Most often, the disease develops as a result of long-term administration of large doses of glucocorticoids to the patient for the purpose of treating a number of autoimmune pathologies.
The syndrome includes:
- Cushing's disease is an excessive synthesis of adrenocorticotropic hormone (ACTH) by the pituitary gland, which triggers a number of hormonal changes. Accounts for 80% of all pathological conditions included in the syndrome.
- Corticoliberin-ectopic syndrome - develops in most cases with bronchial carcinoma (up to 46%), lung cancer (up to 20%), pheochromocytoma (up to 23%), malignant tumor of the thyroid gland (up to 7%). Rarely, ectopic ACTH production is affected by neoplasms at other sites. This condition accounts for up to 18%.
- Iatrogenic cancer of the adrenal cortex is a malignant formation that appears as a result of the influence of various medical treatment and diagnostic procedures on the body (drug and radiation therapy, surgical trauma). Iatrogenic tumors include adenomas, adenomatosis, and adenocarcinomas. Iatrogenic cancer accounts for 1–2%.
In all conditions included in the syndrome, hypercortisolism is observed - increased production of cortisol (adrenal hormone), which causes similar symptoms of Itsenko-Cushing syndrome. Depending on the etiological factors, treatment of the disease can be either conservative or surgical.
What is hypercortisolism syndrome
Hypercortisolism is a condition in the human body, an endogenous process in which an extremely large amount of the hormone cortisol is produced in the adrenal cortex, which destabilizes the entire hormonal system and has a detrimental effect on the overall health of a person.
Hypercortisolism has a number of other names, the most commonly used of which are: Itsenko-Cushing syndrome, Cushing's disease, Cushingoid.
In most cases, the disease can be treated, however, this must be done as early as possible, because excessive neglect of the disease leads to an unfavorable outcome.
There are several reasons that contribute to the formation of excess cortisol in the adrenal cortex, but its further effect on the body is always the same: carbohydrate, protein and fat metabolism is disrupted, the concentration of sugar in the blood increases significantly (leads to diabetes), proteins break down (they are the building material of tissues) organism). All of these processes impair the functioning of all organs and systems.
Cushing's syndrome in children
The disease is rare in children; almost twice as many of the total number of children are girls. Itsenko-Cushing syndrome can develop in a child of any age group, including newborns, but sick children of school age are more common.
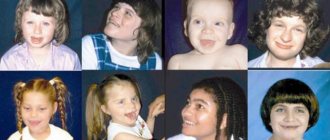
The pathogenesis of hypercortisolism is extremely similar in children and adults. But the main indicators that a child needs to be shown to a doctor are obesity with the presence of pigmentation in the fat folds and growth retardation. As a child gains weight, fat deposits are distributed unevenly: you may notice that fat accumulates especially strongly in the area of the head, collarbones and neck. Almost 75% of children with the disease have high blood pressure; many have difficulty exercising and experience muscle weakness.
The disease can develop in the body for a long period of time and not manifest itself with significant symptoms. So, from the moment the symptoms first appear until the patient begins to be diagnosed, it can take from six months to five years, on average this period is two years.
Treatment of children with Itsenko-Cushing syndrome is accompanied by drug therapy, irradiation of the area of the brain in which the pituitary gland is located - proton therapy. The procedure involves sending proton beams to the area where adrenocorticotropic hormone is produced, the main stimulator of cortisol production, and its gradual destruction occurs.
Publications in the media
Regarding the treatment of this disease, you can contact the Surgical Department No. 2 of the Clinic of Faculty Surgery named after. N.N. Burdenko
Itsenko-Cushing syndrome (Cushing's syndrome) is hypercortisolism caused by an increase in the content of endogenous or exogenous GCs in the blood. Endogenous GCs appear due to their overproduction by the adrenal cortex in the presence of: • glucosteroma; • hyperproduction of ACTH by the anterior lobe of the pituitary gland (presence of adenoma; in this case they speak of Itsenko-Cushing’s disease); • ACTH-secreting tumors of various organs (primarily the lungs; in this case they speak of the syndrome of ectopic ACTH production). Exogenous GCs cause drug-induced Itsenko–Cushing syndrome, which occurs much more often than spontaneous; usually develops in patients receiving GCs for a long time for various diseases (for example, autoimmune diseases).
