Strictly speaking, glaucoma is not one disease, but a whole group of diseases with similar symptoms. They are characterized by:
- increased intraocular pressure - it can be either constant or episodic;
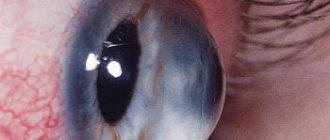
- damage and subsequent atrophy of the optic nerve;
- decreased visual acuity, impaired visual function.
Sign up for a free vision test
According to statistics, more than 70 million people suffered from this disease in 2021. In Russia, the number of cases is estimated at approximately one million. Glaucoma is the second most common cause of blindness, second only to cataracts. It is very important to be regularly examined by a specialist!
The purpose of this article is to give a general idea of glaucoma, talk about the causes of this disease, symptoms, treatment and prevention.
Types of glaucoma
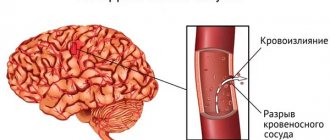
The space of the eye, filled with a transparent liquid and limited on one side by the cornea and on the other by the iris, is called the anterior chamber. There is an area called the anterior chamber angle, or ACA. In the outer wall of the UPC there is a drainage system of the eye, providing controlled outflow of intraocular fluid. Fluid circulation maintains intraocular pressure (IOP) at a constant level, and disruption of its function leads to an increase in pressure.
Accordingly, there are two main types of glaucoma:
- closed angle;
- open angle.
The first type, that is, angle-closure glaucoma, is less common; according to various estimates, it affects from 10 to 20% of the total number of cases. Most often, people over the age of 30 who also have farsightedness encounter it.
The specificity of this type is that the iris overlaps the anterior chamber angle (ACA) of the eye. For this reason, the natural drainage system is disrupted, and pressure increases in the visual organ. This may be accompanied by:
- severe headache;
- redness of the eye;
- blurred vision and other visual impairments, including complete blindness.
Open-angle glaucoma is detected in approximately 80-90% of those who experience increased IOP. In this case, access to the natural drainage system remains open, but it does not work properly. As a result, the pressure inside the eye gradually increases. Such a disease can be asymptomatic, which is especially dangerous, since a person can suddenly, without any clear reason, feel that the quality of his vision has noticeably decreased.
Open-angle glaucoma: clinical forms and their causes
Primary open-angle glaucoma (POAG) accounts for 70% of all glaucomatous diseases. In the age group of people 45 years old, its prevalence is 1-2%, by 60 years old it is already 3-4%. This is a genetically determined pathology. Also at risk are elderly people with diabetes, hypertension, myopia, and early age-related farsightedness.
There are 4 clinical forms of POAG:
- simple;
- pigment;
- pseudoexfoliative;
- normal pressure.
Simple - occurs against the background of dystrophic changes in the trabecular apparatus - the drainage system of the eye. Difficulty in the outflow of aqueous humor is accompanied by a lack of blood supply and ischemic disorders. Simple POAG is characterized by a relatively slow progression, the second eye is affected later and to a milder extent.
| Patients turn to an ophthalmologist only in the later stages due to the absence of symptoms of primary open-angle glaucoma in the initial period of the disease. |
Pseudoexfoliative POAG is characterized by a more aggressive course with high levels of hypertension.
The disease is bilateral, only a quarter of patients affect only one eye. The cause of glaucoma is amyloid-like deposits on the iris, lens, ciliary body and in the structures of the PC angle against the background of dystrophic lesions of the trabecular filter. Pseudoexfoliation syndrome leads to damage not only to the hydrodynamic, but also to the vascular system of the eyeball, general vascular pathology, aggravating the course of the disease. Pigmented POAG develops due to the “clogging” of the drainage system with lumps of pigment. Granules from the deteriorating neuroepithelial layer of the iris are also deposited on the inner surface of the cornea, causing complaints of iridescent circles around light sources. This symptom of open-angle glaucoma - the pigmented form - is constant, in contrast to similar periodic complaints during a subacute attack of angle-closure glaucoma.
