Inflammation of the ovaries is a fairly common gynecological problem associated mainly with infection. It is one of the most relevant in clinical practice. The disease often becomes chronic, causes constant pain, negatively affects a woman’s menstrual, sexual, and reproductive function, and worsens her general well-being and emotional and mental state. Timely correct diagnosis and earlier initiation of treatment are of great practical importance.
Inflammation of the ovaries - what is it?
In the medical community, ovarian disease that develops as a result of inflammation is given the name “oophoritis.” If it is combined with inflammation of the fallopian tubes (also fallopian tubes, oviducts), then the term “salpingoophoritis” is used - this is how inflammation of the appendages is designated. In ICD-10 they are included in the section “Inflammatory diseases of the pelvic organs” and form a separate category “Salpingitis and oophoritis”, which is assigned code N70. Oophoritis can be unilateral or bilateral, when both glands are affected at once.
Features of the chronic form of inflammation
If inflammation becomes chronic, it periodically worsens. Usually the cause is colds or infectious diseases, physical or mental stress, digestive disorders, and diseases of the genitourinary system. If a woman smokes or drinks alcohol frequently, the risk of exacerbations increases.
In some cases, relapses of the disease do not occur; the woman is only worried about discharge and irregular menstruation. This course of ovarian inflammation is typical, for example, with gonorrhea. However, gradually thickening of the walls of the fallopian tubes occurs, and the formation of adhesions in the ovaries. With a unilateral process, the pain is localized at the site of inflammation. If it occurs on the right side, then the symptoms of oophoritis may be confused with the symptoms of appendicitis. A thorough diagnosis of the disease is required.
Often inflammation that occurs on one side spreads to the second ovary. In women suffering from chronic inflammation of the ovaries, a common symptom is the presence of constant scanty discharge (leucorrhoea). Typically, patients consult a doctor for examination and treatment if pregnancy does not occur.
Pathogenesis
As an independent disease, oophoritis is extremely rare; it often develops as a secondary form caused by previous infection and the development of inflammatory processes in neighboring structures. The rarity of isolated inflammation of the ovaries is explained by the fact that the ovaries themselves are reliably protected by a dense protein membrane. Since the pelvic organs are compactly located and are a functional whole, there is a high probability of penetration (spread) of infection. It enters through the bloodstream, lymph from anatomically distant organs, from the infected intestines, lungs, genitourinary system, abdominal cavity, but more often there is an ascending route of infection - from the vagina, through the cervix, fallopian tubes.
Main signs of the disease
The pathology does not have specific symptoms, which significantly complicates its diagnosis. As a result, the infectious process spreads to healthy tissue, the surface of which becomes deformed and becomes covered with adhesions and scars. In advanced cases, pathological changes affect internal organs located in the abdominal cavity. Therefore, if a woman notices suspicious symptoms that are uncharacteristic of her usual state, it is better not to wait until her health returns to normal on its own, but to visit a doctor as soon as possible and get tested.
Pain in the lower abdomen
This symptom mainly accompanies acute inflammatory processes. Infection leads to swelling and enlargement of the ovaries, causing nearby nerve fibers to be compressed and irritated. This entails painful discomfort of varying degrees of intensity. Locations of pain:
- suprapubic region;
- crotch;
- lumbar spine;
- inner thighs.
If there is chronic inflammation of the left or right ovary, the pain is first localized in the corresponding side of the diseased organ. But as the inflammation progresses, the pain syndrome spreads to the entire abdominal area.
Increased body temperature
A rapid increase in temperature is a characteristic sign of a progressive infectious-inflammatory process. Fever is the body’s natural immune response to a foreign infection. When the temperature rises, unfavorable conditions are created that suppress the active activity of pathogenic organisms.
Digestive system dysfunction
The progression of infection in the body leads to severe intoxication, which becomes the main cause of disruption of the functioning of the digestive system. Poisoning by decay products of pathogenic microflora causes the following pathological symptoms in oorphitis:
- nausea accompanied by bouts of vomiting;
- intestinal disorder.
