Esomeprazole Canon lyophilisate
Pharmacodynamics
Esomeprazole is the 5-isomer of omeprazole and reduces gastric acid secretion by specifically inhibiting the proton pump in gastric parietal cells. The 5- and R-isomers of omeprazole have similar pharmacodynamic activities.
Mechanism of action
Esomeprazole is a weak base that transforms into an active form in the highly acidic environment of the secretory tubules of the parietal cells of the gastric mucosa and inhibits the proton pump - the enzyme H + / K + -ATPase, thereby inhibiting both basal and stimulated secretion of hydrochloric acid.
Effect on the secretion of hydrochloric acid in the stomach
After oral administration of esomeprazole at a dose of 20 mg or 40 mg for 5 days, patients with gastroesophageal reflux disease (GERD) with symptoms experienced a decrease in the secretion of hydrochloric acid in the stomach for most of the day. The effect was the same when administered intravenously and when taken orally.
Analysis of pharmacokinetic data revealed the relationship between the inhibition of hydrochloric acid secretion and the concentration of esomeprazole in plasma after oral administration (the AUC parameter, the area under the concentration-time curve, was used to assess the concentration).
Following an intravenous infusion of 80 mg esomeprazole over 30 minutes followed by an extended intravenous infusion of 8 mg/hour esomeprazole for 23.5 hours, gastric pH was above 4 for an average of
21 hours, and above 6 - for 11-13 hours.
The therapeutic effect achieved by inhibiting the secretion of hydrochloric acid
Healing of reflux esophagitis with oral administration of esomeprazole in a dose
40 mg occurs in approximately 78% of patients after 4 weeks of therapy and in 93% of patients after 8 weeks of therapy. The effectiveness of esomeprazole in bleeding from peptic ulcers, confirmed endoscopically, has been shown.
Other effects associated with inhibition of hydrochloric acid secretion
During treatment with drugs that reduce the secretion of gastric glands, the concentration of gastrin in the plasma increases as a result of a decrease in the secretion of hydrochloric acid. Due to a decrease in the secretion of hydrochloric acid, the concentration of chromogranin A (CgA) increases. Increased concentrations of CgA may affect the results of examinations for the detection of neuroendocrine tumors. To prevent this effect, therapy with proton pump inhibitors should be suspended 5-14 days before testing CgA concentrations. If during this time the CgA concentration has not returned to normal, the study should be repeated.
In children and adult patients taking esomeprazole orally for a long period of time, an increase in the number of enterochromaffin-like cells was observed, which is likely due to an increase in plasma gastrin concentrations. This phenomenon has no clinical significance.
Patients who took drugs orally for a long time that reduce the secretion of gastric glands were more likely to develop glandular cysts in the stomach. These phenomena are caused by physiological changes resulting from inhibition of hydrochloric acid secretion. Cysts are benign and undergo reverse development.
The use of drugs that suppress the secretion of hydrochloric acid in the stomach, including proton pump inhibitors, is accompanied by an increase in the content of microbial flora in the stomach that is normally present in the gastrointestinal tract. The use of proton pump inhibitors may lead to a slight increase in the risk of infectious diseases of the gastrointestinal tract caused by Salmonella spp.,
Campylobacter spp.
and, in hospitalized patients, probably
Clostridium difficile.
In children less than 1 month of age and 1-11 months of age, oral esomeprazole 0.5 mg/kg and 1.0 mg/kg, respectively, showed a decrease in the mean percentage of time with intragastric pH less than 4. Profile The safety of esomeprazole in children is similar to that in adults.
Pharmacokinetics
Distribution
The apparent volume of distribution at steady state in healthy individuals is approximately 0.22 l/kg body weight. Esomeprazole is 97% bound to plasma proteins.
Metabolism and excretion
Esomeprazole undergoes complete metabolism with the participation of the cytochrome P450 system. The main part is metabolized with the participation of the specific polymorphic isoenzyme CYP2C19, resulting in the formation of hydroxylated and desmethylated metabolites of esomeprazole. The remainder is metabolized by the CYP3A4 isoenzyme; in this case, a sulfo derivative of esomeprazole is formed, the main metabolite detected in plasma.
