Stroke is one of the most common and serious diseases of the central nervous system. Stroke occurs regardless of gender and age. However, stroke in representatives of the stronger sex also has its own characteristics.
1. Signs and symptoms of stroke in men
2. First signs of stroke in men
3. First aid
4. Treatment and prevention
Representatives of the stronger sex are most at risk after the age of 40. The presence of diabetes mellitus, poor heredity, cardiac arrhythmia, hypertension, atherosclerosis and previous myocardial infarction significantly increase the risk of developing ischemic stroke. Lifestyle is equally important. Thus, constant stress, impaired metabolism, alcohol abuse, unhealthy diet, excess weight, physical overload, lack of sleep - all this negatively affects the functioning of the central nervous system and poses a serious threat to health.
What is a stroke
The essence of a stroke is the cessation of blood supply and functioning of a part of the brain as a result of damage to a vessel.
The larger the affected area, the more severe the stroke. Necrosis of a portion of the brain substance is called an infarction [3]. There is a high risk of death in the first few hours, and then in the period up to 28 days after a vascular accident. The annual mortality rate from stroke in the Russian Federation is 374 cases per 100,000 [10]. In 2018, 35% of patients died in the acute period of stroke; by the end of the first year, this figure increases by 15%, and in general, in the first 5 years, the mortality rate of strokes is 44% [11]. The mortality rate from stroke was 92.9 per 100,000 population, and the hospital mortality rate was 19.1% [5].
Long-term disability is most likely for patients who have suffered a stroke. The prevalence of primary disability due to stroke in 2018 was 3.2 per 10 thousand population [2]. Of these, 31% need constant care, 20% have severe mobility limitations, and only 8% return to work [3]. The prevalence of recurrent strokes in 2014 was 0.79%, of which ischemic
strokes account for 87.5% [9].
Who is at risk
There are people who need to be especially wary of developing a stroke, as they are at risk.
Among them:
- Persons with hypertension.
- Patients with diabetes.
- Men and women over 65 years of age.
- People with abdominal obesity.
- Persons with a hereditary predisposition to vascular pathologies.
- Patients who have previously had a stroke or heart attack.
- Patients with diagnosed atherosclerosis.
- Women over 35 years of age taking oral contraceptives.
- Smokers.
- People suffering from heart rhythm disturbances.
- People with high cholesterol levels.
Most often, patients with the listed diagnoses are registered at the dispensary. Special mention should be made of people living in a state of chronic stress. Emotional stress negatively affects all systems of the body and can cause a stroke.
Causes of stroke
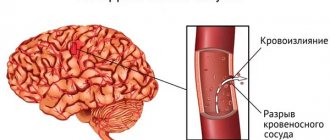
Depending on the cause of cerebrovascular accident, ischemic and hemorrhagic strokes are distinguished.
Ischemic stroke occurs as a result of blockage of cerebral vessels by a blood clot, when gradually less and less blood flows to an area of the brain. Hemorrhagic stroke develops as a result of rupture of a vessel and hemorrhage in the brain tissue, as a result of which the blood supply to its area abruptly stops. Hemorrhage can be into the subarachnoid space (SAS) or directly into the cerebral substance (ICH). The ratio of ischemic and hemorrhagic strokes is 4-5:1 [4].
Pathologically, a stroke can be cardioembolic, lacunar, atherothrombotic, or another, including unknown, etiology (TOAST classification) [10].
Predisposing factors:
- men from 45 to 59 years old;
- age 70 years and older (for both sexes) [4];
- arterial hypertension;
- atrial fibrillation;
- atherosclerosis of cerebral vessels;
- coagulopathy, thrombophilia, anemia;
- arteriovenous malformations;
- osteochondrosis with damage to the vertebral artery;
- brain tumors;
- dyslipoproteinemia;
- obesity;
- diabetes;
- intermittent claudication;
- mechanical prostheses of heart valves and blood vessels;
- IHD, myocardial infarction less than 6 months before the stroke;
- other cardiac diseases;
- smoking, alcoholism;
- family history of stroke;
- sedentary lifestyle;
- stress [1, 3].
Features of stroke in women
If in men the most likely risk of stroke is after 40 years, then in women this probability reduces the age limit to 18 years. The main reason for this fact is that physiologically women are more prone to aneurysm (a feature of the structure of the vessel with congenital expansion). Constant stress, high blood pressure, and emotional experiences lead to ruptures in the walls of blood vessels, and hemorrhage occurs in the cranial cavity.
During pregnancy and childbirth, as well as hormonal changes, there is a lot of stress on the body. This in turn greatly affects the blood circulation process in the brain. Some symptoms of eclampsia and preeclampsia are mistaken for ischemic ones. Such atypical symptoms of a stroke can significantly delay the provision of first aid to the victim and create a life-threatening situation for further treatment of the consequences of a stroke.
Contraceptive drugs increase the risk of vascular thrombosis significantly. Since the use of such drugs for a long time affects blood clotting.
Signs of an incipient stroke
The onset of a hemorrhagic stroke is characterized by the following symptoms:
- severe headache;
- increased blood pressure;
- vomit;
- dizziness;
- loss of consciousness;
- weakness in the limbs;
- visual impairment;
- seizures [1].