Often such symptoms blur the true clinical picture of the disease. The patient thinks that she has poisoning, for which she begins to take appropriate medications, without rushing to seek medical help. However, with inflammation of the ovaries, taking absorbents does not bring the desired effect, the symptoms rapidly worsen, which should alert the woman.
Unpleasant discharge from the genital tract
If a woman does not have any problems with the health of the reproductive system, her vaginal discharge does not have foreign inclusions or an unpleasant odor. With bacterial inflammation of the ovaries, the nature of the discharge changes and it can be used to determine that something is wrong with the body.
Pathological discharge with orrfit is:
- Purulent. The presence of purulent inclusions in vaginal discharge is a sign of a bacterial infection and progression of complications. If there is no treatment for the disease, the risk of developing sepsis and the spread of infection throughout the body increases, which very often causes death.
- Serous. They are concerned when ovarian tissue is damaged by a viral infection that affects the body and cervix.
- With bloody inclusions. The presence of blood clots in vaginal discharge indicates a violation of the integrity of the blood vessels located in the organ.
Menstrual irregularities
Disruptions in the menstrual cycle may indicate various gynecological pathologies. With inflammation of the ovaries, menstrual irregularities manifest themselves as follows:
- complete absence of menstrual bleeding;
- heavy or scanty bleeding;
- long breaks between menstruation;
- sharp, intense pain in the lower abdomen.
Such disorders arise as a result of malfunctions of the ovaries due to inflammation and the development of hormonal imbalance.
Pain during sexual intercourse
Inflammation of the organs of the reproductive system leads to the formation of edema, as a result of which the ovaries increase in size, squeezing and irritating nearby nerve structures. With orphitis, a woman is bothered by acute pain, which intensifies during sexual intercourse.
Pain during sexual intercourse may be due to a lack of vaginal lubrication, which is no longer produced in sufficient quantities as a result of hormonal imbalance.
Hormonal disorders
Ovarian dysfunction caused by infectious processes leads to hormonal imbalance, in which the body experiences a deficiency of such important female hormones as:
- estrogen;
- progesterone.
You can suspect that you have hormonal imbalances based on the following symptoms:
- decreased sexual desire;
- sudden mood swings;
- causeless surges in blood pressure;
- weight gain with the usual diet;
- infertility.
Hormonal disruptions are most often observed with chronic bilateral oorphitis. In this case, long-term, complex treatment carried out under the strict supervision of a doctor will help correct the pathology.
Infertility
Often, a long-term inflammatory process in the ovaries causes disruption of egg maturation. It is not possible to conceive a child if inflammation of the fallopian tube is associated with oorphitis. The progression of the pathology leads to a narrowing of the lumen of the fallopian tube, which, if left untreated, sooner or later leads to obstruction, which becomes the main cause of infertility.
Inflammation of the ovaries during pregnancy
Oorphitis significantly reduces the chances of conceiving and safely bearing a child. In the chronic course of the inflammatory process, adhesions and scars are formed, which prevent the normal movement of sperm through the fallopian tubes and fertilization of the egg. Therefore, even at the stage of pregnancy planning, it is necessary to diagnose and treat the disease. Once ovarian function is restored, a woman will be able to get pregnant without problems and carry a healthy child.
Inflammation of the ovaries during menopause
Women who are in menopause are no less susceptible than others to infectious and inflammatory complications affecting the ovaries and nearby organs of the reproductive system. During this period, the mucous layer of the vagina becomes thin, which is why it ceases to fully perform its protective functions. Infections that enter the vagina can easily spread to neighboring tissues, affecting the reproductive organs, causing inflammation and related complications.
Causes
Depending on the etiology of inflammation of the ovaries, they are divided into 2 groups:
- Specific processes - occur against the background of tuberculosis, mycoplasmosis, venereal disease (most often it is gonorrhea, genital herpes, trichomoniasis, chlamydia, and their combinations are also found).