POAG with normal (pseudonormal) IOP is a special form in which one of the key signs – increased ophthalmotonus – is absent. At the same time, there are other signs of the glaucomatous process - characteristic visual field defects, atrophy of the Nervus opticus with excavation. They allow pathology as a variant of reduced adaptation of the optic nerve to the individual level of IOP - the so-called low level of tolerance. All patients have systemic hemodynamic disorders - vascular crises, spasms, nocturnal hypotension, etc.
Causes of glaucoma
The balance of inflow and outflow of intraocular fluid maintains the pressure inside the healthy eye at approximately between 10 and 20 mmHg. Art. If normal fluid circulation is disrupted, pressure begins to rise. Problems arise with blood circulation in the structures of the eye, the fibers of the optic nerve die, the field of vision gradually narrows, and then the optic nerve may atrophy, and then complete blindness occurs.
Currently, experts cannot say unambiguously for what reasons glaucoma occurs. The appearance of this disease is influenced by factors such as:
- heredity;
- individual anatomical features, specific structure of the visual organs in a particular person;
- various pathologies of the cardiovascular, nervous and endocrine systems.
Risk factors for the development of glaucoma include a small volume of the anterior chamber of the eye. This structural feature of the organ of vision is found in some nationalities - Eskimos and residents of East Asia. This anatomical feature is more common in women than in men, so their risk of developing glaucoma is slightly higher.
The presence of age-related and genetic risk factors is the reason why many people should be examined at least once a year for suspected glaucoma. This primarily concerns those who:
- over 40 years of age – the likelihood of developing the disease increases with age;
- suffers from other eye diseases, such as cataracts, tumors, acute inflammation;
- has diseases of the cardiovascular, endocrine and nervous systems;
- has been taking or has taken hormonal medications for a long time;
- has relatives who have been diagnosed with glaucoma.
What is secondary glaucoma
A persistent increase in intraocular pressure can occur as a result of various diseases of the visual system, injuries to the eyeball and other conditions. Then they talk about secondary glaucoma, which develops as a complication of other pathologies. The main common pathogenetic link of all diseases that can lead to secondary glaucoma is a violation of the hydrodynamics of the natural intraocular fluid, an increase in its exudation and the impossibility of normal outflow. The degree of increase in IOP and reversibility of changes depends on the severity and duration of exposure to the secondary glaucoma factor.
Stages of glaucoma
The disease goes through several stages in its development. The transition to a more serious stage is usually expressed in the appearance of visual field defects. The field of view is the space that a person sees around him when looking at a certain point.
At the initial stage of the disease, loss of small central areas of the visual field most often occurs. The patient may either not notice this at all, or pay attention to small dark spots in front of the eyes.
Then peripheral vision gradually deteriorates. A person with glaucoma sees more or less well only what is directly in front of him. But over time, the central field of vision narrows—experts often use the term “tunnel vision” because a person feels as if they are looking at the world through a long, narrow tube. A veil appears before the eyes; it may seem that dark dots are running in front of them.
At the last stage of glaucoma, which is called terminal, complete loss of vision occurs.
Disease prevention
There are no specific measures to prevent the disease. If there is an increased risk of developing secondary glaucoma, it is necessary to adhere to the following general preventive measures:
- Be careful with your eyes. It is important to avoid injury, exposure to direct sunlight and other adverse environmental factors.
- Timely contact an ophthalmologist. Any complaints from the visual system require an immediate appointment with a specialist in order to make a diagnosis as early as possible and begin appropriate treatment. Early elimination of the primary disease is the main point in preventing the formation of glaucoma.
- Preventive examinations. Regular visits to an ophthalmologist, even in the absence of complaints, is a good way to early detect even hidden pathologies. Every person needs to measure intraocular pressure regularly, starting at age 40.
- Diet. Sufficient, varied food filled with vitamins and microelements can prevent visual impairment.
