Unfortunately, there are still diseases that in a matter of hours bring a seemingly completely healthy person to a critical condition and have an extremely unfavorable prognosis. One of these diseases is Lyell's syndrome (L51.2 according to ICD-10).
A scandalous case of death from this pathology was widely discussed in the media - the death in July 2003 of a journalist, deputy of the State Duma of the third convocation, Yuri Shchekochikhin.
Witnesses noted an inexplicable sharp deterioration in his condition: “in two weeks he turned into a very old man, his hair fell out in clumps, the skin came off his body, almost all of it, one by one the internal organs failed” (“Novaya Gazeta”, issue No. 20 of March 24, 2008 .).
In connection with the death of the deputy, a criminal case was opened under Article 105 of the Criminal Code of the Russian Federation, Part 1 - “Murder”. Relatives and the press, which caught up with the hype, were talking about poisoning, in particular with thallium. The relevant examinations were carried out for seven months, and the deputy’s body was exhumed. Only by March 2004 were the circumstances of the rapid deterioration of Shchekochikhin’s condition established. Diagnosis and cause of death: Lyell's syndrome, acute cardiovascular failure.
Causes of Lyell's syndrome
Regarding the causes of the development of Lyell's syndrome in modern dermatology, 4 variants of the disease are identified.
First option
The first option represents an allergenic reaction that occurs as a response to an infectious process. Often this reaction is explained by the presence of Staphylococcus aureus, which belongs to group 2. The first option is observed in children and is distinguished by its severe course.
Second option
The second option is Lyell's syndrome, observed due to the use of drugs (such as antibiotics, anti-inflammatory, sulfonamides, anti-inflammatory, anti-inflammatory, anti-tuberculosis). Very often, the formation of the syndrome is explained by the use of several drugs at once, including sulfonamide. Recently, cases of the spread of Lyell's syndrome have been known when using dietary supplements, as well as vitamins and substances intended for radiography.
Third option
Another, third variant of Lyell's syndrome includes idiopathic cases of the disease, the cause of which has not yet been clarified.
Fourth option
The fourth variant of Lyell's syndrome is caused by various mixed causes (medicinal and infectious), and usually develops during the treatment of any infectious disease.
Pathogenesis
Basically, Lyell's disease develops in people prone to allergic manifestations. Most often it manifests itself against the background of the use of medications, but in some cases the cause of the disease cannot be established. The essence of pathogenesis is the mass death of basal keratinocytes of the skin and mucosal epithelium. It is provoked by Fas-induced and perforin/granzyme-mediated cell apoptosis. Cells die due to immune-mediated inflammation, which is determined by cytotoxic T cells (CD8+ T lymphocytes). Most often, the syndrome develops after the use of phenytonin , carbamazepine , allopurinol , phenibutazole , chlormazanon , penicillins , sulfonamides .
Mechanism of development of Lyell's syndrome
A significant role in the development of Lyell's syndrome is assigned to the genetic component, which is caused by a predisposition to reactions of an allergic nature. The anamnesis of most patients indicates various allergic diseases, such as:
- hay fever;
- eczema;
- allergic rhinitis;
- allergic contact dermatitis;
- bronchial asthma.
In people suffering from this disease, the process of neutralizing various types of toxic metabolic products is disrupted; the administered medicinal components and the protein contained in the epidermis react. This newly formed substance is called an antigen characteristic of Lyell's syndrome. That is, the body’s immune response is directed not only to the injected substance, but also to the patient’s dermis. This process is very similar to the reaction in which transplant rejection occurs. It is known that with such a reaction, the immune system mistakes the patient’s skin itself for the graft.
The basis of Lyell's syndrome is the Schwartzman-Sanarelli phenomenon. This phenomenon is an immunological reaction that leads to disruptions in the regulation of the possibility of protein breakdown, as well as to the accumulation of products of this breakdown in the human body. The result is toxic damage to human organs and organ systems. The latter leads to disruption of the functioning of organs that are responsible for the neutralization and elimination of toxins, which means that the process is aggravated by intoxication and entails obvious changes in the water-salt balance (as well as electrolyte). Such processes lead to a deterioration in the patient's condition in the case of Lyell's syndrome. They can cause death.
