This is a special category of bacterial cultures, many species of which are dangerous to human health. Staphylococci are commonly called opportunistic microbes. Living in the body constantly, they are under the control of the immune system. But when the protection is weakened, they can provoke an inflammatory process. Some bacteria are extremely resistant to antimicrobial agents and often cause superinfections.
What is staphylococcus
Staphylococci are non-motile bacteria with a diameter of 0.6-1.2 microns, during the growth process they form colonies that look like bunches of grapes. Bacteria can also occur in pairs, groups, or short chains.
Staphylococci are the most well-known and widespread bacteria. They represent part of the microflora of mammals. To date, more than 26 varieties are known. Some of them are pathogenic for humans, especially Staphylococcus aureus or Staphylococcus aureus. If immunity is reduced or the general condition of the body is unsatisfactory, it can pose a significant threat to health, causing infections, including post-operative and wound infections. They often take a long and difficult time to treat.
Diagnostic search
For a proper diagnosis, you need to see a doctor. But it is worth conducting research only if there are symptoms. The fact that biological material contains staphylococcus is an absolute norm. Initially, you need to collect the material. Be sure to conduct dynamic tests. If the number of bacteria constantly increases, this is a staphylococcal infection. It is necessary to understand what type of infection caused it in order to choose the right treatment tactics for Staphylococcus aureus .
diagnosis of staphylococcus
What is staphylococcus
Staphylococci are non-motile bacteria with a diameter of 0.6-1.2 microns, during the growth process they form colonies that look like bunches of grapes. Bacteria can also occur in pairs, groups, or short chains.
Reference!
When using the Gram stain of microorganisms, they show a rich blue color that does not disappear over time. Some can synthesize pigments.
For the most part, staphylococci are non-spore-forming and non-encapsulated bacteria. They are found in the external environment and do not do well in aqueous solutions of silver salts.
Staphylococci are:
- Conditionally pathogenic - do not cause diseases in a healthy person with strong immunity)
- Pathogenic - live on the skin, mucous membranes of the nasopharynx and oropharynx. They produce various toxins and enzymes that negatively affect the functioning of the cell.
Features of Staphylococcus aureus
The most famous among pathogenic ones is Staphylococcus aureus - the culprit of purulent lesions of organs and tissues. It can live in the nasal passages, armpits and inguinal folds, as well as on the skin of the perineum. Produces the enzyme coagulase, which not only protects it from the hostile reaction of the human body, but also ensures adhesion (adhesion) of the pathogen to the surface structures of cells.
Some strains of Staphylococcus aureus can cause toxic shock due to the exotoxin they produce. And other enterotoxins lead to diarrhea.
But much more terrible is the ability of this microorganism to provoke purulent-septic infections of tissues and organs, and postoperative complications. An important role in this process is played by the conglomerates (biofilms) formed by the bacterium, which grow under the influence of glucose, NaCl, and sodium citrate.
Staphylococcus aureus thrives even in a hospital environment, demonstrating resistance to many antibacterial drugs.
The ideal temperature for Staphylococcus aureus is 30-37 degrees, but the bacterium can tolerate higher temperatures (dying only at 80 degrees and above), as well as freezing and drying.
Staphylococcus can be transmitted by airborne droplets, fecal-oral, and also through household contact.
Why is staphylococcal infection dangerous?
Staphylococcus is especially dangerous in association with viruses and fungi, as well as with concomitant childhood droplet infections that reduce the overall reactivity of the body. It is not without reason that in many diseases local or general complications caused by staphylococci are observed.
Thus, during influenza epidemics, staphylococcal pneumonia is not uncommon, which most often turns out to be the cause of a child’s long-term illness and is the most common prerequisite for death.
Staphylococcal and streptococcal toxins have pronounced sensitizing properties, causing allergies and toxic damage to the heart muscle, kidneys and other important organs. Unlike a number of pathogens of childhood infections, the site of action of which is limited to certain areas of body tissue, staphylococcus and streptococcus are “omnivorous”.