The parameters given below mainly reflect the nature of pharmacokinetics in patients with increased activity of the CYP2C19 isoenzyme. The total plasma clearance is approximately 17 l/h after a single dose of the drug and 9 l/h with repeated administrations. The half-life is 1.3 hours with repeated administrations of the drug once a day. The area under the concentration-time curve (AUC) increases with repeated administration. This increase is time- and dose-dependent, resulting from a decrease in first-pass metabolism through the liver, as well as a decrease in systemic clearance, probably caused by the fact that esomeprazole and/or its sulfo derivative inhibits the CYP2C19 isoenzyme. With daily use once a day, esomeprazole is completely eliminated from the plasma in the interval between administrations; there is no tendency for esomeprazole to accumulate.
With repeated intravenous administration of esomeprazole at a dose of 40 mg, the average maximum plasma concentration is approximately 13.6 μmol/L. When administered orally at similar doses, the average plasma maximum concentration is 4.6 µmol/l. Total exposure increases slightly less (approximately 30%) with intravenous esomeprazole compared to oral administration.
Intravenous administration of esomeprazole at doses of 40 mg, 80 mg and 120 mg over 30 minutes followed by intravenous administration at a dose of 4 mg/hour or 8 mg/hour for 23.5 hours showed a linear dependence of AUC on the administered dose. The main metabolites of esomeprazole do not affect the secretion of hydrochloric acid in the stomach. When administered orally, up to 80% of the dose of esomeprazole is excreted in the form of metabolites by the kidneys, the other part by the intestines. Less than 1% unchanged esomeprazole is found in urine.
Features of pharmacokinetics in some groups of patients
Approximately 2.9±1.5% of the population has reduced activity of the CYP2C19 isoenzyme. In such patients, the metabolism of esomeprazole is mainly carried out by CYP3A4, and with repeated oral administration of 40 mg of esomeprazole once daily, the average area under the concentration-time curve is 100% higher than in patients with increased activity of the CYP2C19 isoenzyme. The average values of maximum plasma concentrations in patients with reduced isoenzyme activity are increased by approximately 60%. Similar differences were found with intravenous esomeprazole. The noted features do not affect the dose and method of administration of esomeprazole.
In elderly patients (71-80 years), the metabolism of esomeprazole does not change significantly.
In patients with mild to moderate hepatic impairment, the metabolism of esomeprazole may be impaired. In patients with severe hepatic impairment, the metabolic rate is reduced, resulting in a doubling of the area under the concentration-time curve for esomeprazole. There is no tendency for the accumulation of esomeprazole and its main metabolites when the drug is administered once a day.
Pharmacokinetic studies have not been conducted in patients with reduced renal function. Since it is not esomeprazole itself that is excreted through the kidneys, but its metabolites, it can be assumed that the metabolism of esomeprazole in patients with impaired renal function does not change.
Use in children
A study of the pharmacokinetics of esomeprazole in children aged 0 to 18 years was carried out after a 3-minute intravenous injection once a day for 4 days. The maximum steady-state concentration of the drug in blood plasma (Css,max) was assessed 5 minutes after administration of the dose in children in all age groups, and in adult patients - 7 minutes after administration of the 40 mg dose and at the end of the 20 mg dose infusion.
The table presents the results of assessing systemic exposure to esome-
prazole as geometric means (range).
| Age group | Dose | AUC µmol-h/l | Сss, max µmol/l |
| 0 - 1 month* | 0.5 mg/kg (n=6) | 7,5 (4,5 — 20,5) | 3,7 (2,7 — 5,8) |
| 1 – 11 months* | 1.0 mg/kg (n=6) | 10,5 (4,5 — 22,2) | 8,7 (4,5 — 14,0) |
| 15 years | 10 mg (n=7) | 7,9 (2,9 — 16,6) | 9,4 (4,4 — 17,2) |
| 6 – 11 years | 10 mg (n=7) | 6,9 (3,5 — 10,9) | 5,6 (3,1 — 13,2) |
| 20 mg (n=8) 20 mg (n=6)** | 14,4 (7,2 — 42,3) 10.1 (7,2 — 13,7) | 8,8 (3,4 — 29,4) 8,1 (3,4 — 29,4) | |
| 12 - 17 years old | 20 mg (n=6) | 8,1 (4,7 — 15,9) | 7,1 (4,8 — 9,0) |
| 40 mg (n=8) | 17,6 (13,1 — 19,8) | 10,5 (7,8 — 14,2) | |
| Adults | 20 mg (n=22) | 5,1 (1,5 — 11,8) | 3,9 (1,5 — 6,7) |
| 40 mg (n=41) | 12,6 (4,8 — 21,7) | 8,5 (5,4 — 17,9) |
*The 0 to 1 month age group included patients with a corrected age (sum of intrauterine age and postnatal age in completed weeks) >32 completed weeks and <44 completed weeks.