- Rest. Work associated with constant visual stress, frequent and prolonged use of the computer, and other unfavorable factors contribute to the development of various pathologies of the visual organ. It is important to provide sufficient rest to the eyes - take breaks every 20-30 minutes and do relaxing exercises.
Tips for recovery after eliminating the primary disease and treating secondary glaucoma include:
- the need to avoid stressful situations and worries;
- good sleep;
- moderate physical activity without sudden changes in body position and lifting heavy objects;
- ban on visiting saunas and steam baths - high temperature provokes surges in intraocular pressure;
- compliance with the rules of visual hygiene. After treatment, it is especially important not to spend a lot of time in front of the monitor. It is necessary to adhere to generally accepted standards of distance between the eyes and the desktop, maintain the physiological position of the back, and maintain posture;
- performing a set of exercises aimed at narrowing the pupil and reducing intraocular pressure.
Secondary glaucoma is a diagnosis for which complete cure cannot be guaranteed. Various risk factors and predisposition to the occurrence of increased intraocular pressure can manifest themselves in the form of pathology at any time. Therefore, it is important to make every effort to prevent visual impairment and associated IOP surges.
Symptoms of glaucoma
Obviously, the sooner ophthalmologists make an appropriate diagnosis, the greater the likelihood that the problem will be affected. However, signs of glaucoma, as mentioned above, often do not appear. Therefore, a person can find out about the presence of serious complications, for example, by visiting a specialist for a completely different reason.
Glaucoma is often discovered accidentally during a routine visit to the ophthalmologist.
However, there are a number of symptoms that clearly indicate that you need to see a doctor
. This:
- blurred vision;
- the occurrence of a sharp headache, including only in one half of the head;
- pain in the eye area;
- the appearance of rainbow halos around light sources;
- redness of the eye;
- blurred vision in low light, especially in the evening and at night;
- loss of peripheral vision.
Find your nearest optical store
How does secondary glaucoma differ from primary glaucoma?
Secondary glaucoma can also be open-angle or closed-angle, it has the same stages and signs as primary. However, a secondary increase in intraocular pressure has a number of characteristic differences from the primary forms of pathology:
- secondary glaucoma is always a consequence and complication of other diseases;
- most often the damage occurs asymmetrically, the disease affects one eye;
- vision loss occurs quite quickly;
- the processes are reversible if the underlying pathology can be treated.
Prevention
Preventing glaucoma is especially important for people over 45 years of age. They should follow simple recommendations from doctors - this will reduce the likelihood of the development and progression of the disease:
- Do not lift weights exceeding 12 kg;
- you need to ensure that your night's sleep is regular, sound and lasts at least 8 hours;
- people with a hereditary predisposition to glaucoma should not be in a position in which the head is tilted forward for a long time - washing floors, weeding the garden or picking berries;
- it is necessary to control blood pressure, monitor the amount of fluid and salt consumed, drink less coffee and eat more plant foods;
- You should avoid overwork, stress and nervous tension;
- It is undesirable to be in rooms with sudden changes in lighting;
- it is necessary to protect your eyes from sudden flashes;
- it is better to refuse to visit cinemas or reduce such visits to a minimum;
- stop drinking alcohol and tobacco.
Treatment of open-angle primary glaucoma
If the disease is detected, antihypertensive drops are prescribed. The drug of first choice, in the absence of contraindications, is prostaglandins F-2a - Xalatan, Travatan, Prolatan or their analogues.
After 2 weeks, the drug effect is monitored; if the effect is insufficient, the drug is changed or supplemented with a second one of a different mechanism of action. These may be beta blockers (Timolol, Betoptik, Proxodolol) or carbonic anhydrase inhibitors (Azopt, Dorzopt, Trusopt). Combination pharmaceuticals are also used - Xalacom, Azarga, Dorzopt-Plus, etc.
| Independent withdrawal or replacement of drugs is unacceptable! |
On the eve of the control IOP measurement, it is imperative to instill medicinal drops according to the prescribed regimen. If this condition is not met, it is impossible to evaluate the effectiveness of conservative treatment of primary open-angle glaucoma. The use of these medications is constant, daily, according to the schedule recommended by the ophthalmologist.