Epidemiology
Since the 70s, medicine has kept an annual record of the prevalence of Lyell's syndrome. According to various authors, rates range from 0.4–1.3 cases per 1 million population per year. Mortality rates range from 20–60% of the number of cases, depending on the state of the region's health care system. Thus, the number of deaths from this pathology throughout the world per year is in the thousands. Among immediate allergic reactions, Lyell's syndrome is second only to anaphylactic shock in terms of mortality. In the general structure of drug allergies, the share of Lyell's syndrome is 0.3%. Women are more often affected: the ratio to male patients is 1.5:1. There was no direct relationship between the risk of the disease and age. Patients who have previously had Lyell's syndrome, especially in childhood, are considered a risk group.
The most common form of the syndrome is medicinal, up to 80% of all cases. After medicinal, the second most common cause is malignant neoplasms (especially lymphomas). The frequency of idiopathic cases of the syndrome is 5–10%.
In children, Lyell's syndrome more often - up to 60% of cases - has an infectious etiology. A special risk group for the manifestation of the disease among children is those who suffered from acute respiratory viral infections at an early age and underwent a course of treatment with NSAIDs in connection with this.
Symptoms of Lyell's syndrome
Typically, Lyell's syndrome begins unexpectedly with a suddenly elevated temperature (up to 39-40°C). Also, in just a few hours, slight swelling and erythematous spots, which are characterized by pain, appear on the patient’s skin, namely on the skin of the torso, oral mucosa, genitals, limbs and face. Such spots can be of very different sizes. Sometimes they merge.
After 12 hours, the epidermis begins to peel off on healthy skin. At this point, thin-walled blisters of a sluggish nature and irregular shape appear. Their sizes reach the size of a hazelnut (up to 15 cm in diameter). After opening such bubbles, large erosions usually remain, which along their periphery are covered with fragments of the remains of bubbles. Erosions are usually surrounded by edematous skin, which can also be hyperemic. Erosions release exudate, characterized by its abundant serous-bloody content, which is the cause of immediate dehydration of a person.
In the case of Lyell's syndrome, the Nikolsky symptom inherent in pemphigus is noted, that is, the characteristic peeling of the epidermis due to little effect on the surface of the skin. Due to the detachment of the epidermis, those areas subjected to compression, as well as friction (or maceration), form erosions, without the formation of blisters.
Diet
Hypoallergenic diet
- Efficacy: therapeutic effect after 21-40 days
- Timing: constantly
- Cost of products: 1300-1400 rubles. in Week
If the patient eats independently, he should adhere to a strict hypoallergenic diet. You need to follow such a nutritional system during the recovery stage.
You need to exclude the following foods from your diet:
- eggs;
- chocolate;
- nuts;
- seafood, fish;
- cocoa, coffee;
- red fruits and berries;
- spicy, fried, smoked food;
- all types of citrus fruits.
It is also important to minimize the amount of baked goods, baked goods, confectionery products, milk, and sauces.
Useful products during the period of treatment and recovery are:
- low-fat dairy products;
- rice, buckwheat, oatmeal;
- vegetable soups;
- herbal teas.
Skin manifestations
As this disease progresses, the entire skin quickly becomes red and the person feels a characteristic pain when touched. The appearance of such skin is very similar to a 2nd or 3rd degree burn. There is also a characteristic symptom when, when touched, the skin quickly wrinkles and moves to the side. Sometimes manifestations of Lyell's syndrome are accompanied by the appearance of small petechial rashes throughout the body. The main symptom of the disease in children is considered to be conjunctivitis, which is combined with infectious lesions of the dermis by a special staphylococcal flora.
Symptoms
Previously, Lyell's syndrome with an area of skin affected less than 10% was called Stevens-Johnson syndrome. It is currently considered a milder form of toxic epidermal necrolysis with a fatality rate of less than 5%. Both of these syndromes are characterized by involvement of the mucous membranes in the process (in more than 90% of cases of the disease). Forms with an area of skin damage from 10 to 30% are classified as intermediate.
Manifestation of Lyell's syndrome
In the clinical course of the disease, 3 periods are conventionally distinguished:
- Prodromal, which develops in the first 2 weeks after starting to take the corresponding drug (usually in the first 2-3 days). Sometimes this period is several hours and even (rarely) 1 hour.
- Critical, or acute.
- Recovery.
Prodromal period
Usually the disease begins with a rapid increase in body temperature to 38-41°. The general condition suddenly becomes severe, severe chills, general weakness and malaise, headache, pain in the joints and muscles, lumbar region, pain when swallowing, enlarged peripheral lymph nodes, loss of appetite, and slight nasal congestion appear. Symptoms of the prodromal period can occur 1-2 days before skin manifestations, which often leads to erroneous diagnosis of influenza or respiratory viral infection and too late discontinuation of the drug that caused acute epidermal necrolysis.