The 1 to 11 month age group included patients with a corrected age >44 completed weeks. **Two patients were excluded - one due to reduced activity of the CYP2C19 isoenzyme, the second due to the concomitant use of a CYP3A4 isoenzyme inhibitor.
According to the constructed model, Css,max after intravenous administration of esomeprazole in the form of a 10-minute, 20-minute and 30-minute infusion will decrease, on average, by 37%-49%, 54%-66% and 61%-72%, respectively, in all age groups and dosage groups compared to the Css,max value after a 3-minute injection.
Nexium
Esomeprazole is the S-isomer of omeprazole and reduces gastric acid secretion by specifically inhibiting the proton pump in gastric parietal cells. The S- and R-isomers of omeprazole have similar pharmacodynamic activities.
Mechanism of action
Esomeprazole is a weak base that transforms into an active form in the highly acidic environment of the secretory tubules of the parietal cells of the gastric mucosa and inhibits the proton pump - the enzyme H + / K + - ATPase, thereby inhibiting both basal and stimulated secretion of hydrochloric acid.
Effect on the secretion of hydrochloric acid in the stomach
The effect of esomeprazole develops within 1 hour after oral administration of 20 mg or 40 mg. When taking the drug daily for 5 days at a dose of 20 mg once a day, the average maximum concentration of hydrochloric acid after stimulation with pentagastrin is reduced by 90% (when measuring the acid concentration 6-7 hours after taking the drug on the 5th day of therapy). In patients with gastroesophageal reflux disease (GERD) and the presence of clinical symptoms, after 5 days of daily oral esomeprazole 20 mg or 40 mg, intragastric pH values above 4 were maintained for an average of 13 and 17 hours out of 24 hours. When taking esomeprazole at a dose of 20 mg per day, an intragastric pH value above 4 was maintained for at least 8, 12 and 16 hours in 76%, 54% and 24% of patients, respectively. For 40 mg esomeprazole, this ratio is 97%, 92% and 56%, respectively.
A correlation was found between the concentration of the drug in plasma and the inhibition of hydrochloric acid secretion (the AUC parameter (area under the concentration-time curve) was used to assess the concentration).
The therapeutic effect achieved by inhibiting the secretion of hydrochloric acid. When taking Nexium at a dose of 40 mg, healing of reflux esophagitis occurs in approximately 78% of patients after 4 weeks of therapy and in 93% after 8 weeks of therapy.
Treatment with Nexium at a dose of 20 mg 2 times a day in combination with appropriate antibiotics for one week leads to successful eradication of Helicobacter pylori in approximately 90% of patients.
Patients with uncomplicated peptic ulcer disease after a week-long eradication course do not require subsequent monotherapy with drugs that reduce the secretion of gastric glands to heal the ulcer and eliminate symptoms.
The effectiveness of Nexium for peptic ulcer bleeding was demonstrated in a study of patients with endoscopically confirmed peptic ulcer bleeding.
Other effects associated with inhibition of hydrochloric acid secretion. During treatment with drugs that reduce the secretion of gastric glands, the concentration of gastrin in the plasma increases as a result of a decrease in acid secretion. Due to a decrease in the secretion of hydrochloric acid, the concentration of chromogranin A (CgA) increases. Increased concentrations of CgA may affect the results of examinations for the detection of neuroendocrine tumors. To prevent this effect, therapy with proton pump inhibitors should be suspended 5-14 days before testing CgA concentrations. If during this time the CgA concentration has not returned to normal, the study should be repeated.
In children and adult patients receiving esomeprazole for a long time, there is an increase in the number of enterochromaffin-like cells, probably associated with an increase in plasma gastrin concentrations. This phenomenon has no clinical significance.
Patients taking drugs that reduce the secretion of gastric glands for a long period of time are more likely to develop glandular cysts in the stomach. These phenomena are caused by physiological changes as a result of pronounced inhibition of hydrochloric acid secretion. Cysts are benign and undergo reverse development.
The use of drugs that suppress the secretion of hydrochloric acid in the stomach, including proton pump inhibitors, is accompanied by an increase in the content of microbial flora in the stomach that is normally present in the gastrointestinal tract. The use of proton pump inhibitors may lead to a slight increase in the risk of infectious diseases of the gastrointestinal tract caused by bacteria of the genus Salmonella spp. and Campylobacter spp. and, in hospitalized patients, probably Clostridium difficile.
