Publications in the media
Pelvic fractures account for 4–7% of all fractures. Classification • Marginal fracture: fractures of the iliac spines, ischial tuberosities, coccyx, transverse fracture of the sacrum below the sacroiliac joint, ilium • Fracture of the pelvic ring without breaking its continuity •• Unilateral or bilateral fracture of the same branch of the pubic bone •• Unilateral or bilateral fracture of the ischium •• Fracture of one branch of the pubis on one side and the ischium on the other • Injuries with disruption of the continuity of the pelvic ring •• Vertical fracture of the sacrum or fracture of the lateral mass of the sacrum •• Rupture of the sacroiliac joint •• Vertical fracture ilium •• Fracture of both branches of the pubic bone on one or both sides •• Fracture of the pubis and ischium on one or both sides (butterfly type fracture) •• Rupture of the symphysis • Damage with simultaneous disruption of the continuity of the anterior and posterior half rings (Malgenia type ). and posterior on the other •• Dislocation of the innominate bone - rupture of the sacroiliac joint and symphysis •• Combination of rupture of the symphysis with a fracture of the posterior semi-ring or combination of rupture of the sacroiliac joint with a fracture of the anterior semi-ring of the pelvis • Fracture of the acetabulum •• Fracture of the edge of the acetabulum; may be accompanied by posterosuperior hip dislocation •• Fracture of the floor of the acetabulum; may be accompanied by a central dislocation of the hip - a displacement of its head inward towards the pelvic cavity.
Fracture of the marginal pelvic bones • Causes: direct trauma, short-term compression of the pelvis, sudden muscle contraction. • Detachment of the anterosuperior spine •• Clinical picture: pain, swelling, displacement of the fragment downwards and outwards, which creates the impression of a shortened limb; Lozinski's symptom of reverse movement - the appearance of sharp pain when flexing the hip while taking a step forward (moving the leg back causes less pain); the patient walks backwards •• Treatment: pain relief, the leg is placed on a Beler splint in a position of slight abduction for 3 weeks. Sometimes osteosynthesis is used. • Duvernay's fracture is a fracture of the ilium and the upper part of the acetabulum •• Clinical picture: pain in the area of the iliac wing, aggravated by tension of the abdominal muscles and percussion, limitation of movements in the hip joint. When the wing is displaced upward, a shortening of the distance from the xiphoid process to the anterosuperior spine is detected •• Treatment: pain relief - intrapelvic blockade according to Shkolnikov-Selivanov, Beler splint, exercise therapy, physiotherapy; if there is significant displacement, the patient is placed in a hammock with compression of the lateral surfaces of the pelvis for 4 weeks. • Transverse fracture of the sacrum and coccyx •• Clinical picture : pain, aggravated in a sitting position, pressing on the distal part of the sacrum during rectal examination, difficulty in defecation, swelling in the area of the sacrum (coccyx), pathological mobility of the distal fragment of the coccyx (sacrum). If the sacral nerves are damaged, urinary incontinence and anesthesia of the buttock area develop •• Treatment: pain relief, the patient is placed in bed on a backboard (a wide cushion is placed under the lower back so that the sacrum does not touch the bed) or in a hammock (the hammock is placed under the back from the angle of the shoulder blades to fracture area so that the distal fragment of the sacrum does not touch the bed) for 3–5 weeks, belladonna suppositories, warm enemas, physiotherapy; if pain persists, presacral blockades and physical therapy are repeated; if conservative treatment is ineffective, the fragment is removed.