The onset of ischemic stroke is gradual; within an hour, some of the following symptoms appear:
- facial asymmetry, numbness;
- difficulty speaking – incoherent, impaired understanding;
- double vision, visual disturbances;
- headache;
- numbness, limited mobility in the limbs, often on one side;
- dizziness, imbalance, staggering, staggering gait;
- confusion with disorientation, subsequently there may be loss of consciousness [3].
If one or more of these signs appear, you should:
- Sit the patient down, providing access to fresh air.
- Call emergency medical help immediately.
- If the patient is conscious and able to chew and swallow, give him one aspirin tablet.
The patient must be hospitalized in a neurological or neurosurgical department, where stroke treatment will be carried out. The sooner the patient is in the hospital, the more effective the therapy.
First signs and symptoms
Before a stroke, drowsiness, headache, numbness of the limbs, fatigue, spots before the eyes, nausea, dizziness, temperature fluctuations, and blood pressure jumps appear. These are the harbingers or first signs of a stroke that appear several hours or days before the disaster. Most often, these symptoms are ignored, or they are attributed to fatigue and overwork.
Symptoms of a stroke themselves are divided into general cerebral and focal. They can be of varying degrees of severity depending on the prevalence of the pathological process.
- General cerebral symptoms: headache, impaired consciousness up to loss of consciousness, stupor, agitation or weakness, disorientation in space and time, sweating, feeling hot, convulsions. Makes you feel sleepy and sometimes chills.
- The focal abnormalities of a stroke depend on which area of the brain is affected. They can be unilateral or bilateral. This group includes disturbances in speech, vision (visual hallucinations), gait, movements up to paralysis, and sensitivity.
Symptoms of ischemic cerebral stroke develop gradually, with focal symptoms predominant.
With a hemorrhagic stroke, the onset is rapid, with a predominance of cerebral symptoms.
There are several stages in the development of a stroke: the acute period (from the moment of the stroke to 3 weeks on average), the recovery period - from 2 weeks to 24 months.
Symptoms of a stroke
Stroke leads to various brain injuries, depending on the location of the lesion and the pathological type of cerebrovascular accident:
- disturbances of movement in the limbs: from restrictions (paresis) to complete paralysis. When the lesion is localized on the right, the left limbs suffer; with a left-sided lesion, right hemiparesis is formed; in some cases, movements in all limbs may stop (tetraparesis or double hemiparesis);
- sensory disturbances on one or both sides;
- speech disorders (dysarthria - poor articulation; aphasia - inability to pronounce and understand words, write and read);
- ataxia (impaired coordination of movements, “overshooting”, unsteadiness, imbalance, tremor);
- visual impairment: from blindness to double vision and gaze paresis;
- hearing impairment and dizziness;
- violation of mental functions (consciousness, thinking, attention, memory, will, behavior);
- paresis of the soft palate and pharynx, swallowing disorders;
- disorders of urination and defecation;
- depression of respiration and vascular tone;
- increased intracranial pressure;
- patients complain of headaches, vomiting, hiccups, yawning, shoulder pain;
- consciousness is gradually depressed to the point of coma [1, 3].
Causes of death may include cerebral edema, pneumonia, heart failure, and recurrent stroke. In severe cases, “locked-in syndrome” may develop: the patient is conscious, but cannot move, swallow or speak [3].
First aid
If the victim shows one or more of the above signs, then you need to call an ambulance. It is prohibited to give the victim any medications at this time. The man must be laid on a flat surface with his head slightly raised. A cold compress is applied to the back of the head, and a heating pad is applied to the lower extremities. It is important to ensure that the victim is in a state of complete rest, not allowing him to move or stand up abruptly. If a person is indoors, open the windows to allow fresh air to flow in. When vomiting occurs, tilt your head to the sides so that he does not choke. At the first signs of clinical death, artificial respiration and chest compressions are performed.
Consequences of a stroke
There are transient ischemic attack (less than a day), minor stroke (from 1 day to 3 weeks) and stroke with persistent residual effects. The consequences of a stroke are expressed mainly in motor and sensory disorders, the formation of muscle contractures (pronounced constant restriction of movements in the joints), speech and swallowing disorders. General symptoms may also remain, including confusion, disturbances in thinking, will, and emotional regulation. Complications can develop: from epilepsy to bedsores, encephalopathy and anxiety-depressive syndrome [1, 3].
Diagnosis of strokes
First of all, it is necessary to conduct a detailed neurological examination. Instrumental diagnostic studies and laboratory tests are also prescribed. In case of a stroke, in the first hours, an MRI or CT scan of the brain is performed, if necessary, CT or MR angiography, color Doppler mapping of blood flow, ECG or Holter monitoring, echocardiography as indicated, monitoring of blood pressure, saturation, assessment of the risk of developing bedsores, assessment of swallowing function [ 1, 3, 6].
Tests for stroke
- Complete clinical blood test, including erythrocyte sedimentation rate (ESR).
- Biochemical blood test with determination of C-reactive protein and homocysteine, glucose level, platelet count, activated partial thromboplastin time, INR.
