- home
- general surgery
- Gastroesophageal reflux disease
- Reflux esophagitis
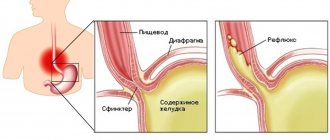
As a result of regularly repeated spontaneous reflux of gastric and/or intestinal contents into the esophagus, which have an irritating effect, an inflammatory process develops in the wall of the lower esophagus - reflux esophagitis. This chronic relapsing disease can be considered the most common among adults. Reflux esophagitis is diagnosed in 30% of adult patients, although the figures are very approximate, since many simply do not go to the doctor.
Causes of reflux esophagitis
The disease develops due to contact of the contents of the stomach and duodenum with the mucous membrane of the esophagus, which occurs when the lower esophageal sphincter, located at the border of the stomach and esophagus, is incompetent. As a result of impaired motility of the organs of the gastroesophageal zone, acidic gastric contents, being in the esophagus for a certain time, damage the cells of the mucosa.
Factors contributing to the development of reflux esophagitis are hiatal hernia - hiatal hernia, excess weight, pregnancy, leading to increased intra-abdominal pressure, taking certain medications, and smoking.
You can ask questions and sign up for a consultation by phone: +7 (495)222-10-87
or fill out the form below
Thank you, your question has been sent successfully, we will contact you soon!
Ask a new question
Prevention of GERD
It is impossible to predict the development of gastroesophageal reflux disease in a particular person. Therefore, the disease is difficult to prevent. If there is a hereditary predisposition, it is recommended for prevention:
- eliminate physical activity that increases pressure in the peritoneum;
- lead a healthy lifestyle without bad habits;
- harden the body;
- promptly treat gastrointestinal diseases;
- regularly diagnose parasitic infestations and, if necessary, undergo treatment;
- eat properly, in portions, regularly and in a balanced manner;
- avoid stress, severe nervous shock;
- treat psychoemotional diseases.
Interesting fact: every day, more than 10% of all energy expended is spent on digesting food. It is most difficult for the gastrointestinal tract to digest alcoholic products and animal proteins. You can relieve the gastrointestinal tract by giving up alcohol and changing the way you prepare meat dishes. It is strictly not recommended to combine alcohol with fatty snacks!
Not all patients can boldly say: “I cured GERD.” An innovative approach to treatment at the ACMD clinic will help you achieve a complete recovery!
Symptoms
The clinical picture depends on the severity of the inflammatory process and the condition of the esophageal sphincter; reflux esophagitis is accompanied by a complex of dyspeptic, pulmonary and cardiac disorders. The main symptoms of reflux esophagitis are:
- Heartburn, manifested as a burning sensation behind the sternum, in the area of the xiphoid process, is the most characteristic symptom, occurring in more than ¾ of patients. Unpleasant and painful sensations can appear after eating, during physical activity, bending the body, and even in a horizontal position; wearing a tight belt can provoke heartburn.
- Belching that occurs after eating or carbonated drinks is the second most common symptom of reflux esophagitis. It can appear even in a horizontal position of the body, but more often during physical activity.
- Dysphagia is difficulty passing food that occurs when the motility of the upper parts of the digestive tract is impaired or when stricture is a narrowing of the lumen of the esophagus.
- Odynophagia is a retrosternal or interscapular pain that occurs when food passes through the esophagus. Painful sensations can radiate to the intercostal space and even resemble an angina attack.
- Regurgitation is regurgitation in which the contents of the stomach enter the oral cavity. Appears regardless of body position and physical activity of a person.
There are also extraesophageal manifestations involving other organs, e.g.
- bronchopulmonary: cough, attacks of respiratory discomfort or suffocation at night; the cause is the entry of small particles of stomach contents into the bronchi;
- otolaryngological: hoarseness, signs of rhinitis, pharyngitis due to refluxant entering the larynx;
- dental: thinning of tooth enamel, caries as a result of the aggressive action of acid.
If left untreated, reflux esophagitis can cause severe complications. If the wall of the esophagus is damaged down to the submucosal layer, there is a risk of ulcer formation, which can cause bleeding. Scars formed after healing can lead to stricture, a narrowing of the esophagus.