- Nonspecific inflammation - caused by the penetration of opportunistic organisms, septic diseases, appendicitis. The main culprits: Escherichia coli, staphylo-, strepto- or pneumococci, enterococci, microorganisms of the genus Candida, clostridia, etc.
Predisposing factors for the development of oophoritis include childbirth, abortion, increased sexual activity, intrauterine contraception, and other interventions on the uterus.
The list of factors that provoke exacerbation of existing inflammation includes:
- general hypothermia of the body, swimming in cold water;
- inadequate or insufficient nutrition;
- prolonged stress;
- severe fatigue;
- weakening of the immune system.
Prevention
In order not to encounter inflammation of the appendages and complications of the disease, it is necessary to follow preventive measures:
- visit a gynecologist every 6-12 months;
- maintain personal hygiene, do not use other people’s towels;
- refuse casual sex;
- avoid stressful situations;
- do not overcool your body;
- do not abuse alcoholic beverages or spicy foods;
- treat all diseases in a timely manner;
- use a condom during sexual intercourse.
In conclusion, it is worth noting that salpingoophoritis is a pressing problem for many modern women. Only careful attention to your body can protect you from this disease and the consequences of inflammation of the uterine appendages. If salpingo-oophoritis makes itself felt, then you should seek qualified medical help as soon as possible.
Symptoms of ovarian inflammation
There are acute, subacute inflammation and chronic recurrent inflammation. In the acute course, the clinical picture is most pronounced, the patient is concerned about:
- severe pain in the depths of the pelvis, often radiating to the lower back;
- urination disorder;
- tense stomach, painful touch;
- spotting or purulent discharge (not in all cases);
- general phenomena - nausea, flatulence, fever, weakness, headache.
In the subacute phase, symptoms subside. Chronic oophoritis manifests itself:
- aching pain, aggravated by tension, during menstruation;
- pain radiating along the branches of the nerve;
- heavy or scanty periods, cycle failure;
- sexual desire disorder;
- painful sexual intercourse.
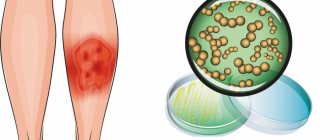
Gardnerellosis
The disease is not an STD. It is caused by gardnerella vaginalis, and, in fact, gardnerella is a manifestation of vaginal dysbiosis. That is, this is not inflammation in the vagina. That is why this disease is also called bacterial vaginosis.
Unlike other infections, with gardnerellosis the symptoms are pronounced and specific. Symptoms include heavy, thin vaginal discharge that is white or yellowish in color and has a very unpleasant odor, similar to rotten fish. This odor may become stronger during and after menstruation, as well as after sexual intercourse. This disease causes discomfort and burning in the external genital area.
During a gynecological examination, an experienced doctor will be able to immediately make a diagnosis, since the discharge has a slightly foamy characteristic appearance. In some cases, there may be no symptoms, so gardnerella can only be detected during an examination.
Gardnerella is located directly in the vagina. This infection most often does not penetrate further, therefore there are no symptoms such as, for example, pain in the lower abdomen.
Gardnerella and pregnancy
Gardnerella can cause a lot of trouble during pregnancy. It is possible, although very rare, that intrauterine infection may occur. Gardnerella can also cause inflammation of the uterus after childbirth or abortion. That is why bacterial vaginosis during pregnancy must be treated immediately when it is detected.
Gardnerella usually appears in a simple smear on the flora. The PCR diagnostic method is also used to identify them.
Treatment
Treatment is carried out in 2 stages. First, the infection is destroyed, and then the microflora in the vagina is restored.
At the 1st stage, drugs such as flagyl, fasigin, clindamycin, trichopolum are used.
The 2nd stage is longer, it can last 1 month or even more. Here you need to be patient, because... If the microflora is not restored, the disease will return again. Sexual activity during the treatment period is possible, but only if the partners use a condom.