- Interleukin 10.
- Extended coagulogram.
- Determination of acid-base status.
- General urine analysis.
To prepare for neurosurgical intervention, a blood test is additionally performed for hepatitis, syphilis, HIV, blood group and Rh factor determination.
Stroke is an acute disruption of the blood supply to the brain that occurs as a result of rupture or blockage of a cerebral vessel. In this case, the flow of blood to a certain part of the brain is significantly reduced or stopped.
Blood brings oxygen and nutrients to the nerve cells of the brain, which are necessary for normal functioning. During a stroke, the supply of oxygen and nutrients to brain cells is stopped, which leads to their death within a few minutes.
A stroke is characterized by loss of consciousness, disturbances in movement, speech, and loss of sensation in a certain part of the body. Early treatment can reduce brain damage and improve the prognosis of the disease. Control of blood pressure, cholesterol levels, smoking cessation and alcohol abuse are of great importance in the prevention of stroke.
Synonyms Russian
Acute cerebrovascular accident, apoplexy.
English synonyms
Cerebrovascular accident, stroke.
Symptoms
- Intense headache, which may be accompanied by nausea and vomiting.
- Loss of consciousness.
- A sudden feeling of numbness in the skin on the face, torso, arm, or leg on one side.
- Sudden weakness in the muscles of the arms, legs, and torso, mainly on one side.
- Speech impairment. There may be difficulties in pronouncing words or sounds, or in understanding speech.
- Visual impairment: double vision, decreased visual acuity.
- Convulsions - in rare cases.
General information about the disease
There are two main types of stroke: ischemic and hemorrhagic. The most common is ischemic - about 80% of cases. It occurs when an artery becomes blocked (for example, by a blood clot) and blood flow through that artery stops or suddenly decreases. In the absence of blood supply to the area of the brain that receives blood from this artery, nerve cells die.
The second type of stroke is hemorrhagic. It develops when a blood vessel in the brain ruptures, resulting in bleeding in the brain.
Depending on the cause, ischemic stroke is classified into the following types.
- Thrombotic stroke is when an artery blockage occurs due to the formation of a thrombus (blood clot) in one of the arteries supplying blood to the brain. A blood clot forms on the walls of arteries that contain atherosclerotic plaques (deposits of cholesterol and other fats). The plaque narrows the lumen of the vessel, and a blood clot forms around it. The narrowing of the lumen of the vessel leads to a decrease or cessation of blood supply to an area of the brain, which causes a stroke.
- Embolic stroke - develops when emboli (blood clots, fat particles, air) form at a distance from the brain, which, with the blood flow, enter narrower vessels of the brain, causing their complete or partial blockage. Emboli are often formed due to cardiac arrhythmias, heart defects and other diseases.
Hemorrhagic stroke occurs for many reasons, mainly due to high blood pressure and weak spots in the blood vessels of the brain (aneurysms and malformations).
- Aneurysm rupture. A cerebral aneurysm is an enlargement of the vessel with thinning of its walls. When blood pressure increases, the vessel in this place is damaged and hemorrhage occurs in the brain.
- Rupture of arteriovenous malformation. Arteriovenous malformation is a tangle of thinned vessels that are normally absent. This pathology increases the risk of cerebral hemorrhage.
Depending on the location of the vessel, hemorrhage can occur in the substance of the brain or between the brain and its membranes. If the ruptured vessel is located in the substance of the brain, intracerebral hemorrhage occurs, if closer to the surface of the brain - subarachnoid hemorrhage (between the brain and its membranes). In both cases, severe damage and disruption of brain activity occurs, which causes a serious condition for the patients.
Sometimes symptoms of a stroke appear. The difference is that they pass quite quickly (sometimes within a few minutes). This can occur as a result of a temporary decrease in blood flow in a vessel in the brain, and this condition is called a transient ischemic attack. The mechanism of development is the same as for ischemic stroke, but with a transient ischemic attack, significant brain damage does not occur, since circulatory disorders are temporary. Despite the complete disappearance of symptoms, a transient ischemic attack requires examination and treatment, as it may be a precursor to a stroke.
Patients who have suffered a stroke may have serious disabilities that require long-term rehabilitation. These include:
- decreased strength or complete lack of movement (paralysis) in the muscles on one side of the body;
- memory impairment;
- speech disorders;
- disturbances in chewing and swallowing food;
- behavior change.
These disorders occur when certain areas of the brain that are responsible for these functions are damaged during a stroke. The severity of these disorders and the possibility of restoring lost functions depend on the degree of brain damage.
Who is at risk?
- Persons over 55 years of age.
- Those whose relatives have suffered a stroke.
- People with high blood pressure.
- People with high cholesterol levels.
- Patients with diabetes.
- Alcohol abusers, smokers.
- Obese people.
- Leading a sedentary lifestyle.
- Taking contraceptives or hormonal medications containing estrogens.
Diagnostics
Diagnosis of stroke consists of brain studies (computed tomography, Doppler ultrasound, etc.) aimed at establishing the type of stroke, volume, and area of brain damage. The serious condition of patients with stroke requires careful monitoring of many laboratory parameters of blood and urine.
