A bone fracture is a partial or complete disruption of the structure of bone tissue. The main cause of fractures is the physical load created on the human skeleton, which exceeds the strength of the bones. But fractures also occur due to various diseases, due to which bone tissue becomes thinner and loses strength, and crunching appears in the joints.
Let's take a closer look at the concept of a fracture and how it differs from a dislocation based on symptoms; we'll also talk about the main causes of injuries and the rules of first aid.
Bone fracture - definition and significance of the problem
Fracture is a common natural injury. The mechanism of occurrence of this type of injury in humans is the same as in all vertebrates. About 80% of all broken bones are tubular: femur, radius, pelvis. Not only bones are damaged, but also nearby soft tissues - muscles and blood vessels. Less commonly, compression or complete rupture of nerve endings occurs, followed by bleeding.
Fractures in real life are combined with damage to various organs and systems of the body. In medicine, such diseases are called combined injuries. For example, when rib fractures develop, pleurisy develops, and when the skull bones are damaged, intracerebral hematomas develop.
Comminuted fracture
Comminuted clavicle fractures usually occur in adults. In most cases, the integrity of the bone is disrupted in the middle third, and the fragments are displaced due to muscle traction. The patient complains of pain, movements are limited, deformation and swelling are detected in the area of damage. When the fragments are displaced, shortening of the shoulder girdle is possible. When nerves are damaged, sensory disturbances are detected. If large vessels are damaged, massive bleeding is possible. Palpation for such injuries should be as gentle and careful as possible, since pressure on the bone can cause displacement of small fragments and rupture or compression of previously intact vessels and nerves.
To confirm the diagnosis, an x-ray of the collarbone is prescribed. Therapeutic tactics depend on the position of the bone fragments. In the absence of complications, closed reposition is performed with the application of Delbe rings (with minor displacement), Smirnov-Vanshtein bandage, figure-of-eight bandage or Sayre bandage. If the brachial plexus is damaged, as well as the presence of a fragment directed with its sharp end towards the vessels and nerves, surgical treatment is indicated - osteosynthesis of the clavicle with a knitting needle, plate, pin or Bogdanov nail.
Comminuted fractures of the humerus can occur in any part of the segment. The cause is usually a fall on the hand, less often - a blow or twisting of the hand. If the upper third is damaged (fractures of the head, fractures of the neck of the shoulder), swelling and deformation of the shoulder joint are observed. Movements in the joint are sharply limited, crepitus may not be detected. Proximal fractures, as a rule, have a relatively favorable course. Usually, a good result can be achieved using conservative methods - reposition and subsequent fixation. If it is impossible to compare the fragments, osteosynthesis of the humeral head with screws or osteosynthesis of the surgical neck of the shoulder with a plate or knitting needles is performed.
With comminuted fractures of the humeral diaphysis, deformation, swelling, crepitus and pathological mobility are detected. There may be compression or disruption of the radial nerve or, less commonly, artery. With injuries to the lower parts (fractures of the intercondylar eminence, capitate eminence and trochlea), the elbow joint is swollen, deformed, and movement is impossible. With fractures of the diaphysis and lower third of the humerus, difficulties often arise in the process of comparing fragments.
Treatment tactics are selected taking into account complications and radiographic data of the humerus. If the artery is damaged, emergency surgery is indicated. In other cases, reduction is usually performed or skeletal traction is applied. If the fragments cannot be compared, osteosynthesis of the humeral diaphysis is performed with a plate or knitting needles. Surgical intervention to restore the nerve is usually performed in the long term. In the absence of tension, a suture of the nerve is indicated; in other cases, plastic surgery of the damaged nerve trunk is indicated.
Comminuted fractures of the bones of the forearm can be intra- and extra-articular, located in the lower, middle and upper third of the segment. Intra-articular fractures include a comminuted fracture of the olecranon, a fracture of the head of the radius, and a Malgenya injury (fracture of the olecranon combined with dislocation of the bones of the forearm). With all of these types of injuries, swelling and deformation of the joint are observed. Movements are severely limited or impossible. Treatment tactics are determined taking into account X-ray data of the elbow joint. Surgical intervention is often required: osteosynthesis of the olecranon process with a plate, wires or screws, resection of the head of the radial bone.