Statistical data. Most often, Itsenko–Cushing syndrome is iatrogenic in nature. In the United States, the incidence of Itsenko–Cushing syndrome, caused by endogenous hyperproduction of GCs, is 13 cases per 1 million population. Of these, 70% are caused by Itsenko-Cushing's disease with the presence of an ACTH-producing adenoma, 15% by ectopic ACTH production, and 15% by a primary adrenal tumor (glucosteroma). The predominant gender is female (5:1). Predominant age: for Cushing's syndrome caused by pituitary or adrenal adenoma - 25-40 years, for ectopic ACTH production due to lung cancer - elderly age.
Etiology
• Treatment of GC: usually Itsenko-Cushing syndrome occurs with systemic use of GC, but it can develop with intra-articular administration of GC and even inhalation use. The range of diseases for which GCs are prescribed is very wide and includes a variety of rheumatological, nephrological, pulmonary and neurological pathologies; In addition, the use of GC is possible in the presence of transplanted tissues and organs.
• Endogenous hyperproduction of GC due to: •• the presence of ACTH-producing pituitary adenoma (as part of Itsenko-Cushing's disease), which, when large, compresses the pituitary tissue and suppresses the production of most pituitary hormones, as well as leading to ophthalmological disorders; •• lesions of the adrenal glands: glucosteroma (adenoma or carcinoma), macro- or micronodular hyperplasia (a simultaneous increase in hyperproduction of both GC and androgens by cells of the reticular or zona fasciculata of the adrenal cortex is possible) •• ectopic production of ACTH by cancer cells in oat cell or small cell carcinoma lung.
Pathogenesis
• Increased ACTH synthesis leads to adrenal and extra-adrenal effects •• Adrenal - increased content of GC and androgens in the reticular layer of the adrenal cortex. To a lesser extent, ACTH affects the increase in the concentration of mineralocorticoids •• Extra-adrenal - hyperpigmentation of the skin and mucous membranes (in 10% of cases) and mental disorders
• Increased HA production is a key point in the pathogenesis of Itsenko-Cushing syndrome/disease. Effects: •• Catabolic effect on protein and carbohydrate metabolism leads to atrophy of muscle (including cardiac) tissue and skin, as well as hyperglycemia with the development of steroid diabetes (in 20% of cases). In the pathogenesis of steroid diabetes, relative insulin deficiency (with increased gluconeogenesis in the liver) and insulin resistance also play a role •• Anabolic effect on fat metabolism leads to obesity (more than 90% of cases) •• Mineralocorticoid activity promotes activation of the renin-angiotensin-aldosterone system with the development of arterial hypertension and hypokalemia. The GC potentiation of the effect of catecholamines and biogenic amines (in particular, serotonin) has a certain significance in the pathogenesis of arterial hypertension. •• The catabolic effect on bone tissue leads to a decrease in the ability of bone tissue to fix calcium and the development of osteoporosis (more than 80% of cases). A certain role in the pathogenesis of osteoporosis is played by a decrease in GC reabsorption of calcium in the gastrointestinal tract, which is associated with inhibition of the processes of hydroxylation of calciferol •• Suppression of specific immunity leads to the development of secondary immunodeficiency •• Increased secretion of androgens (testosterone) by the adrenal glands leads to a decrease in the gonadotropic function of the pituitary gland and the development of sexual disorders • • Changes in the secretion of other tropic hormones - decreased levels of growth hormone and TSH, increased levels of prolactin.
Clinical manifestations
• Symptoms of a fat metabolism disorder define a Cushingoid appearance: •• Moon face (deposition of fat on the face) •• Deposition of adipose tissue on the neck (“buffalo hump”) and upper torso (especially noticeable above the collarbones), but not on the extremities (“colossus hump”) with feet of clay").