The most severe complication is Barrett's esophagus syndrome - the squamous epithelium characteristic of the esophagus is replaced by a cylindrical epithelium characteristic of the gastric mucosa. With metaplasia, the likelihood of developing cancer increases by more than 30 times.
Classification
To assess the patient’s condition and unify data, a classification is used; depending on the degree of damage to the esophagus, several stages of reflux esophagitis are distinguished.
- I - rounded and longitudinal delimited, non-merging foci of inflammation, spreading to the mucous membrane of the esophagus from the Z-line - the border of the transition of the multilayered squamous epithelium of the esophageal mucosa into the columnar epithelium of the gastric mucosa;
- II - lesions in the Z-line zone merge, but do not cover the entire circumference of the esophagus;
- III - merging lesions covering the entire surface of the mucosa;
- IV - chronic damage to the esophagus, in which fibrous stenosis, shortening of the esophagus, peptic ulcers, and Barrett's esophagus develop.
To determine the stage of reflux esophagitis, it is necessary to undergo an examination, based on the results of which treatment is prescribed.
Indications for hospitalization of patients with GERD
- esophagitis grades C, D without complications or Barrett's esophagus (hospitalization of the patient to the therapeutic, gastroenterological departments of the district health care organization (hereinafter - RHO), city health care organization (hereinafter - GOZ), regional health care organization (hereinafter - OHO));
- esophagitis with complications (bleeding, penetration, stenosis) (hospitalization of the patient to the surgical department of the ROZ, GOZ, OZ);
- GERD with a course resistant to treatment and the need to clarify the diagnosis (hospitalization of the patient to the gastroenterology department of the state health department or public health unit).
Diagnostics
There are various diagnostic methods that can accurately determine the degree of damage to the esophagus. This is evidenced by the presence of changes due to the inflammatory process, erosions, ulcers, strictures, and metaplasia. The main diagnostic methods include:
- Fibrogastroscopy is an examination of the upper parts of the gastrointestinal tract using endoscopic equipment; during the procedure, it is possible to identify abnormalities in the wall of the esophagus, assess the condition of the mucous membrane, and exclude or confirm diseases of the stomach and duodenum. During the examination, a biopsy can be performed - taking tissue particles from visible pathological areas for the purpose of further histological examination.
- X-ray examination allows you to detect a stricture of the esophagus, ulcerative lesions, hiatal hernia, its size, it is also possible to assess the motility of the esophagus and stomach, the presence of reflux during examination using a barium suspension.
- Daily pH-metry - determination of the level of gastric secretion and the presence of reflux; it is possible to estimate the duration of reflux episodes, which allows you to select therapy and monitor the effectiveness of the drugs used.
- Esophageal manometry is an examination that allows you to determine the tone of the esophageal sphincters and their patency based on measuring pressure in different parts.
- pH impedansometry is a study aimed at assessing esophageal peristalsis and differentiation of gastroesophageal reflux, which is important for determining the nature of the disease and its cause.
Depending on the presence of certain symptoms, other examinations may be prescribed: ultrasound, ECG, consultation with an otolaryngologist, etc. In our clinic, patients have access to all the necessary diagnostic procedures, the examination takes a minimum of time.
GERD in children
Reflux esophagitis in children with diseases of the gastrointestinal tract is detected in 17% of cases (approximately). The exact prevalence of GERD in childhood is unknown, due to the variety of clinical manifestations of the disease.
Important information! The process of GERD itself can be quite natural for a child under one year of age. Due to the insufficient length and immaturity of the esophagus, stomach contents regularly enter it, and from there into the throat and oral cavity. In common parlance this is called regurgitation.
Signs of GERD in childhood are varied and numerous. You can suspect a disease in a child by:
- regular severe vomiting after eating;
- frequent belching with a sour aroma;
- prolonged hiccups;
- morning cough;
- a feeling of bitterness in the mouth;
- chest pain;
- night snoring;
- attacks of difficulty breathing;
- thinning and darkening of tooth enamel.