Comminuted diaphyseal fractures of the forearm bones are a fairly common injury. Accompanied by visible deformation, pathological mobility, crepitus, edema, and disruption of the limb axis. Retention of fragments after reduction in such injuries often becomes a challenge even in the case of simple transverse or oblique fractures, since the fragments are repeatedly displaced due to muscle traction. In the presence of fragments, the task becomes even more complicated, so it is often necessary to resort to surgical treatment. The tactics of surgical intervention are determined taking into account X-ray data of the forearm. Osteosynthesis with a plate or pin is possible; in some cases, osteosynthesis of the forearm bones is performed using an Ilizarov apparatus.
Comminuted fractures of the radius in a typical location are also not uncommon. Usually there is displacement of the fragments. The wrist joint is deformed, swollen, and movements are severely difficult. Crepitation is unusual. An x-ray of the wrist joint reveals a fracture with the presence of a varying number of fragments. In most cases, the displacement can be eliminated during closed reposition; in some cases, osteosynthesis of the distal metaepiphysis of the radius with screws, wires or a plate is necessary.
What types of fractures are there: generally accepted medical classifications
Fractures are classified according to several criteria: the location of the fragments, the location of the injury and the shape of the fractured area.
Depending on the location of the fragments, bone fractures can be open or closed. In the first case, the injury is accompanied by damage to soft tissue, to the point that the bone is visible. With a closed fracture, this does not happen: the soft tissue remains intact, there is no hemorrhage.
Open fractures are divided into primary and secondary. In the first case, soft tissues are injured due to an external provoking factor, and in the second, due to the fact that a bone fragment injures the tissues, forming a through wound in them.
There are separate types of closed fractures:
- Combined . Characterized by multiple injuries to internal organs.
- Combined . Appear due to external influences, such as trauma or radiation.
- Multiple . Several bones are damaged at once.
- Single . Only one bone is injured.
- Full . The ends of the bone are separated from each other.
- Incomplete - the bone does not separate, but cracks and marginal fragments form on its surface.
The most severe type of injury is a displaced bone fracture. Due to a displaced fracture, complications arise: such as paralysis of the limbs or loss of sensitivity, loss of ability to work, and sometimes death.
Based on location, the fracture is classified into the following types:
- Epiphysiolytic - with damage to the growth zone of bone tissue in children.
- Epiphysial - with injury to the joint cavity.
- Diaphyseal - damage to tubular bones.
- Involved - associated with damage to cancellous bone elements.
The epiphyseal type of fractures is considered the most difficult to cure. It is often combined with dislocations, which makes it difficult to immediately determine the type of injury and prescribe precise treatment.
Another classification of types of fractures is given by the form of bone damage:
- Transverse - the fracture line is perpendicular to the bone itself.
- Longitudinal - the fracture line is located parallel to the damaged skin tissue.
- Oblique - the fracture line is located at an angle to the tubular bone itself
- Helical - a type of fracture in which bone fragments are displaced relative to their original position.
- Comminuted - during an injury, not a single fracture line is formed, but individual fragments appear on a section of the bone.
- Wedge-shaped - this type of fracture is characteristic of spinal injuries, when one bone is pressed into another and forms cracks and wedge-shaped defects on its surface.
- Compression fracture is a type of fracture in which many small fragments form on the damaged area of bone tissue.
Causes
Depending on the cause of occurrence, traumatic and pathological fractures are distinguished. The cause of traumatic bone fractures is a sharp, sudden action of a mechanical shock force on the bone. Pathological fractures appear when a certain pathological process affects bone tissue. This may be the result of a cyst or the development of a malignant tumor. In this case, the structure of the bone tissue is gradually destroyed and even small loads can lead to a fracture. With the second type, the risk of fracture increases several times. It even gets to the point where a person can also break a leg while walking. Here the reason is that this is a pathology of the bone itself, and not an external influence on it.
Diagnosis of fractures
Diagnosis of injury is carried out by a surgeon or traumatologist. You can independently distinguish fractures from other injuries (dislocation, bruise), but only a doctor can determine the degree of its severity.