• Symptoms of carbohydrate metabolism disorders - steroid diabetes or decreased glucose tolerance with rapidly increasing hyperglycemia and/or glycosuria.
• Symptoms of protein metabolism disorders: •• Muscle weakness - steroid myopathy: patients have difficulty climbing stairs, rising from a low chair, raising their arms •• Red-violet stretch marks on the skin of the abdomen, chest and thighs •• Predisposition to ecchymosis (due to increased capillary fragility) •• Slow wound healing •• Predisposition to infections due to immunodeficiency.
• Symptoms of impaired water-electrolyte metabolism: an increase in BCC due to water and sodium retention.
• The presence of an ACTH-producing pituitary adenoma (as part of Cushing's disease) leads to the appearance of ophthalmological disorders, headaches, galactorrhea and other disorders (see Pituitary adenoma).
• Other disorders: •• Arterial hypertension (newly detected or progressive) •• Lipid metabolism disorders (increased synthesis of both HDL and LDL, triglycerides) contribute to the rapid progression of atherosclerosis of the coronary arteries and the development of coronary artery disease •• Petic ulcers, sometimes asymptomatic, especially in patients receiving high doses of GC •• Osteopenia and osteoporosis (up to osteoporetic fractures); avascular necrosis of the femur is also possible •• Disorders of hormonal regulation of the reproductive system (dysmenorrhea, amenorrhea, infertility) •• Acne, hirsutism •• Formation of trophic ulcers and pustular skin lesions (due to the development of secondary immunodeficiency) •• Hyperpigmentation of the skin and mucous membranes (ACTH effect ), usually in areas of skin friction - an important differential diagnostic sign for identifying excess ACTH production •• Emotional lability, depression, cognitive disorders •• In children - growth retardation.
Adrenal crisis. Emergency condition; may occur in patients with Itsenko-Cushing syndrome due to abrupt cessation of GC intake, as well as if the dose of GC is not increased when the patient develops any acute disease. In addition, it occurs in the postoperative period after removal of an ACTH- or GC-producing tumor.
Clinically manifested by arterial hypotension, abdominal pain, vomiting and disturbances of consciousness. Laboratory changes include hypoglycemia, hyponatremia, hyperkalemia, and metabolic acidosis.
Laboratory data. The main goal is to determine the hyperproduction of HA in the patient’s body with the simultaneous determination of ACTH content (the condition for reliable results is that the patient does not have an acute illness). The first step is to assess the dependence/independence of manifestations on ACTH • To identify overproduction of GC, it is necessary to detect increased levels of cortisol itself or its metabolites in the blood or in the urine (increased daily urinary excretion of free cortisol or 17-hydroxycorticosteroids [17-OX]) • • An increase in the concentration of cortisol in the blood at night (preferably closer to midnight) of more than 7.5 mcg% is a reliable sign of Itsenko-Cushing syndrome. Even more reliable is the detection of elevated levels of cortisol in the blood for several days in a row. Currently, methods for determining the content of cortisol in saliva (saliva collection at home) have been developed, but their use is limited due to high cost • An increase in the level of ACTH in plasma to 20 pg/ml (the most significant increase at night) is an important differential diagnostic sign •• With glucosterome due to excessive production of cortisol, the secretion of ACTH by the pituitary gland is suppressed, which leads to a decrease in its level in plasma (less than 5 pg/ml) •• In the syndrome of ectopic ACTH production or ACTH-serating pituitary adenoma, its concentration is 10–20 pg/ml and higher.
However, to identify Itsenko-Cushing syndrome, two screening tests are usually used (more convenient).
• Daily cortisol excretion test. This is the most reliable test for detecting daily hyperproduction of HA. An increase of more than 3–4 times (relative to the upper limit of normal) indicates an undoubted diagnosis of Itsenko–Cushing syndrome/disease, while with an increase of 2–3 times it is necessary to carry out differential diagnosis with Itsenko–Cushing pseudosyndrome. When performing the test, you should make sure that the patient correctly collected daily urine - to do this, you need to determine the amount of creatinine in the same daily urine.