The following tests are used to assess your risk of stroke.
- General blood analysis. Allows you to determine the number of red blood cells, platelets, leukocytes, hemoglobin content in red blood cells. Assessing these indicators is important to identify possible causes of stroke. A decrease in the number of red blood cells and hemoglobin (anemia) interferes with the delivery of oxygen and promotes hemorrhage.
- Erythrocyte sedimentation rate (ESR). An increase in ESR may indicate inflammatory processes in the body, including inflammatory changes in the walls of blood vessels (arteritis), which can play a role in the occurrence of stroke.
- General urine analysis with microscopy. Allows you to characterize various properties of urine (color, density, protein, glucose, bilirubin) and identify inflammatory changes in the organs of the urinary system. Glucose can appear in the urine in diabetes mellitus, and one of the reasons for the increase in protein levels in urine is hypertension. These diseases are risk factors for stroke.
- Blood glucose. Glucose is the main type of carbohydrate that is used as a source of energy in the body. Its concentration is often increased in diabetes mellitus.
- Cholesterol – low density lipoproteins. They deliver cholesterol to the organs and tissues of the body. An increase in their number contributes to the development of atherosclerosis (deposition of atherosclerotic plaques on the walls of blood vessels).
- Coagulogram is an analysis of the blood coagulation system. Among the coagulation parameters are indicators of INR (international normalized ratio), aPTT (activated partial thromboplastin time), etc. An increase in INR and aPTT indicates hypocoagulation, that is, a decrease in the ability of blood to clot (tendency to bleed), a decrease in these indicators indicates an increased risk thrombosis. Taking into account the coagulogram is important for the prevention of stroke and for assessing the effectiveness of taking anticoagulants (drugs that prevent the formation of blood clots).
Brain Research
- Computed tomography plays a leading role in the diagnosis of cerebral stroke. The method is based on changes in the intensity of X-ray radiation when passing through media of different densities. Special sensors record these changes, and after computer processing, layer-by-layer images of the body’s structures are formed. With the intravenous administration of a special contrast agent, the vessels of the brain can be examined. This study allows us to identify the type of stroke, the volume and area of brain damage, as well as changes in blood vessels.
- Magnetic resonance imaging is based on the action of a strong magnetic field on human tissue. As a result, after computer processing, layer-by-layer images of internal organs are obtained, so that the volume of damaged brain tissue during an ischemic stroke can be determined.
- Angiography allows you to see the blood vessels of the brain. Through a small incision, a special catheter is inserted into the femoral artery, which is then passed through large vessels into the carotid or vertebral artery and then from these arteries to the vessels of the brain. During the manipulation, a contrast agent is passed through the catheter, visible in X-rays. After introducing a contrast agent into the vessels, their image is obtained in a series of photographs.
- Doppler ultrasound is based on the use of ultrasound. With its help, narrowing of the lumen of blood vessels, atherosclerotic plaques are identified, the speed of blood flow in the vessels and other important indicators are determined.
Additional Research
- Echocardiography is an ultrasound method for examining the heart. Allows you to obtain an image of the heart and identify emboli, which can travel through the bloodstream to the brain and cause a stroke.
Treatment
The treatment approach depends on the type of stroke. In an ischemic stroke, the main task is to restore blood supply to the affected area of the brain. For this purpose, blood thinners are used to help dissolve blood clots. In order to prevent ischemic stroke, the following operations can be performed in the future:
- carotid endarterectomy - an operation aimed at removing atherosclerotic plaques that narrow the carotid arteries that supply blood to the brain;
- stenting and angioplasty are operations aimed at expanding the lumen of narrowed arteries. A balloon is inserted into the lumen of the narrowed artery, which inflates and increases the volume of the artery. Then special mesh tubes - stents - are placed in the artery, which prevent the lumen of the vessel from decreasing in the future.
For hemorrhagic stroke, treatment is aimed at controlling bleeding from a ruptured vessel and ensuring normal blood supply to the brain. Surgical treatment is used to remove intracranial hemorrhages and to prevent recurrent bleeding.
- Clipping of cerebral aneurysms is an operation aimed at isolating an expanded part of an arterial vessel (aneurysm) from the bloodstream. This eliminates the source of bleeding. A clip (special clamp) is applied to the base of the aneurysm, and blood stops flowing into the aneurysm.
- Embolization of aneurysms is the introduction of coils into the lumen of the aneurysm with a special catheter. The blood flow in the aneurysm is significantly reduced, and the aneurysm is thrombosed (clogged with blood clots) - this prevents its rupture.
- Removal of arteriovenous malformations - removal of a tangle of dilated and thinned vessels, which can be a source of bleeding.
Prevention
- Monitoring blood pressure levels.
- Controlling cholesterol levels.
- Controlling blood sugar levels.
- Maintaining normal weight.
- Eating plenty of vegetables and fruits.
- Regular physical activity.
- Quitting smoking, alcohol abuse.