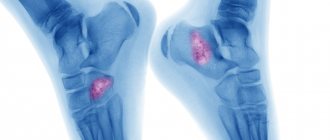
The main diagnostic method is radiography in two projections. See what the fracture looks like in the picture:
If there are signs of an open fracture of a limb, the doctor will additionally prescribe an MRI or ultrasound to the patient to determine how much the fragments damaged the soft tissues and whether the nerve endings are affected.
Diagnostics
For most closed fractures, X-ray diagnosis plays a leading role. This study is necessary not only to confirm the diagnosis of the fracture and document it. It is very important for the traumatologist, based on radiographs, to get an idea of the nature of the displacement of the fragments, the direction of the fracture lines and the presence of additional cracks indicating splitting of the fragment. This information is needed to determine treatment tactics and select the type of osteosynthesis. X-ray examination is also important during the treatment process. It determines the completeness of reposition, the correct position of the fixing structure, the absence of secondary displacement (as swelling subsides), the appearance and formation of callus. The surgeon and traumatologist must follow the rules for taking radiographs for fractures.
Providing first aid for fractures - 3 very important steps
In case of fractures, it is very important to provide correct and timely first aid. Consistent, competent actions will prevent the consequences of injury and pain shock in the victim.
Rules and procedures for providing first aid:
- Call an ambulance . Setting a joint yourself is something you should not do if you have a fracture. Before the ambulance leaves, the victim is given consistent first aid .
- Give the victim painkillers - Ketanov or Nise. It is better if painkillers are administered intramuscularly, so they will act faster. If you don’t have an ampoule of medicine on hand, use the drugs in tablet form. Pain relief is something that must be done for fractures. Otherwise, a person will feel intense pain in the joint when trying to fix the affected limb, and even painful shock is possible.
- Secure the joint with a splint . A splint is placed at the fracture site to prevent bone fragments from damaging soft tissue. When providing first aid, you can use available means: a wooden board, ski poles. If there are no objects suitable for splinting, then the victim’s body is used as a splint. For example, a broken leg is fixed to a healthy one using a bandage or clothing. The upper broken limb is fixed with a splint to the neck or torso.
Subsequent first aid procedures will depend on the type of fracture. If it is open, then help will include disinfecting the wound and stopping the bleeding before applying a splint. Bacteria can quickly enter through a wound and cause gangrene of the limbs. Before fixing the joint in one position. It is necessary to place an antiseptic wipe moistened with hydrogen peroxide on the injured area.
With an open fracture, blood often oozes from the wound, so you need to know how to properly stop it. Assistants must correctly determine the type of bleeding that has opened:
- Venous. The blood flows slowly and has a dark red tint (brown). In this case, the tourniquet is applied below the fracture site.
- Arterial. The blood flows out in a pulsating stream and has a scarlet color - the tourniquet is fixed above the wound as quickly as possible so that as little blood spills out as possible.
Instead of a tourniquet, you can use bandages, bandages or scraps of clothing; If necessary, cut off the clothing with a knife. You should definitely put a piece of paper with a note under the bandage. In it, first aid providers must indicate the time of application of the compressive bandage. If the ambulance is delayed, the tourniquet is loosened every 30 minutes!
If a person breaks the thoracic or lumbar spine, then they do not put a splint on him. In this case, first aid only includes calling emergency services, pain relief and stopping the bleeding. If you need to move a victim from the scene of an accident, for example from a roadway, then only a rigid stretcher is used for this. The person is secured on a stretcher to prevent him from flying off. For a fracture of the cervical spine, an immobilizing collar is used.
Symptoms
Bone fractures have characteristic symptoms that make it possible to identify pathology when it occurs, which is very important to exclude complications. The following main relative signs of a fracture can be distinguished: - Pain syndrome: sharp pain when a bone ruptures and aching pain in the future, which intensifies with longitudinal load or its imitation. - Swelling: Swelling in the affected area develops gradually. — Hematoma: of different sizes on the affected area; in this case, a hematoma with pulsation indicates continued bleeding. The absolute sign of a fracture occurs as a result of direct destruction of the bone and indicates the completion of the process. These signs of a fracture are: - A characteristic crunch (crepitus): occurs when bone tissue ruptures, and is subsequently audible with a phonendoscope due to the friction of the fragments. — Unnatural direction of a limb or other bone. — Increased mobility in case of joint rupture. — Bone fragments are visible visually during an open fracture. - Shortening of the limb when fragments are displaced, protrusion of the broken bone. Some signs of a fracture without displacement or an incomplete fracture may not appear, which will complicate the diagnosis. The symptoms of a fracture are clearly determined by radiography - the location, type and degree of destruction are recorded.