• Overnight dexamethasone suppression test is a primary diagnostic test for suspected Cushing's disease or syndrome (administration of exogenous GC normally leads to a decrease in the production of ACTH and, therefore, cotrizol). The patient takes 1 mg of dexamethasone orally at 11 o'clock in the evening, and the next morning at 8 o'clock the serum cortisol level is determined •• Serum cortisol concentration less than 1.8 mcg% indicates normal suppression of ACTH and cortisol by dexamethasone and allows excluding the diagnosis of Itsenko-Cushing syndrome . In this case, the test is considered sensitive, there is no need to further clarify the diagnosis •• In patients with Cushing's disease or syndrome, the cortisol concentration during this test exceeds 1.8 μg% (usually 5–10 μg%). When such results are obtained, the test is not considered sufficiently specific, since false positive results are possible (obesity, alcoholism, stress, chronic renal failure, anorexia, bulimia; taking phenobarbital, contained, for example, in drugs such as Corvalol, Valocordin, tamoxifen, rifampicin).
If further examination is necessary, the following tests are used.
• The standard dexamethasone suppression test is a reliable test for the diagnosis of Cushing's syndrome/disease, although the sensitivity and specificity of this test is approximately 70%. Suppression of the hypothalamic-pituitary-adrenal axis is studied by administering low-dose dexamethasone (0.5 mg dexamethasone divided into 8 doses, every 6 hours orally for 2 days) with measurement of serum cortisol concentrations and urinary 17-OX levels on the second day. day (expected to decrease). Currently, a combination of the standard dexamethasone suppression test with additional administration of corticoliberin (1 mcg/kg IV 2 hours after taking the eighth dose of dexamethasone) is considered promising. The test can also detect a reduction in 17-OX excretion by more than 50%.
• The overnight high-dose dexamethasone suppression test is more convenient to perform than the standard test. It is used when ACTH levels are intermediate between 5 and 10 pg/ml. Serum cortisol concentrations are determined at 8 a.m. for two consecutive days, and 8 mg of dexamethasone is taken at 11 p.m. on the first day. A drop in serum cortisol levels of more than 50% on the second day indicates a pituitary origin of excess ACTH rather than ectopic ACTH production or primary adrenal pathology.
• Corticoliberin stimulation test. Corticoliberin is administered parenterally and after 15 minutes the levels of ACTH and cortisol are measured. In Itsenko-Cushing's disease, the levels are usually elevated (for cortisol - more than 1.4 μg%), the absence of a response indicates an ectopic or adrenal genesis of hypercortisolism.
Other criteria • Neutrophilic leukocytosis (sometimes more than 11´109/l) • Hyperglycemia and glycosuria • Hyperlipidemia • Hypokalemia • Lymphopenia • Eosinopenia.
Instrumental data. The use of special research methods must be preceded by a thorough laboratory examination.
• X-ray of the skull reveals macroadenomas of the pituitary gland (10% of cases), X-ray of the lumbar spine reveals osteoporosis. However, for diagnosing Itsenko–Cushing syndrome and disease, this method is currently considered to be of little information.
• If Itsenko-Cushing's disease (pituitary origin of excess ACTH production) is suspected, it is necessary to conduct imaging studies of the head •• CT scan of the head with the introduction of contrast can detect about 50% of pituitary adenomas •• MRI with gadolin contrast - the method of choice - allows us to detect about 75% of such tumors •• Often, even with MRI, no changes are detected due to very small microadenomas or diffuse hyperplasia of the corresponding pituitary cells. In this case, it is useful to separately determine the ACTH content in the blood from the inferior petrosal sinus and peripheral veins. Blood samples are taken from peripheral veins and (by catheterization) from the inferior petrosal sinus of the dura mater. A ratio of the level of ACTH in the sinus blood to the level of ACTH in the peripheral veins of more than 2.0 is observed in Cushing's disease, while a ratio of less than 1.5 is characteristic of the syndrome of ectopic ACTH production.