Recommended tests
- General blood analysis
- Erythrocyte sedimentation rate (ESR)
- General urine analysis with microscopy
- Plasma glucose
- Cholesterol – low density lipoproteins (LDL)
- Coagulogram No. 3 (prothrombin (Quick, INR, fibrinogen, ATIII, APTT, D-dimer)
Stroke treatment
Treatment of stroke is regulated by relevant clinical guidelines and the Procedure for providing medical care to patients with acute cerebrovascular accident. In the first hours, thrombolytic therapy is carried out and subsequently - prevention of thrombus formation. For hemorrhagic stroke, neurosurgery may be performed. They normalize blood pressure, water-electrolyte balance, glucose levels in peripheral blood and urine, support the basic vital functions of the body and prevent complications. Drug therapy is also aimed at improving the affected functions of the nervous system [1, 3, 6].
Treatment and rehabilitation
The patient receives treatment in a hospital. All patients with suspected stroke are hospitalized on an emergency basis. The optimal period for providing medical care is the first 3 hours after a brain accident has occurred. The person is placed in the intensive care unit of a neurological hospital. After the acute period has been overcome, he is transferred to the early rehabilitation unit.
Until the diagnosis is established, basic therapy is carried out. The patient’s blood pressure is adjusted, the heart rate is normalized, and the required blood pH level is maintained. To reduce cerebral edema, diuretics and corticosteroids are prescribed. Craniotomy is possible to reduce the degree of compression. If necessary, the patient is connected to an artificial respiration apparatus.
Be sure to direct efforts to eliminate the symptoms of stroke and alleviate the patient’s condition. He is prescribed medications to lower body temperature, anticonvulsants, and antiemetics. Medicines that have a neuroprotective effect are used.
Pathogenetic therapy is based on the type of stroke. In case of ischemic brain damage, it is necessary to restore nutrition to the affected area as quickly as possible. To do this, the patient is prescribed drugs that resolve blood clots. It is possible to remove them mechanically. When thrombolysis fails, the patient is prescribed Acetylsalicylic acid and vasoactive drugs.
In case of a stroke, it is extremely important to provide timely treatment to the damaged areas of the brain. A course of use of the drug accelerates the process of recovery of brain cells after a stroke, even in cases of impaired blood circulation or hypoxia. This allows for rapid restoration of memory, thinking, speech, swallowing reflex and restoration of other functions of daily activities. Gliatilin has a positive effect on the transmission of nerve impulses, protects brain cells from repeated damage, which prevents the risk of recurrent stroke.
The drug is well tolerated by patients; it is contraindicated for use by pregnant, lactating women and people with hypersensitivity to choline alfoscerate.
Courses will need to be taken regularly. You definitely need to do physical therapy, undergo physical therapy, and visit a massage therapist. After a stroke, many patients have to restore motor skills over a long period of time and learn to care for themselves independently.
Relatives and friends should provide support to the patient and not leave him alone with the problem. Psychologists are involved in the work. Sessions with a speech therapist are often required.
Stroke rehabilitation
Stroke is a disease in which rehabilitation and care are of the utmost importance.
Recovery from a stroke begins in intensive care, from the moment vital functions are stabilized. A multidisciplinary rehabilitation team works with the patient, which includes a rehabilitation doctor, physical therapist or exercise therapy instructor, speech therapist, massage nurse, physiotherapist and physical therapy nurse, psychologist, occupational therapist, guard and rehabilitation nurse. Diagnosis is carried out using special scales that reflect the degree of dysfunction and limitations in the patient’s activity, the influence of environmental factors on the rehabilitation potential. The rehabilitation process continues throughout the entire period of hospitalization. At the second stage, patients with serious disabilities who are unable to move independently are sent to rehabilitation departments or specialized hospitals. Those who can walk independently or with support are rehabilitated in outpatient centers based in clinics and sanatoriums.
The rehabilitation process should not be interrupted, so classes must be continued at home. Of course, there are no high-tech robotic complexes or physiotherapeutic equipment at home, but exercise therapy, massage, and work with a psychologist, speech therapist and occupational therapist are possible. For this purpose, telemedicine technologies are used and visits to rehabilitation specialists are organized.
The individual rehabilitation program includes not only a referral for rehabilitation treatment, but also technical means of rehabilitation. However, usually relatives also have to devote significant physical and financial resources to achieve the best effect [7].
Rehabilitation and recovery after stroke
The recovery program after a stroke should be comprehensive and include:
- quality patient care,
- drug treatment,
- restoration of lost skills through gymnastics,
- physiotherapy,
- massage.
Rehabilitation measures also include psychotherapeutic assistance and social adaptation. The rehabilitation period takes several months or years and requires patience and perseverance.
When drug therapy is used:
- aspirin,
- beta blockers,
- diuretics,
- ACE inhibitors,
- calcium channel blockers statins,
- muscle relaxants,
- anticonvulsants,
- nootropic and neurotrophic agents,
- antidepressants.
Rehabilitation at home
Treatment after a stroke at home is carried out under the constant supervision of a neurologist. It is also aimed at preventing recurrent strokes, the risks of which are significant in the first two years after a stroke.
Treatment includes a set of rehabilitation measures related to the restoration of vital functions (movement, thinking, speech, vision, hearing), drug therapy, exercise therapy and breathing exercises.