Treatment of glaucoma is supplemented with courses of vascular therapy to improve blood supply and metabolic processes in the brain.
If ophthalmotonus persists despite the use of 2 or more medications, surgical treatment of open-angle glaucoma is indicated.
Surgical treatment of open-angle glaucoma
Glaucoma surgeries are aimed at normalizing hydrodynamics and do not restore visual functions. Glaucoma intervention is performed with a laser or scalpel at stages I-III. Their goal is to artificially form additional pathways for the outflow of aqueous humor.
Laser treatment of open-angle glaucoma - trabeculoplasty (TTP) and its variant, selective TTP - improves the permeability of the trabecular apparatus for aqueous humor. This is the operation of choice provided that hypertension is compensated and there are no other contraindications.
Microsurgical treatment of open-angle glaucoma with fistulizing operations (non-penetrating deep sclerectomy, trabeculectomy, sinusotomy) allows you to direct part of the intraocular fluid under the conjunctiva.
Cyclodestructive interventions reduce the secretion of the ciliary body. These operations are usually performed for terminal painful glaucoma, since there is a high probability of severe hypotony and atrophy of the eyeball in the postoperative period.
Surgical treatment of open-angle glaucoma does not exclude a rise in pressure in the future due to fibrous degeneration in the intervention area. In most cases, even after a successful operation, laser or microsurgical, there remains a need for daily instillation of antihypertensive drops in a minimum dosage.
There is no treatment for open angle glaucoma to prevent the disease. By strictly following the recommendations of your doctor regarding the treatment of open-angle glaucoma and regular scheduled examinations, you can significantly slow down the development of the process.
Glaucoma treatment
Damage to the optic nerve and, especially, vision loss due to glaucoma are irreversible. However, there are ways to normalize intraocular pressure and thereby prevent or stop the progression of the disease.
Conservative, that is, drug treatment involves the use of various medications, primarily eye drops. At the same time, it is necessary to understand that they do not “cure” in the literal sense of the word, that is, they do not change the structure of the eye in such a way that the natural fluid outflow system works again without disruption. They artificially maintain fluid balance in the eye. If you stop using the drops, after a while the disease will begin to progress.
Surgical treatment of glaucoma is used in cases where medications do not help. The main goal of the operation is to remove obstacles to the outflow of intraocular fluid or to create new pathways. There are several ways to achieve this. Most often, specialists:
- use modern laser techniques to, for example, expand existing or create new channels for outflow of IOP;
- special devices are implanted through which intraocular fluid is removed: tubes, drains, valves.
Treatment methods
Treatments include eye drops, tablets, laser surgery, traditional surgery, or a combination of these methods. Their goal is to prevent permanent vision loss due to glaucoma. The main goal of treatment is to reduce IOP to an acceptable level, which is achieved in two ways: reducing the production of intraocular fluid and improving fluid outflow. Optimism is inspired by the fact that the course of glaucoma can be controlled if it is detected early, and thanks to conservative and/or surgical treatment, most patients do not lose the ability to see.
Treatment tactics depend on its type, cause of development, and severity of the disease.
Drug treatment
Eye drops are the most common treatment for glaucoma. They lower intraocular pressure in two ways - by reducing the production of aqueous humor or improving its outflow through the angle of the anterior chamber.
Drops must be instilled daily. Like other medications, it is important to take them regularly as prescribed by your ophthalmologist. Never change or stop taking your medicine without talking to your doctor. If for some reason you are going to stop using it, ask your doctor what you can replace it with.
Surgery
Some patients are indicated for surgical treatment, which improves the outflow of intraocular fluid and reduces eye pressure.
Laser trabeculoplasty
. This surgery is often used for open-angle glaucoma. There are two types of trabeculoplasty: argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT).
During ALT, the laser creates thin, evenly distributed burns in the trabecular meshwork. It does not create new drainage holes, but stimulates the outflow system to operate more efficiently.