• If pathology of the adrenal glands is suspected, the following diagnostic procedures are performed •• CT scan of the abdominal cavity, which makes it possible to detect enlargement of the adrenal glands (if their size is more than 4-6 cm, carcinoma should first be excluded, for which it is possible to conduct a targeted aspiration biopsy under CT control). Uniform enlargement of both adrenal glands suggests Cushing's disease or ectopic ACTH production syndrome. Enlargement of one adrenal gland in the presence of the corresponding clinic suggests glucosteroma • Radioisotope study using 19-iodocholesterol labeled with radioactive iodine reveals bilateral hyperplasia in the case of Cushing's disease or ectopic ACTH production syndrome, in glucosteroma - asymmetric absorption of the drug.
• If ectopic ACTH production syndrome is suspected: •• CT scan of the chest and abdominal cavities •• Scintigraphy labeled with octreotide (cells of neuroendocrine tumors have receptors for somatostatin).
Diagnostic tactics. Suspected on the basis of anamnestic and clinical data, Itsenko-Cushing syndrome, after exogenous intake of GC (even inhalation or intra-articular) has been excluded, requires verification through a thorough laboratory examination aimed at identifying the source of GC hyperproduction and the dependence of the condition on ACTH. Special instrumental research methods (of the head, adrenal glands or chest cavity) are prescribed for final verification of the diagnosis after a hypothesis about the cause of Itsenko-Cushing syndrome has been formulated, based on laboratory findings.
Differential diagnosis • Functional hypercortisolism in alcoholism (currently referred to as “alcohol-induced pseudo-Cushing syndrome”) and pregnancy • Depressive disorders - they are often manifested by changes in the functions of the hypothalamic-pituitary-adrenal system with hyperproduction of GC and secondary development of moderate Itsenko-Cushing syndrome. On the other hand, Itsenko-Cushing syndrome can manifest itself as emotional lability and depression, so the combination of both conditions requires a careful search for the root cause • Obesity, occurring with arterial hypertension and carbohydrate metabolism disorders • Adrenogenital syndrome.
TREATMENT
General tactics. Treatment for Cushing's syndrome/disease depends on the cause. Iatrogenic syndrome (treatment is mandatory in this case as well) involves the gradual withdrawal of GCs (with their replacement, if necessary, with other immunosuppressants).
For Itsenko–Cushing syndrome with overproduction of HA, the method of choice is surgical removal of the causative tumor (pituitary gland, adrenal glands, lungs). If surgical treatment is ineffective or impossible (which is more often the case with ectopic ACTH secretion syndrome or metastatic carcinoma), drug treatment is attempted. Unfortunately, the latter often turns out to be ineffective, and then they resort to bilateral adrenalectomy. For ACTH-producing pituitary adenoma, they often resort to, among other things. to radiation therapy.
Drug therapy. To provide “medicinal adrenalectomy,” drugs such as mitotane, ketoconazole, and aminoglutethimide are used. However, at doses that cause a decrease in cortisol synthesis, these drugs are often toxic. Therefore, when prescribing them, it is necessary to carefully monitor the patient, assessing the effectiveness of the therapy by the level of daily cortisol excretion • The drug of choice for long-term use is ketoconazole. It inhibits both the synthesis of cortisol and, most likely, ACTH • Currently, studies are being conducted on the effectiveness of drugs that reduce the secretion of ACTH and corticoliberin - bromocriptine, octreotide, valproic acid, cyproheptadine.
Radiation therapy. It is used when treatment - surgical or medicinal - is ineffective, usually in combination with them. Radiation therapy increases the effect of drug treatment.
Surgery
• The method of choice for Cushing's disease is transsphenoidal resection of the pituitary adenoma with the maximum possible preservation of its functions. Endoscopic techniques are now becoming available. The operation is successful in 60–80% of cases and is accompanied by the subsequent establishment of normal function of the pituitary gland and adrenal glands and the cure of Itsenko-Cushing syndrome. If conventional surgical treatment is ineffective, it is necessary to keep in mind the possibility of performing surgery on the pituitary gland using MRI guidance.