Treatment of gastroesophageal reflux disease in children is not much different from therapy for adults. Often the child outgrows the disease on his own, and it disappears without a trace, forever.
Treatment
Conservative treatment is indicated for patients with mild manifestations. Drug therapy can be aimed at neutralizing the contents thrown from the stomach into the esophagus, reducing gastric acidity, and protecting the esophageal mucosa.
There are various drugs: antisecretory agents, prokinetics and antacids, but they can only eliminate the symptoms. At the end of the course of treatment, signs of the disease return again. It is also worth considering that long-term use of medications that suppress the production of gastric juice can lead to poor digestion of food, which will lead to a number of disorders. When using medications that affect acidity, the risk of malignancy increases.
How is GERD diagnosed?
If symptoms of reflux pathology appear, you should contact your family doctor or directly a gastroenterologist. First of all, the doctor carefully studies the clinical picture and complaints of the patient. Often the diagnosis can be made only by the clinical picture, without additional research. Sometimes the patient is prescribed additional diagnostic procedures, namely:
- endoscopy is the most informative way to diagnose GERD , which consists of visually studying the structure of the esophagus (helps determine narrowing, the presence of erosions and ulcers, changes in the composition of the epithelium);
- daily monitoring of the pH level in the esophagus - helps to assess the nature and synchronicity of the reflux of stomach contents into the esophagus;
- X-ray examination of the esophagus with barium - allows you to identify narrowings and hernias of the esophageal passage of the diaphragm.
Interesting fact: a healthy esophagus is able to push food into the stomach when swallowed in any body position, even when a person is lying upside down. And all thanks to proper peristalsis (muscle contractions).
Surgery
If conservative treatment is ineffective, if complications arise, if there is an esophageal hernia, as well as if there is pain behind the sternum or if there are extra-esophageal signs (cough, hoarseness, etc.), surgical treatment is recommended - fundoplication. The purpose of surgery for reflux esophagitis is to restore normal anatomical relationships in the area of the esophagus and stomach, creating a mechanism that will prevent the reflux of gastric contents into the esophagus.
Most surgeons in domestic clinics perform circular Nissen fundoplication; during the operation, a cuff is created - the fundus of the stomach is wrapped around the esophagus 360°, which prevents reflux in the future. But a valve formed in this way leads to the loss of natural protective mechanisms: the ability to regurgitate and vomit. Large portions of food and drinking carbonated drinks lead to the fact that, if necessary, their removal through the cardia is impossible, discomfort and pain appear. The formed cuff often slips off after 1-2 years, which leads to relapse of the disease.
Conservative therapy
For conservative therapy, the following groups of drugs are used:
- antacids and alginates
- proton pump inhibitors
- prokinetics
Antacids and alginates
Antacids and alginates, topical preparations most often containing aluminum and magnesium salts, these drugs act locally, are not absorbed into the blood and do not have a systemic effect. Their advantage is safety of use, but there is also a disadvantage, a short duration of action. Antacids are not used as an independent method of treatment, but are used as first aid for heartburn, and as an intensification of therapy for the speedy healing of erosions and ulcers of the esophagus. Preparations in the form of gels with alginic acid have proven themselves to be the best, which, when interacting with acid in the lumen of the stomach, form foam, thereby increasing the duration of action of the drug and its effectiveness. Antacids are most often prescribed 40 minutes after meals and at night, or on demand in case of heartburn.
Proton pump inhibitors (PPIs)
Today they are the main drugs in the treatment of reflux esophagitis, these include the well-known omeprazole, lansoprazole, rabeprazole, etc. These are systemic drugs, they block the transport of hydrogen molecules into the parietal cells of the stomach, responsible for the secretion of hydrochloric acid, and how do we We remember from the school chemistry course, this acid consists of a molecule of hydrogen and chlorine, no hydrogen, no acid. These drugs have revolutionized the treatment of reflux esophagitis, significantly improving the outcome and reducing the number of complications. Previously, H2 histamine receptor blockers were used, which were much less effective and had more side effects. It must be said that these drugs are sometimes used now in combination with PPIs to enhance the effect. The main disadvantage of proton pump inhibitors (PPIs) is their fairly rapid removal from the blood, which requires repeated use throughout the day, and even with double use, so-called acid breakthroughs are described, when, more often at night, the acidity of gastric juice sharply increases. Most often, PPIs are prescribed 20 mg twice a day 20 minutes before meals, morning and evening for 6 to 8 weeks. Then maintenance therapy is prescribed at 10 mg per day or 10 mg twice a day.
