Erythrasma is a bacterial skin lesion that manifests itself in areas with large folds: armpits, abdomen, groin area, under the breasts in women, on the inner thigh. Characteristic symptoms of erythrasma are the appearance of gradually growing spots of a reddish, brown and yellowish hue. They are distinguished from other skin diseases by dryness and a tendency to peeling. They are absolutely painless, but require attention because they do not go away on their own. Erythrasma owes its name to Greek terminology - translated into Russian, erythrasma means “colored red.” It is with this that the affected areas glow under the influence of a Wood's fluorescent lamp, with the help of which diagnostics are carried out.
What is erythrasma
Erythrasma is so called due to the fact that when using fluorescent diagnostics, the lesions glow with a reddish tint. This disease occurs most often in adults, mainly among male patients, and lasts a very long time. In this case, the patient does not experience any negative or painful sensations.
For a long period of time, erythrasma, together with actinomycosis, trichophytosis, pityriasis versicolor, microsporia, favus and epidermophytosis, was considered a skin disease of fungal etiology for the reason that when conducting a microscopic analysis of the scales that were removed from the affected skin lesions, it was possible to detect tortuous thin threads that Outwardly they resemble fungal mycelia. In the current classification, dermatologists believe that erythrasma belongs to the group of pseudomycoses. These diseases, in their clinical picture, are very similar to fungal skin lesions, but they have a completely different etiology.
Mechanism
Corynebacterium minutissimum
The bacteria causing this infection are often club-shaped rods that are observed under a microscope after a staining procedure that is the result of a crevice separation that makes them look like a picket fence.
This bacterium is gram positive, which means it has a very thick cell wall that is not easy to penetrate. Electron microscopy confirms the bacterial nature of erythrasma and shows a decrease in electron density in keratinized cells in areas of proliferation.[6] This means that bacteria cause erythrasma by breaking down the keratin fibrils in the skin. Corynebacterium minutissimum
consumes carbohydrates such as glucose, dextrose, sucrose, maltose, and mannitol.[2]
Erythrasma appears primarily in slightly webbed spaces between the toes (or in skin folds of other areas of the body such as the thighs/groin) in warm regions and is more common in dark-skinned people. As a person ages, he or she becomes more susceptible to this infection. This bacterium is found not only in regions with a warm atmosphere, but also in warm and sweaty parts of the human body. Corynebacterium minutissimum
Survives best here by stimulating fungal growth in these regions and allowing them to multiply. It is more common among African Americans due to the pigmentation of their skin.
Causes of erythrasma
The only causative agent of erythrasma is the cornobacterium Corynebacterium minutissimum. The bacterium is slightly pathogenic and has very low contagiousness (the ability of a disease to be transmitted from sick people or animals to healthy people or animals). Normally, the pathogen is often located on the skin of absolutely healthy people in the role of a saprophytic microorganism. The infection is transmitted by contact, mainly through objects of personal use, as well as during sexual intercourse, walking barefoot on the beach or bare ground, visiting a bathhouse or swimming pool.
The erythrasma bacterium affects the surface layer of the skin (epidermis), while hair and nails remain uninvolved in the infection process (intact). Also, the penetration of bacteria into the layers of the epidermis is facilitated by such processes as changes in skin pH (towards the alkaline side), hyperhidrosis, hot climates with high humidity, friction and maceration of the skin, diaper rash, insufficient skin hygiene, and individual characteristics of the body.
How the disease develops
Corynebacterium minutissimum penetrates the surface layers of the skin from the outside - upon contact with the patient or his household items, as well as from the soil (penetrates into the interdigital spaces). When infected, the stratum corneum of the skin is affected by 1/3 of its thickness. Nail plates and hair are not affected. Bacteria develop in moist and warm places - folds of the body and, first of all, places of increased sweating and diaper rash or in the presence of cracks in the interdigital folds on the feet.
Rice. 4. Inguinal erythrasma in a woman. View of the affected areas in the rays of a Wood's lamp.
Symptoms of erythrasma
The appearance of round spots of light brown, yellow-brown, brownish-red color on the surface of the skin indicates the onset of the disease. The size of the spots can range from a few millimeters to several centimeters in diameter. Erythrasma spots generally have round edges, but there are also scalloped (wavy) edges.