In addition to these signs, an inflammatory process of the mucous membrane of the oral cavity, nose, eyelids, conjunctiva, and genitals is often noted. Often the patient complains of a feeling of moderate pain, burning and itching of the skin.
Acute period
It is characterized by the progression of lesions of the mucous membranes and skin, as well as dysfunction of internal organs and systems - changes in the blood count and metabolic disorders appear. In the critical period, 3 stages are also conventionally distinguished:
Erythematous
Resembles eruptive elements on the skin and mucous membranes of exudative erythema multiforme. The rash is represented by erythematous spots, roseola, papules, and pustules. A papular-erythematous rash is typical of the onset of the disease and is located symmetrically, appearing first on the face, then on the limbs and trunk. The rash is profuse, disseminated. Most often, it takes the form of deep red, swollen spots that enlarge and merge with each other, forming large lesions.
Bullous
After 2-3 days, large, irregularly shaped, thin-walled blisters with a brownish tint and a flabby covering form in the center of the erythematous spots. Bubbles tend to merge. When pressed, their area can increase significantly, reaching even the area of the palmar surface of the hand (Asbo-Hansen symptom). This stage is characterized by a burning sensation and itching of the skin, increased and impaired sensitivity of not only the affected, but also healthy areas of the body. In addition, there is such severe pain in the skin that even a light touch of the sheet causes it. Dehydration develops, accompanied by excruciating thirst.
Related articles: Bullous dermatitis
Desquamation
It is characterized by slight rupture of blisters with exposure of extensive erosive surfaces of cyanotic-red color with serous-hemorrhagic discharge. Erosions are sharply painful when touched and bleed easily. Very quickly, almost the entire skin surface takes on the appearance of a II-III degree burn. At this stage, sharply positive Nikolsky’s symptom and its variety of Asbo-Hansen’s symptom are noted, as well as symptoms of “wet underwear” (under the influence of a finger, the epidermal layer easily slides, shifts and wrinkles), and “socks and gloves”, when peeled off on the fingers and feet the epidermis retains their shape.
Nikolsky's sign consists of peeling of the epidermis in an area of apparently normal skin when sliding a finger over it with slight pressure, as well as peeling of the epidermis near the bladder when pulling on pieces of the covering of the bladder. In especially severe cases, detachment of the entire epidermis on the entire skin surface of the body is observed during finger rubbing. A petechial rash may appear.
More than 90% of patients have erosions on the mucous membranes. Multiple painful and easily bleeding erosions appear on the lips and oral mucosa. On the lips they are covered with bloody crusts and cracks, which makes eating much more difficult. Often there is damage to the mucous membranes of the eyes with the formation of erosive blepharitis, conjunctivitis and iridocyclitis, as well as the pharynx and esophagus, larynx, trachea and bronchi, urethra and bladder, and genitals. Typical complaints with damage to the mucous membranes are photophobia and pain in the urethra.
The duration of the critical period depends on the rate of spread of skin lesions and the involvement of internal organs in the process, the presence of concomitant chronic infections and diseases of internal organs, as well as on the effectiveness of treatment and the timeliness of its initiation. Under unfavorable conditions, the acute period lasts about 3-5 days and in 30-70% of cases ends in death.
Causes of death:
- pronounced disturbance of the acid-base state and water-electrolyte balance;
- significant hemodynamic and microcirculatory disorders;
- severe intoxication of the body;
- development of disseminated intravascular coagulation syndrome (thrombohemorrhagic syndrome);
- disorder, mainly of protein metabolism;
- loss of the barrier function of the skin, infection against this background and the development of sepsis;
- respiratory, renal, liver and heart failure.
Recovery
Its duration depends on the same (listed above) factors. It is characterized by the cessation of detachment of the epidermal layer and re-epithelialization of the affected areas.
Depending on the nature of the course of toxic epidermal necrolysis, there are 3 forms:
Lightning fast
Or hyperacute, which accounts for up to 10% of all cases of the disease. The cause is medication or idiopathic. Within 1 day, up to 90% of the entire skin surface is affected. Acute renal failure, impaired consciousness, and coma develop. Such patients very often arrive at the hospital in an extremely serious, terminal condition or do not survive to hospitalization at all. Death occurs already on the 2nd – 3rd day from the onset of the disease and is 95%.
Spicy
Accounts for about 50-60% of all cases. The disease occurs in all stages, from rash to necrolysis. The affected surface area can reach 70%. The duration of the acute form is 7-20 days. From the 3rd – 4th day, symptoms of hepatic-renal, cardiovascular failure, as well as complications of an infectious nature of the lungs and genitourinary organs, are noted. Progression of the disease often leads to sepsis. Fatal outcome is observed in 60%.