• In case of ectopic ACTH production, surgical treatment of the identified tumor is performed; if this is not possible, drug treatment or bilateral adrenalectomy is indicated.
• For adrenal tumors, unilateral adrenalectomy is usually performed.
• Bilateral adrenalectomy is indicated in two cases: •• ineffectiveness of previous therapy (surgical, radiation, drug); •• the need to quickly normalize the concentration of cortisol in the blood. The procedure cures Cushing's disease, but the patient develops Addison's disease and needs lifelong replacement of steroids (GC and mineralocorticoids). In addition, in some cases, after adrenalectomy, Nelson's syndrome develops, in which the pituitary adenoma begins to grow rapidly, because it is no longer inhibited by elevated cortisol levels.
Complications • Osteoporosis • Predisposition to purulent-inflammatory diseases • Hirstutism • Diabetes • Arterial hypertension • Adrenal crisis • Panhypopituitarism • Diabetes insipidus • It should be borne in mind that with an increased content of HA in the blood, the clinical picture of acute pathology of the abdominal cavity can be extremely poor.
Forecast. Depends on the cause of the condition, as well as the possibility and effectiveness of surgical treatment.
Reduction. 17-OX - 17-hydroxycorticosteroids.
ICD-10 • E24 Itsenko-Cushing syndrome
Pathogenesis of Itsenko-Cushing's disease
Cortisol is produced under the direct influence of ACHT (adrenocorticotropic hormone) in the brain, so if ACHT is disrupted, dysfunctional cortisol production will be created. Speaking about the reasons, it is necessary to analyze first of all the conditions that cause disturbances in the functioning of ACHT.
The causes of ACHT dysfunction and, consequently, the development of Cushing's syndrome can be:
- a benign tumor of the pituitary gland, the very part of the brain where adrenocorticotropic hormone is produced, the tumor can be small or large, grow or remain in place, the production of the hormone and the amount of cortisol produced will depend on its actions;
- improper functioning of the hypothalamus - this part of the brain produces the substance corticoliberin, which directly affects the synthesis of ACHT in the pituitary gland;
- the presence of ectopic tumors, in more than half of all cases they are found in the chest.
In addition to the causes associated with ACHT, there are others that are less common:
- adrenal tumor (occurs in about one in a million people);
- taking high doses of cortisol.
FORECAST
There is no clear prognosis for Itsenko-Cushing disease. The consequences of the disease depend on the severity and duration of the pathology, as well as the age of the patient.
If therapy begins at a mild stage, and the patient’s age is less than 30 years, then complete recovery is possible.
With prolonged exposure to NIR on the human body, even with the elimination of provoking factors, complications in the functionality of the urinary, skeletal and cardiovascular systems cannot be avoided. In 40% of cases the patient becomes disabled.
Advanced disease leads to septic processes and renal failure, resulting in death.
Symptoms of hypercortisolism
Hypercortisolism has quite a lot of symptoms, however, they are all too vague, they can be attributed simply to fatigue, confused with other diseases, or they will be so mild that a person simply will not pay attention to them at first. The severity of symptoms depends on many factors and is individual for each patient, this is due to the fact that the root causes may be different, the body itself reacts differently to problems, and the symptoms appear more clearly with a long course of the disease.
With Itsenko-Cushing's disease the following are observed:
- rapid and uneven increase in body weight, so fat deposits are concentrated in the body and head, but the limbs may remain the same;
- thinning of the skin occurs - the skin turns pale, it is easy to bruise, wounds heal more slowly than usual, in addition, due to rapid weight gain and weakness of the skin, a person develops pronounced stretch marks (striae);
- an excess amount of cortisol makes changes to the entire hormonal system, for example, in women the nature of the cycle may change or disappear altogether, male sex hormones may predominate over female ones, which will lead to excess body hair in women;
- osteoporosis – if you have this diagnosis, it is necessary to do an analysis of the amount of cortisol and the condition of the adrenal glands;
- weakness, apathy, fatigue;
- loss of strength leads to reluctance to do anything, a person may notice a decrease in muscle mass;
- presence of diabetes or prediabetes;
- heart problems, often high blood pressure;
- insomnia, panic attacks and increased anxiety;
- thrombosis.