As the lesions increase in size, erythrasma lesions begin to merge, forming one single lesion that is clearly demarcated from healthy skin. This area has a smooth, even surface and is covered with small pityriasis-like scales on top. After some time, in the central part of the area affected by erythrasma, you can notice a brown color or even a pale color.
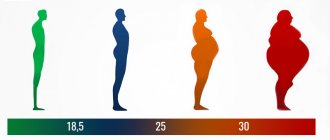
Erythrasma is characteristically localized around and inside large folds of skin. In males, lesions are most often observed in the groin area, skin around the anus, and inner thighs. In females, erythrasma most often occurs in the area of the folds under the mammary glands, as well as on the skin in the umbilical and axillary zone. In people who are overweight, erythrasma may affect the fat folds on the abdomen.
Most often, erythrasma is not associated with any subjective unpleasant sensations. Occasionally, the patient may notice mild itching or burning. For this reason, erythrasma can occur almost unnoticeably and asymptomatically for a long time. Erythrasma lasts for quite a long time (about 10 years) and can be accompanied by frequent alternation of periods, during which remissions and exacerbations occur. Exacerbations of erythrasma most often occur during the spring-summer period, when warm temperatures are conducive to the active proliferation of bacteria. Patients with obesity, diabetes mellitus and hyperhidrosis may suffer from a complicated form of erythrasma. In this case, the symptoms of erythrasma are accompanied by symptoms of eczema, as well as secondary infection of the affected area with the disease or the appearance of diaper rash. The development of complications, in one form or another, is facilitated by frequent friction, wet and contaminated affected skin. Complicated erythrasma is characterized by a feeling of burning and itching, as well as the appearance of pain in the affected area.
How is erythrasma diagnosed?
Making a diagnosis is not difficult. Usually, an in-person examination of the patient and examination of the rash with a Wood's lamp is sufficient. If, under the light of a lamp, the affected areas of the skin turn red, then there is usually no doubt. This feature usually occurs due to the release of water-soluble porphyrins by pathogens.
However, before resorting to Wood's lamp diagnosis, it is worth making sure that the patient has not treated the rash with anything. Otherwise, the coloring pigment may wash off and an incorrect diagnosis will be made.
The inguinal form of the disease has characteristic features. The lesions are distinguished by protrusions at the edges, maceration and blisters. However, erythrasma is very easily confused with rubromycosis of the groin area. These two pathologies have similar symptoms. When diagnosing, special attention should be paid to the edges of the inflamed areas. With rubromycosis they will be intermittent, and erythrasma will have a continuous, pronounced edge.
Diagnosis of erythrasma
The disease is effectively diagnosed by its typical clinical picture and typical localization of lesions, as well as brick-red or coral-red glow during a fluorescent examination using a Wood's lamp. Luminescence testing should be performed on an area of erythrasma that has not been subjected to any treatment, since washing or treatment washes away the pigment secreted by the bacteria. When conducting a microscopic examination of a scraping that was taken from an area of skin affected by the disease, it is possible to identify winding threads similar to the mycelium of the fungus, as well as coccoid cells in the form of separate groups or chains.
Erythrasma has some signs of the clinical picture of diseases such as athlete's foot, lichen versicolor, cutaneous candidiasis, rubromycosis, pityriasis rosea, microbial eczema, perianal dermatitis. In special cases, in order to distinguish erythrasma from similar diseases, bacterial culture of scrapings is carried out to clearly identify the pathogen. In parallel, the sensitivity of the pathogen to antibacterial drugs is also determined. This is primarily necessary for the correct prescription of medications for general antibiotic therapy.
Complications
The main danger of the disease is the risk of complications recorded in patients with hyperhidrosis, diabetes mellitus, obesity and other diseases - the appearance of diaper rash, eczema, vascular disorders, the development of bacterial (streptococcal and staphylococcal) and fungal infections.
Erythrasma in the groin area leads to irritation of the genital organs and the development of secondary infection. The disease is dangerous due to the development of lung abscess, endocarditis, and septicopyemia. The role of Corynebacterium minutissimum in the pathogenesis of male infertility is discussed.