Prokinetics
Prokinetics are drugs that improve and normalize peristalsis of the gastrointestinal organs, including the esophagus. The most commonly prescribed drug is itopride, which is considered the most effective and safe drug. Motilium is also prescribed. The previously popular cerucal has recently been deprecated due to its central effect on the brain. Prokinetics are prescribed 1 tablet three times a day 20 minutes before meals. A course of 2 weeks is recommended.
Problems of conservative therapy
The vast majority of patients with reflux esophagitis are treated conservatively, achieving good functional results, but unfortunately, therapy is not always effective. As we wrote above. The cause of reflux esophagitis is the reflux of gastric contents into the esophagus. So the first problem with conservative therapy is that it does not eliminate the cause, but only relieves the symptoms. With conservative therapy, reflux remains, but is no longer acidic, and therefore patients do not feel any complaints. Although some researchers believe that due to the neutralization of acid, bile begins to flow into the esophagus, since it ceases to be inactivated in the stomach, and bile is an even more aggressive environment for the development of complications of esophagitis. Although it should be noted that this is still a theory that has not received sufficient confirmation. But at the same time, a number of scientists associate the growth of esophageal cancer with this hypothesis. Since, despite the widespread use of PPI drugs, the incidence of esophageal cancer is steadily increasing.
Taking medications in itself can cause complications. Evidence has been obtained that proton pump inhibitors increase the risk of stroke, osteoporosis and heart attack, and although the risk is not quite high, about 0.4 - 0.6% per year, it is still there.
Well, perhaps the main thing is that the effect of conservative therapy is temporary and is not always sufficiently effective. So, 6 months after stopping therapy, complaints return in 40-50% of patients, and after 12 months in 80-90%, that is, most patients are forced to take medications daily for many years. Considering the sufficient safety of the drugs, this may not be scary, although it certainly reduces the quality of life. But the problem lies in the fact that with long-term therapy, after three or five years, the effectiveness of the drugs decreases and in 20 - 30% of patients complaints reappear and complications of esophagitis develop, despite the constant use of the prescribed drugs.
My approach to treatment
When surgically treating patients with reflux esophagitis, I, like most specialists in European clinics, use a more effective technique that does not have the above-mentioned disadvantages - partial Toupet fundoplication with a cuff rotation of 270°. The technique I improved has a number of advantages:
- the physiological functioning of the esophageal sphincter is restored;
- maintaining a functional esophagogastric valve allows the patient to do without medications throughout his life;
- the ability to belch and vomit—the body’s natural defense reactions—is preserved;
- no pain after overeating or carbonated drinks;
- the number of relapses does not exceed 2% within a year after surgery, after 5 years this figure is about 4%.
A Russian Federation patent has been issued for an improved technique - Toupet 270° fundoplication.
Reflux esophagitis
How is the operation performed using a modified technique?
During the operation, a symmetrical cuff is formed from the upper part of the stomach, covering the esophagus at 270°. The anterior right side of the esophagus remains free; The cuff created in this way strengthens the lower esophageal sphincter and prevents the backflow of stomach contents. In the presence of a hiatal hernia, the lower part of the esophagus and the upper third of the stomach are first separated from the adhesions and returned to their natural position. The diaphragmatic hole is sutured to normal size. To prevent relapse and perform diaphragmocruroplasty, I use mesh implants, which reduces the risk of recurrence of the disease from 65% to 1%.
Surgery for reflux esophagitis is performed through laparoscopic access: all manipulations are performed through several small punctures on the anterior abdominal wall. In the future, the puncture marks become almost invisible. The operation is performed using endoscopic equipment equipped with a miniature video camera, which allows all manipulations to be carried out under visual control as accurately as possible. Since important structures (vagus nerve, blood vessels) are located in the surgical area, there is virtually no risk of damage to them.