Fracture treatment methods: what is done in the hospital
The basic principles of treatment in a hospital are preserving the patient’s life, eliminating anatomical disorders (muscle tension), restoring the functioning of internal organs and damaged limbs.
Operative methods
The main method of treating closed fractures is fixation of the joint using a plaster, splint or rigid orthoses. If bone fragments have shifted, then the treatment plan additionally includes traction—long-term comparison of fragments using a weight system.
There are also surgical treatment methods. Fractures are treated using osteosynthesis - connecting bone fragments using pins and screws.
Modern methods of treating fractures involve complete prosthetics. This is when the joint changes completely or partially. This is the “gold standard treatment” for hip fracture in elderly patients.
Conservative methods
After an injury, people experience pain, so they need to know what to take for fractures. Typically, in a hospital, patients, especially those with broken spines, are given narcotic painkillers - Codeine. After this, they switch to non-steroidal medications - Analgin, Ketarol.
After fractures, the risk of blood clots increases, so you additionally need to take drugs that prevent blood clotting, otherwise called anticoagulants - Heparin, Enoxaparin.
If the fracture is open, then it is necessary to prevent a bacterial infection that gets inside the wound. For this, antibiotics (Ceftriaxone or Cefotaxime) or antibacterial drugs (Metronidazole, Pefloxacin) are used.
How successful the treatment is will determine how long you will have to walk in a cast for a fracture. On average, the treatment period ranges from 1 to 2 months.
Physiotherapeutic method
Physiotherapy in the treatment of fractures is used for this purpose. to relieve swelling of soft tissues and relieve pain. The procedures promote rapid bone regeneration, as they improve blood supply to the injured area.
In the acute period, patients are prescribed treatment methods such as magnetic therapy (it is even done through a plaster cast). Magnetic therapy not only reduces pain, but also eliminates compression of soft tissues.
In addition to magnetic therapy, another effective treatment method is cryotherapy. But the procedure is only possible on those areas that are free from a plaster cast. The main purpose of cryotherapy is to relieve swelling from soft tissues due to the narrowing of blood vessels.
After the exacerbation stage subsides, ultrasound therapy with hydrocortisone and electrical stimulation are added to the listed physiotherapeutic treatment methods. These techniques help restore lost muscle volume after fractures.
Therapeutic physical education also plays an important role in treatment. After removing the plaster, you need to gradually develop the limbs and joints so that they acquire their initial mobility. Learn how to develop the radius and humerus after a broken arm from the video and advice from doctors.