Rehabilitation in a sanatorium
Treatment in sanatoriums is aimed at:
- consolidation of treatment results,
- normalization of blood circulation,
- prevention of recurrent stroke,
- increased performance and restoration of motor activity,
- maintaining psycho-emotional health.
The following basic methods are used:
- hardware treatment,
- manual therapy,
- exercise therapy,
- classes with a speech therapist,
- massage,
- acupuncture,
- laser treatment,
- magnetotherapy,
- hirudotherapy.
Sanatoriums for rehabilitation after a stroke are available to anyone who has had the disease, except those who:
- can't take care of himself
- suffers from severe arrhythmia,
- has mental disorders
- serious speech and motor impairments,
- epilepsy.
When choosing a sanatorium, preference is given to treatment in a specialized sanatorium with proven programs for recovery after strokes. A set of procedures requires recommendations from the treating neurologist.
Restoring a hand after a stroke
Due to impaired blood circulation in the brain, the hand after a stroke often loses sensitivity and mobility. It is necessary to begin rehabilitation of the hand in a timely manner so that the regeneration of nerve cells in the brain occurs and its mobility is restored. Most often, the hand goes numb and ceases to obey when the right hemisphere of the brain and cerebellum are damaged.
Psychological and physical rehabilitation helps restore the hand. Faith in treatment will help the patient recover faster and undergo the rehabilitation course more easily. It includes:
- drug therapy,
- exercise therapy,
- massage,
- rubbing and compresses,
- hydrotherapy,
- acupuncture,
- activities to develop fine motor skills.
The hand needs simple exercises:
- flexion-extension of fingers,
- grabbing objects
- raising your hand up,
- spreading to the sides
- modeling,
- writing and drawing.
It is important for the patient to be encouraged to eat and dress independently. Swimming is recommended if possible.
Rehabilitation exercises should be performed 2-3 times a day, physical therapy is prescribed once a day for 3-4 months. The duration of each rehabilitation session is from 10 minutes to an hour.
The task of the rehabilitation therapist is to help the patient remember how he moved his arm before the stroke and restore this action. At first, moving at least one finger can be considered a success. It is important to remember that restoring a hand after a stroke is a very long process, which does not imply giving up rehabilitation due to physical pain and despair from poor results.
It is correct to start the exercises with the large muscles of the healthy arm, mentally repeating all the movements of the affected arm. Exercises need to be changed daily, using objects or special exercise equipment. It is important to work out the entire arm, paying special attention to the fingers and shoulder muscles.
Simple exercises for every day include:
- clenching your fingers into a fist and straightening,
- flexion and extension of the arm at the elbow,
- clapping hands,
- grabbing objects
- rolling a ball on a hard surface.
After the first month of simple exercises, you can move on to training your shoulders and forearms with light dumbbells. Wrist workout includes:
- sculpting,
- letter,
- drawing,
- training with a rubber ring.
To develop the entire limb, you can train using checkers and chess, a Rubik's cube, a children's construction set, collecting buttons or matches.
At the same time, drug therapy is used to restore the arm, in which baclofen, tizanidin-teva, klonopin, and phenol are used.
After medical advice, you can use folk remedies to restore your hand. The most popular of them:
- ointment based on bay leaves and pine needles;
- compresses with alcohol tincture of pine cones and sage (200 ml of vodka per tablespoon of herb);
- sage baths,
- ointments made from propolis and fat.
About half of patients suffer from arm paralysis after a stroke, while 75% return their limbs to normal after six months of rehabilitation procedures.
Exercises for stroke survivors
Complexes and special programs are prepared by the treating neurologist, and the exercises can be performed at home or in exercise therapy rooms. Exercises include complexes of physical therapy, aerobic exercises, complexes for the restoration of motor activity and balance training.
The full rehabilitation package includes:
- massage of the limbs - every 3 hours daily;
- extension/flexion of arms and legs - 2 times a day for half an hour;
- exercises to restore speech and memory;
- breathing exercises.
Exercises can be physical and mental. The latter restore memory, speech, vision, hearing, concentration and thinking.
When performing any exercise, it is important that the patient feels good. If you experience headaches, dizziness, weakness, changes in blood pressure and other symptoms of circulatory disorders, exercise should be stopped.
Every patient who has suffered a stroke needs to undergo long-term rehabilitation, which can last for years. At the same time, it is important to remember that recovery after a stroke is not only possible, but also not uncommon, and to make every effort for successful rehabilitation.
Exercise therapy
Exercise therapy often begins after an acute period of stroke in a hospital. After discharge, as recommended, you can continue them at home. Exercise therapy relieves muscle spasms, restores motor activity and cerebral circulation.
If a stroke has completely or partially paralyzed a person, then the exercises in the first month of training only include changing the patient’s body position every three hours.
After this, they begin to perform a passive exercise therapy complex: massage and extension/flexion of the arms and legs. After the first successes in independent movements, you can perform more active exercises.
Medicine defines four stages of exercise therapy training for patients after a stroke:
- acute (classes in the first weeks after a stroke in a hospital);
- early (classes in the first six months in rehabilitation centers or at home);
- late (in six months of the second half of the first year after the stroke);
- long-term (one year after the stroke).