Favorable
Or smoothed, the frequency of which in the total number of patients with Lyell's syndrome is on average 30%. The skin and mucous membranes are affected in no more than half of patients with a smoothed form. The disease reaches its highest manifestation on the 5th – 6th day, after which over the course of 3-6 weeks there is a gradual regression of symptoms and a complete restoration of health.
In addition, depending on the nature and extent of skin symptoms, the degree of involvement of the mucous membranes and internal organs, three variants of Lyell's syndrome are distinguished:
- atypical;
- with spots;
- without spots, which is a typical variant of toxic epidermal necrolysis.
Other symptoms
The general condition of patients with this syndrome can deteriorate sharply and become even worse over time. Decreased sweating, extreme thirst, and lack of saliva are all signs of dehydration in the body. Patients usually complain of a characteristic severe headache and may become disorientated and drowsy. People with Lyell's syndrome experience hair and nail loss. Dehydration causes blood to thicken and changes the blood supply to internal organs. Along with toxic damage to the body, disruption of the liver, lungs, heart and kidneys is observed. Anuria and severe renal failure may also develop. The addition of a secondary infection cannot be ruled out.
First aid
When a pathological process develops, first of all, it is necessary to immediately stop all medications and try to remove the drug from the body that probably provoked the pathological process. For this purpose, gastric lavage is performed, the patient is given a large amount of liquid, and a cleansing enema is performed.
If symptoms develop, it is important to call emergency services immediately. The doctor assesses the patient's condition, measuring blood pressure, heart rate, and body temperature.
If necessary, the specialist administers antihistamines and hyposensitizing medications to the patient parenterally. Painkillers may be used.
It is also important to minimize trauma to the skin. For this purpose, aseptic dressings are applied to the damaged areas.
Diagnosis of Lyell's syndrome
In Lyell's syndrome, a clinical blood test will usually indicate an inflammatory process. An increased ESR is also observed, as well as leukocytosis with the appearance of immature forms. A reduced level of eosinophils (or their complete absence) in a blood test is considered a sign that helps distinguish Lyell's syndrome from any other allergic conditions. Data from a coagulogram may indicate an increased level of blood clotting. A urine test and a biochemical blood test will help detect disorders occurring in the kidney tissues, as well as monitor the body’s well-being during treatment.
Before prescribing treatment, doctors suggest first identifying the medication that could lead to Lyell's syndrome, since its repeated use during therapy can be dangerous for the patient. Many immunological texts will help identify the substance that became the provocateur. The identification of a provoking drug can be indicated by the accelerated proliferation of immune cells, which occurs as a reaction to its introduction into a sample of the patient’s blood.
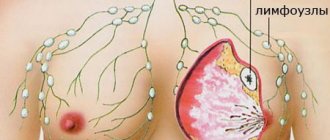
A biopsy or histological examination of a skin sample from a patient with Lyell's syndrome may reveal complete death of epidermal surface cells. In the deep layers, the formation of large blisters, swelling and accumulations of immune cells can be observed, with the highest concentration in the area of the skin vessels.
Lyell's syndrome is usually differentiated from acute forms of dermatitis, which are accompanied by the appearance of blisters:
- pemphigus;
- Steven-Johnson syndrome;
- actinic dermatitis;
- contact dermatitis;
- epidermolysis bullosa;
- herpes simplex;
- Dühring's dermatitis herpetiformis.
Treatment of Lyell's syndrome
Treatment of patients with Lyell's syndrome is carried out in the intensive care unit. Treatment includes a whole range of different emergency medicine measures. Doctors take into account the toxic-allergic nature of the disease itself; medications should be taken strictly according to clinical indications or contraindications.
Therapy for Lyell's syndrome is carried out by injection - through the administration of significant doses of corticosteroids. If the patient feels well, they are transferred to the drug in tablet form with a gradual reduction in the dose. Using the method of extracorporeal hemocorrection, including hemosorption, plasmapheresis helps cleanse the blood of toxic substances that have arisen. Regular infusion therapy (hemodesis, saline, rheopolyglucin) is aimed at combating dehydration and normalizing water-salt balance. Infusion therapy is carried out exclusively with strict control of urine output.
For complex treatment of Lyell's syndrome, drugs are used that support the functioning of the liver and kidneys, as well as enzyme inhibitors that can participate in tissue destruction, all kinds of minerals (including magnesium, potassium and calcium), anti-clotting medications, diuretics and broad-spectrum antibiotics.