Fracture of the pelvic ring • Fracture of the pelvic ring without breaking its continuity •• Causes : direct trauma, compression of the pelvis in the anteroposterior direction (fracture of the ischium) or load on the greater trochanter (fracture of the pubis) •• Clinical picture : pain in the pubic area (with a fracture pubic bones) or in the perineum (with a fracture of the ischial bones), aggravated by palpation, leg movements, compression of the pelvis from the sides; sometimes - a symptom of a stuck heel •• Treatment: anesthesia, the patient is placed on a hard bed with a shield; for a unilateral fracture - a Beler splint in the position of abduction of the leg; for bilateral fractures - the “frog” position. Bed rest - 4-5 weeks. • Fracture of the pelvic bones with disruption of the continuity of the pelvic ring •• Frequency : up to 50% of all pelvic injuries •• Complications : shock, damage to the pelvic organs (rectum, bladder, urethra) •• Causes: indirect injury - anteroposterior or lateral compression of the pelvis , fall from a height, birth injury (rupture of the symphysis) •• Damage to the anterior semi-ring of the pelvis ••• Clinical picture: pain in the pelvis and perineum, aggravated by leg movement, anteroposterior and lateral compression, an attempt to separate the iliac bones; Volkovich's symptom - with a fracture of the upper branch of the pubic and ischial bones, the patient is in a frog position; with a fracture near the symphysis and its rupture, the thighs are brought together and slightly bent, an attempt to separate them causes sharp pain; stuck heel symptom; when the symphysis is torn, the space between the bones is sometimes palpable ••• X-ray examination. It must be remembered that the width of the symphysis pubis at 18 years of age is 6 mm, later it decreases to 2 mm ••• Treatment: fractures without displacement - Volkovich position for 5-6 weeks, from the end of 1 week - exercise therapy, physiotherapy; fracture of the pubic and ischial bones on both sides (butterfly-type fracture) with displacement - Volkovich position; when the X-shaped fragment is displaced upward, additional pillows are placed under the back to bring together the attachment points of the rectus abdominis muscles; if ineffective, skeletal traction with a load of 4–5 kg; symphysis rupture - treatment on a hammock with cross traction; osteosynthesis is used when conservative treatment is unsuccessful; in the postoperative period - treatment on a hammock with cross traction for 6 weeks •• Damage to the posterior semi-ring ••• Clinical picture: the patient lies on the healthy side, active movements of the leg on the injured side are limited, painful, pain increases with palpation; if the sacroiliac joint is ruptured, the posteriorly displaced edge of the ilium is palpated ••• Treatment: the patient is placed on a backboard in a hammock without cross traction for 8–9 weeks; for displaced fractures - skeletal traction; if it is impossible to reposition a rupture of the sacroiliac joint with displacement, arthrodesis of the sacroiliac joint is used •• Malgenya fracture - simultaneous disruption of the continuity of the anterior and posterior half rings ••• Causes: compression of the pelvis, fall from a height ••• Clinical picture: pain, dysfunction of the lower limbs, bruises in the area of the scrotum, perineum and inguinal ligament, asymmetry of the pelvis, upward displacement of one of its halves by 2–3 cm - a decrease in the distance from the xiphoid process to the anterosuperior spine; with lateral compression or an attempt to separate the halves of the pelvis, pathological mobility is revealed ••• Treatment. Antishock therapy - intrapelvic anesthesia, compensation of blood loss; for a non-displaced fracture - treatment on a hammock, skeletal traction with a load of 4-5 kg on each leg for 8 weeks; when half of the pelvis is displaced upward and inward on the side of displacement, the load of skeletal traction is increased to 10–14 kg, traction is carried out in the abduction position for 8–10 weeks; the hammock is used only after reposition; in case of a bilateral vertical fracture with upward and inward displacement - skeletal traction with a load of 10–14 kg for both legs in the abduction position for 8–10 weeks; in case of symphysis rupture - treatment on a hammock with cross traction after reposition for 10–12 weeks.
Fracture of the acetabulum • Causes : lateral compression of the pelvis in the area of the greater trochanters, load on the greater trochanter • Clinical picture: pain in the hip joint and dysfunction (pain intensifies with axial load and tapping on the thigh); with combined dislocation, the apex of the greater trochanter is above the Roser–Nelaton line, the limb is adducted, slightly bent and internally rotated; with central dislocation of the hip, the greater trochanter falls • Treatment •• Anesthesia: intrapelvic blockade according to Shkolnikov-Selivanov •• Fracture without displacement - skeletal traction with a load of up to 5-7 kg, if closed reduction is unsuccessful - osteosynthesis of the broken edge of the acetabulum •• For fractures of the acetabular floor depressions accompanied by central dislocation of the hip, skeletal traction along the axis of the hip and beyond the greater trochanter or subtrochanteric region, transosseous compression-distraction osteosynthesis; if closed reduction is ineffective, open reduction of the central dislocation of the hip and osteosynthesis of fragments of the acetabulum.
ICD-10 • S32 Fracture of the lumbosacral spine and pelvic bones
Causes of pelvic fractures
The main causes of pelvic fractures are high-energy injuries, which can be caused by the following circumstances:
- Impacts during road traffic accidents.
- Compression of the pelvis during collapse of any structures.
- Falling from height.
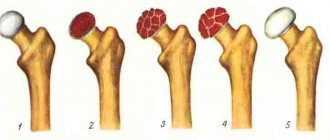
- Decrease in bone quality in older people caused by osteoporosis. In such cases, fractures are observed when falling even from one’s own height.
- Pelvic injuries at the muscle attachment site in young athletes caused by immaturity of the skeletal system.
Rehabilitation after a pelvic fracture
A pelvic fracture is a severe injury to the musculoskeletal system and requires a professional approach from specialists not only in diagnosis and treatment, but also in carrying out rehabilitation measures until the victim’s complete recovery.