During the operation, when isolating the esophagus and stomach, I use a dosed tissue ligation device LigaSure (USA), which is capable of “sealing” vessels without the risk of damage to surrounding tissues, as well as the development of bleeding. At the same time, the duration of the operation is reduced. The use of modern suture material promotes rapid recovery.
Advantages of laparoscopic surgery
- Less traumatic and no pain in the postoperative period;
- Short period of hospitalization - no more than three days;
- Rapid recovery - after two weeks, patients return to their normal lifestyle.
Since patients often have other diseases that require surgical treatment, so-called simultaneous operations can be performed using laparoscopic access. I have been performing similar interventions for more than two decades. When performing a simultaneous operation during one anesthesia, you can immediately get rid of 2-5 surgical pathologies (for example, calculous cholecystitis, cholelithiasis, tumors, cysts, etc.).
Many, even experiencing painful attacks of heartburn, are in no hurry to see a doctor, trying to alleviate the condition in various ways, including with the help of medications. Is it necessary to treat reflux esophagitis if the symptoms are eliminated with the help of drugs that can be bought at any pharmacy? Of course, since there is a risk of developing severe complications. In addition, in the absence of adequate treatment, you will have to take medications throughout your life and adhere to strict dietary restrictions. At the same time, the effect of the drugs is very short-lived, and any physical activity immediately causes unpleasant and even painful sensations. To determine the extent of the disease and choose the most appropriate treatment tactics, just contact me by email or by scheduling a consultation.
Carrying out surgical interventions for diseases of the esophagus and stomach requires excellent command of surgical techniques, including endoscopic suture, which is impossible without appropriate experience. Over more than 25 years of experience, I have performed more than 2000 surgical interventions for reflux esophagitis, GERD and hiatal hernia. I am the author of monographs and more than 50 scientific papers devoted to these problems. I also regularly conduct seminars and master classes on these diseases, which are attended by specialists from various clinics and centers.
Modern treatment of gastroesophageal reflux disease
Treatment for GERD is aimed at combating symptoms and preventing consequences. It can be conservative and medicinal. First, doctors suggest the patient try to change their lifestyle:
- get rid of excess weight;
- switch to a normal regime of wakefulness and rest;
- give up bad habits (smoking, alcohol);
- switch to a balanced, gentle diet.
Diet is the main method of non-drug treatment of GERD. You need to eat small portions 5 times a day. It is recommended to avoid evening overeating (the last meal should be at least 2 hours before bedtime). You need to include more vegetables in your diet. Meat should be consumed after boiling or steaming. Spices, fatty foods, fried foods, carbonated drinks, and sour fruits are excluded from the diet. Dishes should not be too hot or cold.
Patients should avoid situations that increase abdominal pressure. You cannot wear tight trousers, belts, corsets, sweaters, or bandages. It is not recommended to jump, lift weights, or perform intense exercises that strain the abdominal muscles. Ideal sports for people with GERD: swimming, cycling, walking.
If heartburn attacks occur only when lying down, it is recommended to raise the head of the bed or choose a larger pillow. You should not lie down immediately after eating or drinking.
The patient will have to give up medications that can provoke attacks of GERD. Such drugs include:
- nitrates and nitrate-like agents;
- nifedipine, Theophylline, Progesterone;
- antidepressants and antispasmodics;
- non-steroidal anti-inflammatory drugs.
If symptoms of GERD persist, you need to switch to drug therapy. Help to get rid of the manifestations and complications of the disease:
- drugs from the group of proton pump inhibitors;
- combined antacids;
- dioctahedral smectite;
- prokinetics.
Drug treatment for GERD lasts from 4 to 8 weeks. After the main course, you need to undergo maintenance therapy lasting 6-12 months.
Complicated and advanced forms of GERD are treated surgically. To correct a defect in the esophagus, antireflux surgery is performed. In case of a hiatal hernia, a fundoplication is prescribed - suturing the stomach to the diaphragm around the opening of the esophagus, thereby creating a cuff that regulates the passage of food.