Significant weight gain with Itsenko's syndrome occurs in almost 90% of cases; it is especially clearly reflected on the person's face, which becomes more rounded and red.
More than half of patients have stretch marks or stretch marks; they are bright red or purple in color. Problems with sugar occur in 80% of people, so a glucose tolerance test is a very important element of diagnosis. Irregularities in the functioning of the heart occur in slightly less than 90% of patients, so they are also a wake-up call for a person.
In the photo you can see clear signs of Cushing's syndrome, which need to be treated urgently.
Inspection and survey
At the appointment, the doctor interviews the patient in detail about all symptoms and changes in health status. Possible factors that could provoke the disease are established. Concomitant pathologies are determined.
Next is a visual inspection and palpation. Characteristic signs are considered to be severe excess of body weight, the presence of stretch marks, changes in the skin, and problems with hair growth.
Based on the information received, the doctor makes a preliminary diagnosis and refers the patient to all necessary types of examination.
Itsenko-Cushing syndrome: diagnosis
To conduct a high-quality and informative diagnosis, you must first consult a doctor who will collect anamnesis and prescribe appropriate studies. At the moment, there are several types of diagnostics to identify Itsenko-Cushing's disease. They can be used together or separately at different periods, but most often several types of studies are prescribed at once to obtain a more complete and reliable picture of the disease. The main methods for identifying hypercortisolism are:
- blood or saliva test for cortisol - this test must be carried out strictly with all the doctor’s instructions, since cortisol is a fairly mobile hormone and its concentration in the blood is different at different times of the day;
- an analysis is taken to determine the amount of glucose in the blood (its high values may indicate the presence of pathology), a glucose tolerance test and a general blood test with a detailed leukocyte formula are done;
- conducting a small dexamethasone test - the study consists of taking a cortisol test from the patient early in the morning, on the same day in the evening he takes 1 mg of dexamethasone and again donates blood for cortisol in the morning. If the second morning value is higher than the established norm of 50 nmol/l, then we can talk about the presence of hypercortisolism;
- There is also a large dexamethasone test; this test is performed if a small sample is informative or for additional differential diagnosis. This study is of great benefit, as it helps not only to identify the disease, but also to suggest the cause of its development, and this will help the specialist to more correctly develop a treatment plan;
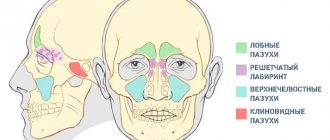
- For a more specific diagnosis, computed tomography or magnetic resonance imaging of the adrenal glands and some areas of the brain may be prescribed; these CT and MRI studies are interchangeable; only one can be performed, but as a rule, CT of the adrenal gland and/or MRI of the pituitary gland are performed. As a result, it will be possible to assess the size of the adrenal glands and the state of the brain, the processes occurring in them and the presence of neoplasms; if any are identified, then in the image it will be possible to fully assess their nature.
If a patient has osteoporosis and symptoms of Cushing's disease, we can talk about almost 100% probability of a diagnosis of hypercortisolism.
Laboratory diagnostics
Since the level of ACTH in the blood plays a major role in making a diagnosis, it is this test that must be taken in addition to the general biochemical one. With the development of hypercortisolism, ACTH will be at a level of 80 - 150 pg/ml.
Another indicator is cortisol levels. However, cortisol can fluctuate for other reasons, so it is not considered the main one. For more accurate information, a study of 24-hour urine or saliva can be performed. Additionally, a small dexamethasone test is performed, which consists of the effect of dexamethasone on cortisol. If NIR develops, the test will give a negative result.
The list of laboratory tests also includes biochemical AK, which can detect: a decrease in the level of activity of phosphatase (alkaline), potassium, albumin and phosphates; increasing the amount of chlorine, cholesterol, globulins and sodium.