Treatment
The main objectives of treating a victim with a fracture are saving his life and preserving the limb, restoring the integrity of the bone and the anatomical shape of the joint, the function of the damaged limb and the working capacity of the victim. First aid is aimed at preventing displacement of bone fragments, damage to soft tissues, wound infection, the development of traumatic shock and massive blood loss. Necessary actions: immobilize the damaged area of the skeleton using a splint that captures the joints above and below the site of injury. Stop the bleeding with a tourniquet and apply a sterile bandage to the wound. Give an anesthetic: analgin or promedol. Transport the victim to the emergency room. In case of multiple fractures and spinal injuries, it is not recommended to move the patient until the ambulance arrives. Conservative treatment consists of immobilization and the use of plaster casts after closed reduction of the fracture or without it (if there is no displacement). When applying plaster, the limb must be in the physiologically correct position. Its distal parts (for example, fingers in case of a fractured limb) must be open to be able to determine swelling and prevent disruption of tissue trophism. Sometimes traction is necessary for a fracture—the use of skeletal, cuff, adhesive, or adhesive traction. This method helps to neutralize the action of muscle layers that are attached to bone fragments, prevent their displacement and create conditions for bone tissue regeneration. Skeletal traction gives the greatest effect. A weight attached to a wire that is passed through the bone ensures that the bone fragments are maintained in a position that is optimal for tissue restoration. The disadvantage is the forced immobilization of the patient, leading to a deterioration in his general condition. For cracks in long bones and fractures of small bones, functional methods are used. They involve the absence of immobilization or minimal immobilization of the damaged area and are reduced to providing it with rest. Surgical treatment is necessary for jaw fractures (installation of an external fixation device), restoration of spongy bones (cranial vault), excessive formation of callus, etc. In the postoperative period, the fracture site is immobilized. Recovery time ranges from several weeks to several months. If bone restoration does not occur and a false joint is formed (persistent abnormal mobility at the fracture site), endoprosthetics methods are used (replacement of elements of the musculoskeletal system with implants). After the cast is removed, rehabilitation therapy begins. This is, first of all, a massage. Prescribed 10-45 days after the fracture. It accelerates the process of callus formation, improves blood circulation and tissue nutrition, and prevents muscle atrophy. CRM therapy is a passive development of joints (without the participation of muscles) using a specially tuned mechanical device. Physiotherapy. In the first 10 days, exercises are done for intact joints and limbs. They prevent muscle weakness and joint stiffness. After removing the cast, exercise therapy helps restore the mobility of damaged joints and muscle strength. It is recommended to increase the load gradually, completing rehabilitation with active gymnastics, which helps neutralize the consequences of the fracture.
Causes and types of displacement of bone fragments
When a bone is fractured, the displacement of fragments is caused by:
1) the primary effect of the force of the mechanical factor - the greater the force, the greater the displacement of the fragments;
2) antalgic muscle contraction - the body’s protective reaction to pain, causing muscle contraction;
3) the mass of the peripheral segment (earth gravity). The displacement depends on the place of attachment of individual muscles or their groups in the central and peripheral fragments, and their functional purpose.
So, the following types of displacement of fragments are distinguished:
1) in width;
2) in length;
3) along the axis;
4) rotation of the peripheral segment.
Overbone osteosynthesis with plates
Bone osteosynthesis is performed using plates of various lengths, widths, shapes and thicknesses, in which holes are made. Through the holes, the plate is connected to the bone using screws. For external osteosynthesis, wire (wrapped wire sutures) and other fixatives are also used.
The latest advancement in bone osteosynthesis is the angular stable plate (LCP). In addition to the threads on the screw, with which it is screwed into the bone and fixed in it, there are threads in the holes of the plate and in the screw head, due to which the head of each screw is firmly fixed in the plate. This method of fixing screws in the plate significantly increases the stability of osteosynthesis.
Plates with angular stability were created for each of the segments of all long tubular bones, having a shape corresponding to the shape and surface of the segment.
Plates for the proximal and distal humerus
Bony osteosynthesis allows for open reduction and perfectly accurate comparison of fragments (directly under visual control at the time of surgery). Therefore, it is the method of choice for osteosynthesis of intra-articular and periarticular fractures, since it is necessary to restore the anatomy of the articular surfaces so that there are no mechanical obstacles to movement in the joint.
Bimalleolar fracture.
This group includes both a fracture of the outer and inner ankles and a functionally bimalleolar fracture - a fracture of the outer malleolus and a rupture of the deltoid ligament. In most cases, surgical treatment is indicated. A combination of neutralizing, bridging, anti-slip plates, and compression screws is often used.
Osteosynthesis of a fracture of the outer malleolus using a compression screw and a neutralizing plate installed on the outer surface of the fibula, osteosynthesis of a fracture of the inner malleolus with two compression screws.
If the distal tibiofibular syndesmosis is damaged, which often occurs with suprasyndesmotic (high) fractures of the fibula, installation of a positioning screw is indicated for a period of 8-12 weeks with the complete exclusion of axial load.
When treating a functional bimalleolar fracture, there is no need to suture the deltoid ligament if it does not interfere with reduction, that is, if the position of the talus is satisfactory. When it is tucked into the joint cavity, it is impossible to eliminate the subluxation closed; for this reason, access to the inner ankle is performed, removal of the joint block and suture of the deltoid ligament.