Exercise therapy training is carried out at a certain time, several times a day according to a planned set of exercises.
Restoring speech after a stroke
Speech and articulation suffer to one degree or another in all patients after a stroke, therefore special training complexes have been developed to restore speech function. They usually include simple exercises:
- smile, hold for 10 seconds;
- rotate with protruding tongue;
- roll your tongue into a tube;
- pronounce the alphabet, words and tongue twisters;
- click your tongue;
- bite your lips.
Each exercise is performed according to an increasing pattern, starting with 4-5 times, increasing to 30 – 40 repetitions.
Exercise equipment for rehabilitation after stroke
Therapeutic exercises after a stroke involve the use of special exercise equipment. In a hospital or sanatorium setting, the attending physician will prescribe an exercise regimen for rehabilitation. The necessary equipment is available in rehabilitation centers and sanatoriums.
The simulators are intended for:
- restoration of the musculoskeletal system,
- fine motor skills,
- for kinesiotherapy and vibration therapy,
- restoration of walking.
For patients after a stroke, there are special lifts and multifunctional exercise machines to restore many functions at the same time.
At home, to train fine motor skills, use a Rubik's cube, spiked rubber balls, modeling clay, and an expander.
Massage for recovery after stroke
Any set of training after a stroke necessarily includes massage. They start it immediately, in a hospital setting, as soon as they receive permission from the doctor. The massage begins with light stroking of the arms and legs to gently restore blood circulation. The intensity of the massage needs to be increased. After just a few days, the massage includes body turns and massage of the back and chest. Massage techniques for the rehabilitation of patients with stroke are quite simple, but it is important to learn how to perform them correctly. During the entire rehabilitation period (up to one year), massage using a special complex is one of the main forms of recovery.
In this case, just as with exercise therapy exercises, the massage complex should be determined by the doctor, and you should not deviate from it. Independent decisions here can cause harm to the patient.
Breathing exercises
Breathing exercises after a stroke are an essential part of rehabilitation. It restores oxygen access to the brain and normalizes cerebral circulation. Breathing exercises can be performed without equipment, but exercises with breathing simulators are most effective.
Today, the best-selling breathing simulator in Russia is Samozdrav. Its effectiveness lies in the fact that with each workout it ensures the supply of the required volume of oxygen to the blood and cells of the body, maintains a normal level of carbon dioxide, which naturally relieves vascular spasm.
Classes with Samozdrav not only restore blood supply to the brain, but also significantly reduce the risk of a recurrent stroke. Thus, classes at Samozdrav are both rehabilitation measures and a reliable form of secondary prevention of stroke.
The advantage of the simulator is that the load for the patient increases gradually, the first sessions do not exceed three minutes. The simulator is suitable for bedridden patients; it is suitable for use while lying down throughout the entire training session.
Its effect is as gentle as possible on the body affected by a stroke. It does not cause overload, like physical exercise, but if it is impossible to engage actively, it can become a simulator of physical activity by increasing blood circulation and bringing the muscles to the desired tone.
Thus, “Samozdrav” has a comprehensive restorative effect on the body of patients who have suffered a stroke, and can be used at home, being today the main simulator for breathing exercises.
Prevention of strokes
Hereditary predisposition to stroke, the presence of cardiac diseases, pathology of blood vessels and blood composition, age over 40 years, obesity and diabetes require a number of preventive measures:
- Maintaining normal blood pressure, taking antihypertensive drugs as prescribed by a doctor, monitoring blood pressure.
- Maintaining a normal level of physical activity, exercise, walking 30-40 minutes a day (for example, walking the dog).
- Conducting preventive examinations, including a standard set of laboratory parameters. During a preventive examination, the following tests are additionally required: gene diagnosis of CADASIL syndrome using the PCR method, plasma factors of the blood coagulation system, antibodies to prothrombin of the IgG and IgM classes to determine the risk of thrombosis, determination of polymorphisms associated with the risk of arterial hypertension, diabetes mellitus, lipid disorders exchange, in order to identify a predisposition to diseases that increase the risk of stroke, von Willebrand factor (a glycoprotein that ensures the formation of blood clots), complex laboratory tests for preclinical diagnosis of cardiovascular diseases are offered (“ELI-ANKOR-Test-12”, “Cardiorisk”).
- Avoiding chronic and acute stress, maintaining mental hygiene.
- Normalization of weight (BMI <25 kg/m2).
- Healthy eating (for example, Mediterranean diet, limiting salt to 5 5 g/day).
- Quitting smoking and taking psychoactive substances.
- Treatment of diseases that are a risk factor for stroke [8, 11].
Who is at risk
There are people who need to be especially wary of developing a stroke, as they are at risk.
Among them:
- Persons with hypertension.
- Patients with diabetes.
- Men and women over 65 years of age.
- People with abdominal obesity.
- Persons with a hereditary predisposition to vascular pathologies.
- Patients who have previously had a stroke or heart attack.
- Patients with diagnosed atherosclerosis.
- Women over 35 years of age taking oral contraceptives.
- Smokers.
- People suffering from heart rhythm disturbances.
- People with high cholesterol levels.