They can cause inflammation of the gallbladder (cholecystitis), toxic dyspepsia and gastroenteritis, inflammation of the joints (arthritis), and genitourinary tract (urethritis and endometritis). In newborns, staphylococcal and other purulent inflammatory phenomena begin with the umbilical wound or other skin lesions that are invisible at first glance (scratches, abrasions).
It must be emphasized that up to 90% of cases of sepsis in young children are associated with staphylococcus.
Classification of Staphylococcus aureus
In scientific circles, Staphylococcus aureus is classified according to its sensitivity to drugs.
There are:
- wild strain,
- methicillin sensitive (MSSA),
- methicillin-resistant (MRSA),
- vancomycin-resistant (VRSA and VISA) is an extremely rare strain that is most often found in patients undergoing bone marrow transplantation.
The resistance of Staphylococcus aureus to drugs and the rate of its formation are very high. At the very beginning of the study of the microorganism, it was sensitive to benzylpenicillin, but over time it adapted to it. Then methicillin was introduced into clinical practice. But soon bacteria appeared that were resistant to it. In this case, vancomycin and teicoplanin, as well as some other antibacterial drugs, are used.
Literature
- Zipperer A., Konnerth MC, Laux C., Berscheid A., Janek D., Weidenmaier C. et al. (2016). Human commensals producing a novel antibiotic impair pathogen colonization. Nature. 535, 511–516;
- Dobson A., Cotter P. D., Ross R. P., Hill C. (2012). Bacteriocin production: a probiotic trait? Appl. Environ. Microbiol. 78, 1–6;
- Donia MS, Cimermancic P, Schulze CJ, Wieland Brown LC, Martin J, Mitreva M et al. (2014). A systematic analysis of biosynthetic gene clusters in the human microbiome reveals a common family of antibiotics. Cell. 158, 1402–1414;
- Antimicrobial peptides are a possible alternative to traditional antibiotics;
- Lewis K. and Strandwitz P. (2016). Antibiotics right under our nose. Nature. 535, 501–502;
- Wikipedia: “Staphylococcus aureus”;
- Karpov I.A. and Kachanko E.F. (2005). Staphylococcal infection: clinical aspects and prospects for therapy. Medical news. 9, 53–56;
- Mandal A. (2012). What is Staphylococcus aureus? News-Medical.net;
- Naber C. K. (2009). Staphylococcus aureus bacteremia: epidemiology, pathophysiology, and management strategies. Clin. Infect. Dis. 48 , S231–S237;
- Staphylococcus aureus (Staphylococcus aureus). GastroScan;
- Mobile genetic elements of prokaryotes: stratification of the “society” of vagabonds and homebodies;
- Wikipedia: “Non-ribosomal peptides”;
- Caboche S., Pupin M., Leclère V., Fontaine A., Jacques P., Kucherov G. (2008). NORINE: a database of nonribosomal peptides. Nucleic Acids Res. 36 , D326–D331;
- Mironovskiĭ ML, Ostash BE, Fedorenko VA (2010). Diversity of genes encoding nonribosomal peptide synthetases in the Streptomyces sioyaensis genome. Genetika. 46, 896–903.
Diseases caused by bacteria
A person can get sick:
- due to the penetration of bacteria into the body,
- increased production of exotoxin.
At particular risk are:
- newborn babies,
- nursing mothers,
- patients with influenza or chronic pulmonary diseases,
- patients with chronic systemic diseases (renal failure, diabetes, AIDS, cancer),
- people with transplants, implanted prostheses, catheters,
- patients who are taking immunosuppressants, glucocorticoids or receiving chemotherapy,
- wounded,
- injection drug addicts.
Direct penetration into the body is fraught with:
- skin infections
- endocarditis,
- osteomyelitis,
- septic arthritis,
- pneumonia,
- death (a common cause among patients is staphylococcal bacteremia, that is, bacteria entering the blood)
Skin infection
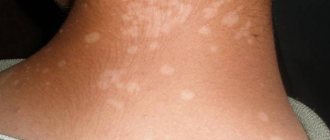
Skin infection is the most common form of Staphylococcus aureus infection. Accompanied by the formation of single blisters with pus or their accumulation, abscesses, boils, crusts. It occurs in conditions of high temperature and humidity, when the integrity of the skin is damaged due to certain diseases (eczema, etc.), surgical interventions, injections or intravenous catheterization, as well as on intact skin.