Treatment of Itsenko-Cushing's disease
It is necessary to understand that the treatment of any disease has certain goals:
- elimination of symptoms;
- preventing the development of complications;
- the onset of stable remission;
- improving the quality of human life;
- in the case of hypercortisolism, most often it is necessary to remove the tumor, but if the tumor cannot be removed, then all efforts will be devoted to stopping its growth.
Since there are several causes of the disease, they are all different and caused by various factors, treatment will be prescribed individually based on these factors. The main methods of treating Itsenko-Cushing's disease are:
- in the presence of a tumor in the adrenal cortex: first of all, removal of one or both adrenal glands, then treatment is carried out with the help of medications aimed at eliminating symptoms and normalizing lifestyle;
- in the presence of a tumor in the brain: removal of the tumor using available methods, based on the patient’s condition, before the operation the patient must take special medications that block the excessive effect of cortisol, after the operation - medications to restore the body;
- If there is excessive formation of adrenal tissue causing Cushing's disease, substances that inhibit the formation of steroids are prescribed, as well as medications to reduce the severity of symptoms; removal of the adrenal glands may be prescribed.
Removal of the adrenal glands is also carried out if it is impossible to remove a tumor in the brain or if other treatment methods are ineffective.
Forecast
Itsenko-Cushing's disease has a progressive course if treatment is not started in time. According to statistics, more than 80% of patients experience stable remission. This value decreases significantly if an inoperable tumor is discovered, in which case, even if the disease is completely ignored and without treatment, only half of the people will be able to live more than 5 years.
Which doctor should I contact?
Cushing's syndrome is usually treated by an endocrinologist. This specialist has the necessary knowledge in the field of endocrinology. An endocrinologist is involved in identifying and treating disorders of the hormonal system.
I, Georgy Nikitich Romanov, am an endocrinologist of the highest qualification category, have a scientific medical degree, and am an experienced specialist. I had the opportunity to gain my experience not only in Belarus, but also in Russia, Great Britain, France and Germany, I have knowledge about modern methods of diagnosing and treating endocrine diseases.
At the moment, you can make an appointment with me in a private clinic in Gomel or for a paid online consultation. Registration for a consultation is made through one of the sources: VKontakte, Instagram, WhatsApp, skype, Viber.
What should you do after treatment?
The patient requires constant monitoring by an endocrinologist. After treatment, it is recommended to periodically take blood tests and undergo an ultrasound of the endocrine organs.
As for prevention, methods to prevent the occurrence of endogenous Cushing's syndrome are unknown.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
conclusions
An interesting fact is what complications occur with Itsenko-Cushing syndrome. The most dangerous are cardiovascular, which increase the risk of death by 4 times compared to the usual mortality rate. Other complications depend on the extent of the disease and its cause.
In general, with timely consultation with a specialist, high-quality diagnosis and correctly prescribed treatment, most patients at any age experience stable remission, which must be maintained with medications and maintaining a correct lifestyle.
CLASSIFICATION OF CLINICAL COURSE
In medicine, Cushing's disease is divided into several forms, depending on the clinical picture. The pathology is classified according to the severity of the course and the speed of development.
Hypercortisolism, according to the severity of symptomatic manifestations and functional disorders, is:
- first degree - mild;
- second degree - average;
- third degree - severe.
In the first degree of the disease, all signs are of moderate intensity. In the second case, the symptoms are already much more pronounced, but complications have not yet arisen. The third degree is the most dangerous; in addition to clearly defined signs, the patient experiences multiple complications.
Classification according to the rate of progression of the disease involves three forms:
- torpid - the process of pathological changes occurs slowly, up to 10 years can pass before the onset of the second stage;
- progressive - the clinical course develops much faster - from six months to a year;
- cyclic - periodic manifestation of symptoms according to the type: exacerbation/remission.
The progressive form of the disease is considered the most complex, since the pathological process develops so quickly that treatment, which sometimes takes up to several years, simply does not have time to achieve the desired effect.