Most often, patients with the listed diagnoses are registered at the dispensary. Special mention should be made of people living in a state of chronic stress. Emotional stress negatively affects all systems of the body and can cause a stroke.
Bibliography
- Hemorrhagic stroke in adults: clinical recommendations of the Ministry of Health of the Russian Federation, 2021. Developers: Association of Neurosurgeons of Russia. - Electronic text. - URB: (access date 08/18/2020).
- Efremova M.D. Stroke as an urgent socio-psychological problem / M.D. Efremova – electronic text//Skif. Questions of student science.- 2021 - No. 2(24) URB: (date of access 08/17/2021) Access mode: Cyberleninka electronic library system. — Text: electronic.
- Ischemic stroke and transient ischemic attack in adults: clinical recommendations of the Ministry of Health of the Russian Federation, 2021 developers: All-Russian Society of Neurologists, National Association against Stroke, Association of Neurosurgeons of Russia, Association of Neuroanesthesiologists and Neuroreanimatologists, Union of Rehabilitologists of Russia. - Electronic text. - URB: ( access date 08/18/2020).
- Machinsky P.A. Comparative characteristics of incidence rates of ischemic and hemorrhagic stroke in Russia / P.A. Machinsky, N.A. Plotnikova, V.E. Ulyankin [and others] – Direct text.// News of higher educational institutions. Volga region. Medical Sciences.- 2021.- “2(50)-P.112 – 132 DOI 10.21685/2072-3032-2019-2-11.
- Monitoring the implementation of the federal project “Combating Cardiovascular Diseases” - Presentation Department of Organization of Medical Care and Sanatorium Affairs of the Ministry of Health of the Russian Federation URB: (date of access 08/17/2021).
- Order of the Ministry of Health of the Russian Federation dated November 15, 2012 N 928n “On approval of the Procedure for providing medical care to patients with acute cerebrovascular accidents.” — URB: (access date 08/17/2021) Access mode: Electronic library system “Garant”. — Text: electronic.
- Order of the Ministry of Health of the Russian Federation dated July 31, 2021 No. 788n “On approval of the Procedure for organizing medical rehabilitation of adults.” – URB: (date of access 08.17.2021).- Access mode: Electronic library system “Garant”. — Text: electronic.
- Prevention of cerebrovascular accidents: textbook. manual / Compiled by: L.B. Novikova, A.P. Akopyan. – Ufa: Publishing house of the State Budgetary Educational Institution of Higher Professional Education BSMU of the Ministry of Health of Russia, 2015.-58 p.
- Stakhovskaya L.V. Analysis of epidemiological indicators of recurrent strokes in the regions of the Russian Federation (based on the results of the territorial-population register 2009-2014) / L.V. Stakhovskaya, O.A. Klochikhina, M.D., Bogatyreva, etc.]. CONSILIUM MEDICUM, 2021, vol. 5, no. 9, p. 8-11.
- Shamalov N. A. Analysis of the dynamics of the main types of stroke and pathogenetic variants of ischemic stroke / N. A Shamalov, L. V Stakhovskaya, O. A Klochikhina [and others]. Direct text. // Journal of Neurology and Psychiatry named after. S.S. Korsakov. Special issues. 2019;119(3-2):5-10. doi.org/10.17116/jnevro20191190325.
- 1RRE Electronic edition. Updated daily Stroke Day is celebrated on October 29, 2021 URB: (accessed 08/17/2021).
Author:
Pugonina Tatyana Alekseevna, Therapist
Disease prevention measures
Stroke prevention consists of a set of measures to organize a healthy lifestyle:
- control your blood pressure in the morning and evening (optimal systolic (upper) pressure should be in the range of 110-139 mm Hg. If your readings regularly increase, consult your doctor to prescribe medication;
- monitor cholesterol levels, as its high content provokes hardening of blood vessels;
- switch to a healthy diet - reduce salt intake, increase the amount of vegetables and fruits. Make changes to your diet gradually. Avoid snacking on the go and overeating, especially sweets and sausages;
- go in for sports - moderate physical activity (cycling, jogging, gymnastics, walks in the fresh air, swimming, tennis);
- limit your consumption of alcoholic beverages. Without serious consequences for the body, it is permissible to consume 20 grams of pure alcohol per day (this is a bottle of beer, 2 glasses of wine or 50 grams of high-quality vodka);
- undergo annual medical examinations upon reaching 40 years of age (ultrasound of the heart and blood vessels, ECG, biochemical blood test, MRI of the brain).
- eliminate increased psycho-emotional stress and stress. If you cannot completely limit yourself from them, protect the nervous system with plant-based sedatives (Fitosedan, Persen, Tenoten, Afobazol, Herbion, etc.);
- stop smoking.
Chronic stress, snacking on the go, and unfavorable environmental conditions lead to decreased vascular function, which reduces blood supply to the brain. If one of the provoking factors is present, the specialist draws up an individual program for the prevention of hemorrhagic stroke.
Stroke is a fatal disease that affects men over 40 years of age. Smoking and constant stress increase the risk of its development, so you should get rid of all bad habits, be less nervous and be examined at least once a year in a medical facility. Remember that any disease, including stroke, is easier to prevent and prevent than to treat serious complications.