Staphylococcal endocarditis
Staphylococcal endocarditis or inflammation of the endocardium is a frequent companion of people with prosthetic heart valves and injection drug addicts. It is accompanied by vascular blockage - embolism, pericarditis, the formation of visceral abscesses, conduction disturbances and heart failure.
Staphylococcal osteomyelitis
Osteomyelitis is an inflammatory destructive disease of the bone that causes bone pain, chills, swelling and redness of the soft tissues surrounding the bone.
Staphylococcal infectious arthritis
S. aureus infection of a joint or endoprosthesis. It may be primary or result from infection during surgery. A person experiences pain in the affected area when moving, flexing and extending limbs, and suffers from fever and weakness.
Staphylococcal pneumonia
S. aureus is a common cause of nosocomial pneumonia, including ventilatory pneumonia during mechanical ventilation, anesthesia pneumonia, and lung abscesses.
In addition to the above, Staphylococcus aureus can lead to:
- rhinitis,
- sinusitis,
- meningitis,
- pharyngitis,
- laryngitis,
- lesions of the genitourinary and visual systems.
Staphylococcal rhinitis
Rhinitis, or inflammation of the nasal mucosa caused by this bacterium, is accompanied by the release of yellow-green mucus, difficulty in nasal breathing, soreness of the nasopharynx, and fever.
If the disease is not treated, the inflammatory process can spread to the paranasal sinuses and cause sinusitis.
Staphylococcal sinusitis
Depending on the affected area, the following types of sinusitis are distinguished:
- sinusitis - inflammation of the maxillary sinus,
- frontal sinusitis - inflammation of the frontal sinus,
- ethmoiditis - inflammation of the mucous membrane of the ethmoid labyrinth,
- sphenoiditis - inflammation of the sphenoid sinus.
Sinusitis is characterized by nasal congestion and purulent discharge, headache, pain in the upper jaw, temperature, and a feeling of pressure. If left untreated, the following complications may occur:
- thrombosis of the paranasal sinuses,
- meningitis,
- infection of the skull bones,
- eye infection.
Staphylococcal meningitis
When the membranes of the brain are damaged by Staphylococcus aureus, meningitis occurs. Symptoms: severe headaches, stiff neck muscles, photophobia, nausea, mental problems.
Staphylococcal pharyngitis
When the bacteria infects the mucous membrane of the pharynx, pharyngitis occurs. The mucous membrane becomes inflamed, red, and the throat swells. The patient complains of a sore throat, enlarged tonsils and the formation of purulent plugs, hoarseness, cough provoked by a sore throat, and chills.
Staphylococcal laryngitis
This is an inflammation of the larynx. The most striking symptom is a change in voice up to its complete loss (aphonia). The situation is aggravated by a sore throat, difficulty swallowing, and fever.
Exotoxin provokes the following systemic lesions:
- necrosis,
- scalded skin syndrome,
- toxic shock.
Staphylococcal scalded skin syndrome (toxic epidermal necrolysis)
The clinical picture of staphylococcal scalded skin syndrome, which occurs in infants and children under 5 years of age, is characterized by large blisters and peeling of the top layer. Ultimately, large layers peel off (exfoliation).
Staphylococcal food poisoning
2–8 hours after consuming meat, fish, eggs, pastries with cream, dairy products contaminated with bacteria and insufficiently thermally processed (or left after processing at room temperature for a long time), severe vomiting, cramps, and fever may occur. In this case, they talk about staphylococcal food poisoning, which can last up to 12 hours.
Diagnosis of the presence of bacteria
After examining the patient and collecting anamnesis, the doctor prescribes laboratory tests of purulent discharge, smears or biological fluids (urine, blood).
Diagnostic methods:
- microscopic - samples obtained from the patient are applied in a thin layer to a glass slide, dried, Gram stained and examined under a microscope;
- cultural - the sample is placed on a nutrient medium in a Petri dish, and after 18-48 hours the results are analyzed;
- enzyme immunoassay (ELISA) method;
- serological diagnostics;
- enzyme tests;
- PCR diagnostics.