In men, gardnerella “takes root” and does not develop, so treatment of sexual partners is not required.
Diagnosis
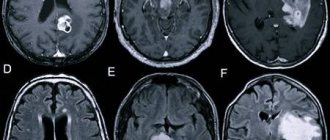
Recognizing oophoritis is a complex process, because Its manifestations are similar to many diseases. To establish the transition of inflammation to the ovaries, the gynecologist:
- Interviews the patient - interested in past illnesses, birth history, presence of abortions, symptoms, duration of course.
- Conducts an examination - palpation, manipulation with a mirror.
- Refers for laboratory testing - analysis of vaginal secretions, blood, urine, urethral smear, bacterial culture.
- Uses instrumental methods - hysterosalpingography, ultrasound OMT, fallopian tubes (USGSS).
- He resorts to additional methods - tuberculin diagnostics, PCR analysis, ELISA, laparoscopy.
Diagnostics
Clinical manifestations of ovarian inflammation may be similar to signs of endometriosis, cystic formations and even ectopic pregnancy. Therefore, at the first suspicious symptoms, first consult a doctor so that he can conduct a differential diagnosis and make an accurate diagnosis.
Examination for ovarian inflammation includes the following procedures:
- laboratory tests of blood and urine, which during the inflammatory process show a high level of leukocytes;
- smears from the vagina, urethra;
- gynecological examination, allowing to suspect inflammation in comparison with the ovaries, pain syndrome and changes in the area of the uterine appendages;
- ELISA, PCR - these are those who have hidden infectious diseases;
- ultrasound examination of the pelvic organs;
- laparoscopy, which allows you to obtain reliable information about the condition of the fallopian tubes and uterus, make an accurate diagnosis, and detect tubal infertility;
- Salpingoscopy is used for gross anatomical abnormalities and changes in the fallopian tubes.
Based on the results of a comprehensive diagnosis, a clinic gynecologist can make an accurate diagnosis by detecting concomitant diseases, including hidden infections.
Treatment
Severe forms are treated in a hospital. Therapy is conservative, long-term. The course is selected individually. The range of measures taken usually includes:
- drug therapy - antibiotics, anti-inflammatory drugs, immunomodulators, vitamins, eubiotics;
- hot douching, ichthyol suppositories, Longidaza;
- physiotherapy – mud, diathermy, ultraviolet irradiation, inductothermy, massage.
Indications for surgery include pain, purulent inflammation, adhesions, and peritonitis.
Treatment of adnexitis - antibiotics, surgery
The healing process depends on the type of inflammation of the appendages, the patient’s condition and the complications listed above. The basis of treatment for an acute condition is urgent hospitalization and intensive antibacterial therapy. An antibiotic for adnexitis must have a wide spectrum of action. Initially, the drugs are administered intravenously, then administered orally. The gynecologist will also prescribe a diet and apply cold compresses to the abdomen.
Surgery for inflammation of the appendages is used in case of failure of conservative treatment, deterioration of the patient’s condition, or the appearance of symptoms of peritonitis. Antibiotics are also used for chronic and sub-spatial conditions. Only complications of the resulting inflammation of the appendages are operated on. The most dangerous of them is peritonitis, caused, for example, by rupture of an ovarian abscess.
In life-threatening conditions, surgeons use an open surgical method, which consists of a wide incision in the abdominal tissue and cleansing the abdominal cavity of pus. For less serious complications, such as a fallopian tube cyst, laparoscopy may be used.
Treatment of inflammation of the appendages with home remedies is ineffective, and any attempts to use natural methods, including herbs, can only do harm and delay a visit to the gynecologist.