In SLT, the laser is used at different frequencies to allow operation at low power levels. In this case, a certain type of cell is affected, and the filtering channels, like a network surrounding the iris, remain intact. SLT may be effective in patients who have not been treated successfully with conventional laser surgery or eye drops.
Even if laser trabeculoplasty is successful, most patients continue to take the medications. For them, this method does not have a long-term effect. Approximately half of those who underwent this intervention again experience an increase in intraocular pressure within 5 years. Many patients who have had successful laser trabeculoplasty are forced to undergo it again.
Laser trabeculoplasty may also be used as a first-line option in those patients who are unwilling or unable to use antihypertensive eye drops.
Laser iridotomy
. Laser iridotomy is indicated for the treatment of patients with angle-closure glaucoma or a very narrow anterior chamber angle. The laser makes a small hole about the size of a pinhead in the upper part of the iris and thus improves the outflow of aqueous humor through the angle of the anterior chamber. This hole is hidden by the upper eyelid and therefore not externally noticeable.
Peripheral iridectomy
. When laser iridotomy is unable to relieve an acute attack of angle-closure glaucoma or is not possible for other reasons, peripheral iridectomy may be performed. A small section of the iris is removed, allowing intraocular fluid access to the drainage system of the eye. Because most cases of angle-closure glaucoma can be cured with glaucoma medications and laser iridotomy, peripheral iridectomy is rarely used.
Trabeculectomy
. During trabeculectomy, a small valve is formed from the sclera (the white tissue that covers the eye). A filter pad, or reservoir, is created under the conjunctiva, a thin tissue covering the sclera. Once formed, the pad appears as a bulge or bubble on the white part of the eye above the iris, usually hidden by the upper eyelid. As a result, aqueous humor can drain through the valve created in the sclera and collect in the pad, from where it will be absorbed by the blood vessels of the eyeball.
Ocular pressure is effectively reduced in 3 out of 4 patients who undergo trabeculectomy. Although regular checkups with an ophthalmologist are necessary, most patients do not need to use eye drops for a long time. If the newly formed filter channel closes or too much fluid begins to drain from the eye, additional surgery is necessary.
Surgical interventions using drainage devices (shunt surgery)
If trabeculectomy cannot be performed, surgery using drainage devices is usually successful in reducing intraocular pressure.
A shunt is a small plastic tube or valve connected at one end to a reservoir (a round or oval plate). It is an artificial drainage device implanted into the eye through a thin incision. When IOP increases above certain numbers, the shunt redirects aqueous humor into the sub-Tenon's space (under the Tenon's capsule covering the eyeball outside the palpebral fissure), from where it is absorbed into the bloodstream. When everything has healed, the reservoir can only be seen if you lift your eyelid when looking down.
Folk remedies
On the Internet you can find many recipes for treating glaucoma with decoctions and tinctures of herbs, vitamins, various lotions, etc. It is no coincidence that ophthalmologists have an extremely negative attitude towards such advice. Practice has not confirmed the effectiveness of folk remedies. Relying on them will only delay a visit to the doctor and the timely start of proper treatment. Meanwhile, the disease will progress, which will ultimately result in an increase in the degree of irreversible vision loss.
We answer your questions: how to slow down glaucoma?
Here you will find answers to questions:
1. What is glaucoma? Explain in simple words. 2. Why does glaucoma occur, what provokes its development? 3. What are the symptoms of glaucoma? 4. Why is glaucoma difficult to detect without testing? 5. What examination needs to be done to detect glaucoma? 6. I have glaucoma. How often should you visit an ophthalmologist? 7. Is glaucoma inherited? 8. What are the restrictions for patients with glaucoma? 9. Is it possible to completely cure glaucoma? 10. Is it possible to restore vision with glaucoma? 11. Is it possible to restore vision after an acute attack of glaucoma?