Forecast
Since 2011, the SCORTEN scale for assessing the severity of Lyell's syndrome has been widely used in the West. It takes into account the following prognostic factors:
- patient age > 40 years;
- Heart rate > 120 beats. in min.;
- presence of concomitant malignant oncological disease;
- affected body surface area > 10%;
- blood urea level > 10 mmol/l;
- plasma bicarbonate level
- blood glucose > 14 mmol/l.
The presence of each factor increases the risk of death. Thus, the approximate risk of death is: in the presence of 1 factor - up to 3.2%; 2 factors - 12.1%; 3 factors - 35.3%; 4 factors - 58.3%; 5 or more factors – 90%.
Clinical case
In 2009, in Donetsk, I witnessed a rare case for Donbass (only 6 cases in the Donetsk region from 1991 to 2013!) case of Lyell's syndrome. Patient: 37 years old. Allergic and infectious anamnesis are not burdened. Three days before admission, she fell ill with a cold. She was treated with “familiar” medications: cough tablets, eye drops, nasal drops, vitamins. From the evening of the second day, itching and rashes appeared. She took suprastin on her own. After short-term relief, the condition worsened. In the evening on the third day, after fainting, she was taken to the city hospital by emergency medical services, and within a few hours was transferred to a regional clinic. A woman was admitted with hyperemic skin on her chest, shoulders, and inner thighs. On the third day, bubbles filled with cloudy contents appeared. The volume of others reached 100 ml. Throughout the entire period, hyperemia of the eyelids, sclera, mucous membranes of the oral cavity, and perianal area persisted.
From the third day, the combustiologist made repeated attempts to close the wound surface of the xenoskin. However, short-term periods of calm were replaced by psychomotor agitation in the patient, which led to displacement of the bandages and xenoskin. Not a single flap took root. Over the course of two weeks in the intensive care unit, the patient spent more than half of the time in forced medicated sleep. And from the sixth day, when the patient’s condition became critical, she was transferred to permanent mechanical ventilation.
In this case, Lyell's syndrome was diagnosed within two days after the patient was admitted to the hospital; the course of the disease was not lightning fast, but rather acute; Asymptomatic therapy was carried out, but it was not possible to save the woman.
Use of local drugs
If we talk about local treatment of Lyell's syndrome, it involves the use of aerosols containing corticosteroids, the use of wet and quickly drying dressings, and all sorts of antibacterial lotions. Local therapy is carried out in accordance with the rules for treating burns. In case of Lyell's syndrome, to prevent infection, underwear is changed several times a day, and the skin and mucous membranes are treated. Taking into account the painfulness of the procedures, therapy is carried out using a specific painkiller. If necessary, make dressings. They are usually bandaged under anesthesia.
Flow
Based on the nature of the course, there are three variants of the clinical picture of Lyell’s syndrome:
- Fulminant form - up to 10% of all cases. Develops over several hours. Etiology: idiopathic or drug-induced. Skin lesions cover up to 90% of the body surface per day. Impaired consciousness up to coma. Acute renal failure - anuria. Due to the fact that most of these patients do not survive to hospitalization or are admitted in a terminal condition, the fatal outcome is 95% within 2–3 days. At autopsy, the internal organs are usually intact.
- Acute form - 50–60% of cases. Damage to the skin and mucous membranes goes through the entire spectrum of maturation: from rashes to necrolysis. The area of necrolyzed surfaces can reach 70% of the body surface. The disease lasts from 7 to 20 days. Starting from 3–4 days, symptoms of renal, hepatic, cardiovascular, and pulmonary failure appear, as well as infectious complications—primarily pulmonary and genitourinary system infections—and as the disease progresses, sepsis. Mortality reaches 60%.
- Favorable course (smoothed form) - frequency up to 30% of cases. Damage to the skin and mucous membranes does not exceed 50% of the body surface. Clinical manifestations reach their peak on days 5–6 of the disease. Then, within 3–6 weeks, the patient’s condition improves until full health is restored.
The overwhelming majority of patients - more than 90% - have erosive changes in the mucous membranes. Typical complaints are pain along the urethra during urination and photophobia.
A positive Nikolsky symptom is characteristic: detachment of the epidermis on externally unchanged skin with sliding pressure and detachment of the peri-vesical epidermis when pulling on a piece of the vesical tire. In especially severe forms, total detachment of the epidermis is observed due to friction over the entire surface of the patient’s body.