Depending on the severity of the fracture, complete recovery from pelvic injuries may take from one and a half to six months. Individual complexes developed specifically for each case and including a number of the following activities will help with this:
- Daily physical therapy to maintain muscle tone, including special exercises to prevent the development of ankylosis, contractures and other complications in the joints.
- Taking special medications that help strengthen bones and nourish them with collagen for complete restoration of the musculoskeletal system.
- The use of ointments, creams and gels that restore joint function and relieve pain and swelling of tissues.
- Therapeutic massage, physiotherapy.
- Walking in the fresh air with a gradual increase in their duration.
- Proper diet. Consumption of foods high in calcium: sea and river fish, dairy products, herbs, vegetables, nuts, persimmons, green beans, poppy seeds, sesame seeds, rose hips.
First aid for a pelvic fracture
Correctly provided first aid at the slightest suspicion of a fracture of the pelvic bones will help to avoid unpleasant consequences, and the speed and professionalism of those nearby will prevent death if the victim has severe pelvic injuries.
In the event that doctors are immediately next to the victim, the first step is to relieve the shock symptom and reduce the pain syndrome. To do this, pain relief is carried out, in particular, the introduction of special medications directly into the fracture site (pain blockades). If the injury is accompanied by bleeding, it is necessary to treat open wounds, apply pressure bandages to bleeding vessels, and in case of significant blood loss, restore blood circulation. Only after this the patient should be carefully transferred to a stretcher and transported to the nearest medical facility.
However, doctors are not always immediately available, which is why up to 30% of victims with isolated trauma are admitted to the hospital in a state of traumatic shock. Statistics show that death in such cases occurs in 6% of cases. This is one third lower than in those hospitalized with multiple pelvic fractures, where shock is observed in almost all victims, and death occurs in 20% of cases, mainly as a result of heavy internal bleeding.
Before doctors arrive, it is especially important to properly prepare the victim for transportation. Below is an approximate algorithm of actions of rescuers located next to the victim:
- Call the doctors, assess breathing, pulse and examine the victim for injuries.
- Provide rest to the victim and, if necessary, immobilize the cervical spine.
- Relieve pain shock with affordable medications, if they are at hand. For those who are conscious and without obvious signs of severe injuries to the pelvic organs, two Analgin tablets and one Diphenhydramine tablet (or Aspirin with butadione), as well as strong sweet coffee, are recommended as an anesthetic.
- Drink plenty of warm fluids to relieve traumatic shock. It is recommended to give the victim warm water (up to 3-4 liters), adding 1 tbsp. a spoonful of table salt and 1 teaspoon of baking soda for every liter.
- Give the patient tincture of valerian (up to 20 drops) and 20 drops of cordiamine (Valocordin or Corvalol) to prevent heart failure and calm down in order to avoid complications during transportation.
- Place the injured person with his back on a hard surface, for example, a shield covered with a mattress or a door removed from its hinges, in the “frog” position: with legs half-bent at the knee joints, raised by about 30 cm, a pillow or an improvised bolster placed under them, knees apart.
- Wrap a scarf, sheet or other available material around the pelvis to prevent further displacement of the broken pelvic bones.
- Cover the limbs, if they are not injured, with heating pads (bottles) with hot water and wrap the victim warmly, regardless of the air temperature.
- Constantly monitor the pulse until the doctors arrive and, if it is difficult to determine, raise the foot end of the improvised stretcher by 30–45 cm.
In cases where it is impossible to call an ambulance, the victim must be transported on his own. In such cases, it is necessary to gently fix his knee joints and feet and strap the injured person to an improvised stretcher.
How long does it take for a pelvic fracture to heal?
A pelvic fracture is a serious injury, the outcome of treatment of which determines the future fate of a person. If the treatment is incorrect or the patient does not follow medical instructions, the bones may heal incorrectly and cause permanent problems in the future.
In general, it can take four to six months for the pelvic bones to heal and recover from injury, but for severe injuries, full recovery can take years. Despite advances in the field of modern traumatology, the number of people with disabilities after pelvic injuries remains quite significant (approximately 15%). In addition, pelvic injuries almost always derail the careers of professional athletes.
Although there is no specific time frame for complete healing of such injuries, there are a number of factors that are taken into account when making a prognosis.
These include the following:
- Type of fracture: open or closed.
- The location of the damage and the number of injured bones and tissues.
- Level of blood supply to damaged bones.
- Age of the victim: It can take six months for the bones of adults to heal, but only one for children.
- General health: level of bone mineralization, blood and muscle tissue.
- Presence of aggravating factors: bad habits, concomitant and chronic diseases, etc.