Answers your questions:
Nikandrova Olga Alexandrovna
Specialization: Diagnostics, glaucoma, diseases of the optic nerve and central retina Work experience: 8 years
Procedures:
more than 35,000
What is glaucoma? Explain in simple words.
Try focusing your gaze on the penultimate word of this sentence. At the same time, you simultaneously see out of the corner of your eye the space around your phone (computer). This is peripheral vision. It helps you not to stumble and to be on your guard if someone suspicious approaches you. Or see that a pedestrian has entered the roadway if you are driving. Glaucoma begins precisely by “stealing” our peripheral vision. The outflow of intraocular fluid becomes difficult, it accumulates and provokes an increase in intraocular pressure. The optic nerve is “squeezed” and the blood supply to the eye is disrupted. Increased stress on the optic nerve can cause it to atrophy, and visual images stop entering the brain. Vision, especially peripheral (side), begins to decline. The disease is dangerous because it can lead to irreversible blindness that cannot be treated, and this happens suddenly. At the same time, if diagnosed in time, glaucoma can be easily stopped: in the early and middle stages - with drops and simple procedures, in the late stage - with a simple operation. Therefore, the most important thing for glaucoma is to detect it in time and begin treatment.
Why does glaucoma occur, what provokes its development?
Among the main factors in the development of glaucoma:
- age over 40, the older you are, the higher the risk
- heredity
- severe myopia
- medium to high farsightedness
- diseases of the vascular system (atherosclerosis, coronary heart disease)
- eye injury
- diabetes
What are the symptoms of glaucoma?
If you notice any of these symptoms, please don't delay! Consult a specialist immediately to get the right treatment on time and avoid vision loss:
- blurring of the image before the eyes
- mild pain in the eye area, temple, above the eyebrow
- narrowing of the view on the sides
- the appearance of haze before the eyes
- light circles or rainbow spots around light sources
Why is glaucoma difficult to detect without testing?
Glaucoma is insidious in that it can affect up to 90% of your vision, and you won’t even notice it. The cerebral cortex has the amazing ability to fill in the gaps for which there was no information from the optic nerve with pictures from nearby areas. This natural mechanism deceives our perception and prevents us from noticing black areas of vision loss in time. And only when the “hole” in the visual field becomes so large that the compensation mechanism cannot fill it, the patient suddenly realizes that vision has deteriorated. Although, in fact, the deterioration began to occur long before that. That is why diagnostics using modern equipment is so important, allowing us to identify glaucoma at the earliest stages. When it will be enough to just prescribe special drops to cope with glaucoma.
What examination needs to be done to detect glaucoma?
Glaucoma is always accompanied by increased intraocular pressure. It sounds as if this is the only thing that needs to be measured for a correct diagnosis. In fact, only a complete comprehensive diagnosis can answer the question of whether there is glaucoma or not. A simple example: a patient has increased intraocular pressure and no other signs of glaucoma. This may be a symptom of an endocrine disorder and will require further testing to make a diagnosis.
Comprehensive vision diagnostics to identify glaucoma and check the effectiveness of prescribed treatment includes several types of studies:
- tonometry – measurement of intraocular pressure (3 types: Goldman tonometry, non-contact tonometry, contour dynamic tonometry), Pascal;
- perimetry - checking visual fields;
- gonioscopy – study of the anterior chamber angle;
- ophthalmoscopy - examination of the optic nerve head and retina;
- OCT – optical coherence tomography, layer-by-layer study of the retina and optic nerve head. Necessary for early diagnosis and follow-up.
I have glaucoma. How often should you visit an ophthalmologist?
Once the diagnosis is made, the ophthalmologist becomes your true ally in the fight against glaucoma. Schedule your visits to the ophthalmology clinic:
- to measure intraocular pressure – once every 1-3 months;
- to control the visual field – once every 3-6 months;
- to monitor the condition of the optic nerve – once every 6-12 months.
The frequency of examination is prescribed by the doctor individually for each patient. If necessary, the glaucomatologist will adjust the treatment by prescribing other eye drops or a combination of several drugs.