Rice. 9. The photo shows erythematous swelling of the foot in a patient with diabetes mellitus. Multiple blisters and bubbles are visible.
Treatment of erythrasma
Local therapy for erythrasma is limited to rubbing erythromycin or sulfur-tar ointment into the affected area. This procedure is usually performed twice a day for a week. After this manipulation, the erythrasma spots slowly and gradually change their color to a paler color and disappear over time. In case of secondary infection, as well as when inflammatory changes appear in the lesions of erythrasma, they are treated with aniline dyes or resorcinol alcohol. Also, a large number or area of lesions is an indication for starting systemic antibiotic therapy.
Elimination of foci of erythrasma and prevention of further exacerbations of the disease is facilitated by the disinfecting and drying effects of soft ultraviolet rays. For this reason, it is very useful for patients to stay in sunlight as long as possible in the evening and morning, and attend ultraviolet irradiation sessions.
To prevent self-infection and successfully treat erythrasma, it is necessary, if possible, to completely disinfect the patient’s clothing, bedding and personal belongings. Clothes and linen must be washed every day and be sure to iron them afterwards.
What is pityriasis versicolor
Pityriasis versicolor, or pityriasis versicolor, is a chronic skin disease of a fungal nature. It appears in the form of specifically pigmented spots of various sizes and shades, without signs of inflammation. Most often, the areas affected by pityriasis versicolor are located on the body (back, abdomen, neck, shoulders) and scalp. Representatives of both sexes are most susceptible to the disease at a young age, and children under 7 years of age are the least susceptible.
External manifestations of the disease usually do not cause concern, so they are often perceived as harmless cosmetic defects. For this reason, the pathology becomes chronic: spots periodically appear, then disappear, and after some time, under the influence of provoking factors, the disease worsens again.
Prevention of erythrasma
First of all, the prevention of erythrasma consists of following the rules of skin hygiene, thoroughly wiping large folds of the skin after taking water treatments, and avoiding tight clothing and synthetic clothing. Secondary prevention involves preventing the development of relapses of the disease. Prevention is carried out within a month after the last symptom of the disease has disappeared. It consists of washing the skin folds with camphor or salicylic alcohol and applying a layer of talc.
Care
Initial treatment for minor erythrasma may begin with keeping the skin area clean and dry with antibacterial soap.
The next level is treated with topical fusidic acid and an antibacterial solution such as clindamycin to kill bacteria. For aggressive types of erythrasma, oral antibiotics such as macrolides (erythromycin or azithromycin) may be prescribed.[1] Below is a graphic showing the different types and subtypes of therapy. Therapy
| Oral | Current |
| Erythromycin | Clindamycin |
| Clarithromycin | Whittfield ointment |
| Tetracycline | Sodium fusidate ointment |
| Chloramphenicol | Antibacterial soap |
There is no consensus on the best treatment for this disease. These treatments have many limitations, such as increased irritation, possible allergic reactions, and ulceration.[3] These treatments are suitable for most ages, but young children should be monitored very closely.
Recommendations
- ^ a b
"Erythrasma - American Osteopathic College of Dermatology (AOCD)".
www.aocd.org
. Retrieved 2017-11-06. - ^ a b
"Erythrasma".
misc.medscape.com
. Retrieved 2017-11-06. - ^ a b c
Holding, M. R. (2002).
"Treatment of cutaneous erythrasma." Drugs
.
62
(8):1131–41. Doi:10.2165/00003495-200262080-00002. PMID 12010076. - Tony Burns; Stephen Breathnach; Neil Cox; Christopher Griffiths (2010). Rock's Textbook of Dermatology
. John Wiley and Sons. P. 5–. ISBN 978-1-4051-6169-5. Retrieved November 14, 2010. - Likness, L.P. (June 2011). "Common Dermatologic Infections in Athletes and Recommendations for Return to Play." Journal of the American Osteopathic Association
.
111
(6):373–379. doi:10.7556/jaoa.2011.111.6.373. PMID 21771922. - Weedon, David (2010). "Bacterial and rickettsial infections." Weedon's Skin Pathology
. pp. 547–572. e22. Doi:10.1016/B978-0-7020-3485-5.00024-3. ISBN 978-0-7020-3485-5.