections. Local therapy consists of the external use of various antiseptics and other medications in the form of douching or moistened vaginal tampons.
Do not forget that if vaginitis is associated with the acquisition of an infectious agent through sexual contact with an infected partner, both partners must be treated at the same time.
It is recommended to abstain from sexual intercourse during therapy until complete recovery.
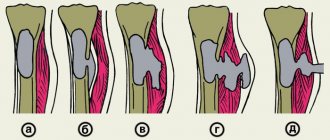
Classification of acute vaginitis
Acute vaginitis is of the following types:
- specific, caused by STDs and tuberculosis. With a combined infection, there are several types of pathogens in the vagina, for example, Trichomonas and gonococcus. Therefore, the ICD-10 classification indicates that code N76.0 includes acute colpitis without further specification (NOS);
- nonspecific, caused by the activation of opportunistic flora: staphylococcus, Proteus, Escherichia coli and Pseudomonas aeruginosa, fungi of the genus Candida. This form of colpitis is caused by a violation of the vaginal microflora;
- non-infectious, occurring due to allergies, sexual intercourse without sufficient hydration, irritation of the mucous membrane with latex, tampons, douching solutions.
Prevention
To prevent colpitis, a number of rules should be followed:
● Regular examinations by a gynecologist to identify disorders in the initial stages of their occurrence.
● Caring for the vaginal lining, including maintaining personal hygiene, frequent changes of underwear, and proper use of toilet paper.
● Taking antibacterial agents exclusively as prescribed by a doctor and, if necessary, combining them with taking medications that will maintain the microflora of the mucous membrane in a normal state.
● Strengthening the immune system.
Why is colpitis dangerous?
Colpitis is not a dangerous disease if treatment is started in a timely manner. If a woman neglects medical care, the disease can become chronic, which will significantly worsen the quality of life.
If vaginitis is not treated correctly, it can develop into endometritis, urethritis or cervical erosion. Also, bleeding microcracks on the walls of the vagina serve as open gates for the acquisition of new pathogenic microorganisms, complicating the treatment process.