Classification
Inflammation of the appendages is classified as follows:
| By localization | With the flow | By pathogen type |
| Left-handed | Acute – abrupt onset, severe symptoms. Recovery in a few days | Bacterial – caused by different groups of bacteria |
| Right-handed | Subacute – lasts several days or months | Fungal – the cause is a fungal infection |
| Two-way | Chronic – occurs if acute inflammation is not treated. Characterized by an undulating course, unexpressed symptoms |
Stages and stages of development
Salpingo-oophoritis most often affects both appendages, but sometimes a left-sided or right-sided pathological process occurs. It is extremely important for doctors to promptly determine not only the location of the pathology, but also its form. There are acute or chronic forms:
- Spicy . Characterized by extremely severe symptoms. Body temperature rises sharply and fever develops. Blood pressure decreases.
- Chronic . Usually appears within a month as a result of improper treatment of the acute stage of the disease. Symptoms are vague, subfertile temperatures and minor pain in the abdominal area are possible. Sometimes an exacerbation occurs due to internal or external factors.
Some gynecologists distinguish the so-called subacute form of the disease, when the symptoms are moderate in nature.
Regardless of the form of the pathology, doctors distinguish several main stages of the development of the disease:
- Toxic . Intoxication of the body. Duration – 1-1.5 weeks. If the doctor selects the right therapy, recovery occurs. If not, the disease moves to the next stage.
- Septic . Determined by deterioration of the patient's condition. The pain intensifies, the purulent discharge increases. The inflammatory process may spread to other pelvic organs.
Complications
Inflammation of the appendages develops rapidly.
If not treated in time, it can become complicated by the following pathological conditions:
- various forms of menstrual cycle disorders. Oligomenorrhea occurs in 3% of women who have recovered from the disease;
- pain syndrome;
- hydrosalpinx - sacs with fluid;
- pyosalpinx - purulent exudate (in the tube), pyovar (ovary);
- cicatricial adhesive process;
- tubo-ovarian tumor - the tube enlarges due to the accumulation of pus and becomes similar to a tumor. It has nothing to do with neoplasm;
- hypofunction, ovarian depletion;
- sexual dysfunction;
- hormonal imbalance;
- damage to the pelvic tissue.
- ectopic pregnancy (up to half of cases).
Infertility is the most severe consequence of inflammation for women of childbearing age. The most dangerous thing is an abscess. It can lead to rupture of the fallopian tube. If purulent contents enter the abdominal cavity, peritonitis will develop. This is a life-threatening condition that requires immediate surgery.
How to prevent it?
To reduce your risk of developing pelvic inflammatory disease, you should follow these tips.
Practice safe sex - use condoms every time and limit the number of partners.
Get tested – If you have been exposed to a sexually transmitted infection, make an appointment at the office and get the necessary tests done. If necessary, agree with your doctor on a regular screening schedule. Early detection and treatment of sexually transmitted diseases gives a much better chance of avoiding pelvic inflammatory disease.
Ask your partner to get tested – If you have pelvic inflammatory disease or other sexually transmitted diseases, ask your partner to get tested and possibly treated for them. Thus, you limit the spread of sexually transmitted diseases, and also reduce the risk of relapse of pelvic inflammatory diseases.
Stop rinsing the vagina - rinsing disrupts the very delicate bacterial balance in the vaginal environment.
Inflammation of the pelvic organs - causes
There are quite a few causes of inflammation “female-style”:
- Unprotected sexual intercourse
. Increases the risk of developing sexually transmitted diseases and, consequently, the development of pelvic inflammatory diseases. - Some methods of contraception.
May influence the likelihood of developing pelvic inflammatory disease. An intrauterine device can increase the risk of getting the disease, while using condoms reduces the risk. Using birth control pills without other forms of protection does not guarantee any protection against sexually transmitted diseases, but they do increase protection against the development of pelvic inflammatory disease by thickening the cervical mucus and thereby preventing bacteria from entering the upper genital tract. - Gynecological manipulations.
Bacteria can also enter the genital tract during an IUD procedure, childbirth, miscarriage, abortion, or a biopsy of the lining of the uterus, which involves removing a small piece of tissue lining the uterus for laboratory analysis.