Is glaucoma inherited?
Unfortunately, glaucoma is indeed quite often inherited. Therefore, you should be especially attentive to your vision if you have close relatives with this diagnosis.
What are the restrictions for patients with glaucoma?
In addition to the personal recommendations on diagnostic results that you will receive from your doctor, there are some general tips:
- do not wear sweaters with a narrow neck, tight collars and ties - anything that can impede blood circulation in the neck area
- When working at a computer, with documents or when reading, take a break of 10-15 minutes every hour
- Night shifts, overtime work are undesirable, you cannot work in hot shops, with toxic substances, or in conditions of constant vibration
- try to quit smoking, it negatively affects intraocular pressure
- Avoid staying in a bent position or with your neck bent for long periods of time. For work in the garden (for example, weeding), adapt a bench.
Is it possible to completely cure glaucoma?
Unfortunately, vision loss from glaucoma is irreversible. Therefore, the main task of ophthalmologists is to identify it at the stage when increased intraocular pressure can still be compensated with special drops, procedures or simple surgery in order to protect the optic nerve and the flow of visual signals to the brain. In this case, good vision can please you for many years.
Is it possible to restore vision with glaucoma?
With glaucoma, vision deteriorates due to incipient atrophy of the optic nerve. If increased intraocular pressure is not treated in any way (with drops or procedures), then the process can occur especially quickly. Glaucoma treatment is mostly aimed at preserving existing vision. To achieve this, various procedures are performed to stimulate the optic nerve, as well as drops that control intraocular pressure. At later stages, an operation is prescribed, the essence of which is to create micropunctures to drain excess fluid from the eyeball and reduce intraocular pressure.
In any case, patients with glaucoma require a careful comprehensive examination. It is necessary to measure intraocular pressure once every 1-3 months, check the visual field once every six months, and conduct OCT of the optic nerve once a year. Depending on the results, your doctor will be able to create the most effective treatment plan for you. So that you can preserve your remaining vision for several decades.
Is it possible to restore vision after an acute attack of glaucoma?
An acute attack of glaucoma is always caused by a sharp increase in intraocular pressure. The main goal of ophthalmologists in this case is to reduce intraocular pressure as quickly as possible to restore normal blood circulation in the eye and adequate nutrition of the optic nerve. If treatment is incomplete or delayed, unfortunately, an irreversible decrease in visual acuity may occur due to the development of optic nerve atrophy. In such cases, treatment is prescribed in two directions: 1) reducing intraocular pressure to normal using drops, procedures or special surgery 2) treating optic nerve atrophy. It is, for the most part, aimed at preserving existing vision. For this purpose, procedures are used that stimulate the optic nerve, as well as drugs that improve metabolic processes in the eye, to ensure that the optic nerve receives adequate nutrition.
In any case, only an experienced glaucomatologist can determine a further strategy for preserving your vision, after all the necessary research.
Diagnostics
At the initial appointment, the ophthalmologist will carefully examine the eyes, ask the patient about warning symptoms, inquire about the medical history, and find out the risk factors that contribute to the manifestation of the pathology. In addition to this, he will carry out the following diagnostic procedures:
- Measure intraocular pressure using tonometry. All manipulations are simple and painless.
- Conducts testing for optic nerve damage using special instruments and equipment.
- Tests visual fields by examining features of the peripheral visual system.
- It will measure the thickness of the cornea (pachymetry), which will provide additional information in the diagnosis of glaucoma.
Dr. Trubilin’s clinic uses traditional and latest methods for diagnosing eye problems. An integrated approach is used for a comprehensive examination and making the most accurate diagnosis.
With us you can:
- undergo a visual acuity test;
- measure intraocular pressure;
- examine visual fields;
- do optical coherence tomography.
Additionally, biomicroscopy and gonioscopy of the affected area are performed. Based on the screening results, the doctor makes a diagnosis and prescribes individual treatment for glaucoma. When drawing up a scheme of restorative procedures, the patient’s age, medical history, as well as related details are taken into account.