In two comparative studies with ranitidine, Nexium was shown to be superior in healing gastric ulcers in patients treated with nonsteroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors. In two studies, Nexium showed high efficacy in the prevention of gastric and duodenal ulcers in patients receiving NSAIDs (age group over 60 years and/or with a history of peptic ulcers), including selective COX-2 inhibitors.
Pharmacokinetics
Absorption and distribution
Esomeprazole is unstable in an acidic environment, so tablets containing granules of the drug, the shell of which is resistant to the action of gastric juice, are used for oral administration. Under in vivo conditions, only a small portion of esomeprazole is converted to the R-isomer. The drug is rapidly absorbed: maximum plasma concentration is reached 1-2 hours after administration. The absolute bioavailability of esomeprazole after a single dose of 40 mg is 64% and increases to 89% with daily dosing once daily. For a dose of 20 mg esomeprazole, these figures are 50% and 68%, respectively. The volume of distribution at steady state concentration in healthy people is approximately 0.22 l/kg body weight. Esomeprazole is 97% bound to plasma proteins.
Eating slows down and reduces the absorption of esomeprazole in the stomach, but this does not have a significant effect on the effectiveness of inhibition of hydrochloric acid secretion.
Metabolism and excretion
Esomeprazole is metabolized via the cytochrome P450 system. The main part is metabolized with the participation of a specific polymorphic isoenzyme CYP2C19, resulting in the formation of hydroxylated and demethylated metabolites of esomeprazole. The remainder is metabolized by the CYP3A4 isoenzyme; this produces a sulfo derivative of esomeprazole, which is the main metabolite detected in plasma.
The parameters given below mainly reflect the nature of pharmacokinetics in patients with increased activity of the CYP2C19 isoenzyme. The total clearance is approximately 17 l/h after a single dose of the drug and 9 l/h after repeated doses. The half-life is 1.3 hours when taken systematically once a day. The area under the concentration-time curve (AUC) increases with repeated dosing of esomeprazole. The dose-dependent increase in AUC with repeated administration of esomeprazole is non-linear, which is a consequence of a decrease in first-pass metabolism through the liver, as well as a decrease in systemic clearance, probably caused by inhibition of the CYP2C19 isoenzyme by esomeprazole and/or its sulfo derivatives. When taken daily once a day, esomeprazole is completely eliminated from the blood plasma in the interval between doses and does not accumulate.
The main metabolites of esomeprazole do not affect the secretion of gastric acid. When administered orally, up to 80% of the dose is excreted in the form of metabolites in the urine, the rest is excreted in feces. Less than 1% unchanged esomeprazole is found in urine.
Features of pharmacokinetics in some groups of patients.
Approximately 2.9±1.5% of the population has reduced activity of the CYP2C19 isoenzyme. In these patients, esomeprazole is metabolized primarily through the action of CYP3A4. When systematically taking 40 mg of esomeprazole once a day, the average AUC value is 100% higher than the value of this parameter in patients with increased activity of the CYP2C19 isoenzyme. The average values of maximum plasma concentrations in patients with reduced isoenzyme activity are increased by approximately 60%. These features do not affect the dose and method of administration of esomeprazole. In elderly patients (71-80 years), the metabolism of esomeprazole does not undergo significant changes.
After a single dose of 40 mg esomeprazole, the average AUC value in women is 30% higher than that in men. When taking the drug daily once a day, there are no differences in pharmacokinetics between men and women. These features do not affect the dose and method of administration of esomeprazole. In patients with mild to moderate hepatic impairment, the metabolism of esomeprazole may be impaired. In patients with severe hepatic impairment, the metabolic rate is reduced, resulting in a 2-fold increase in the AUC value for esomeprazole.
Pharmacokinetic studies have not been conducted in patients with renal failure. Since it is not esomeprazole itself that is excreted through the kidneys, but its metabolites, it can be assumed that the metabolism of esomeprazole in patients with renal failure does not change.
In children aged 12-18 years, after repeated administration of 20 mg and 40 mg of esomeprazole, the AUC and TCmax values in the blood plasma were similar to the AUC and TCmax values in adults.
Efficacy of esomeprazole in the treatment of gastroesophageal reflux disease
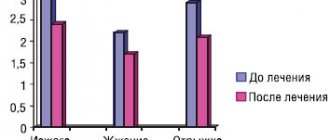
In general, the effectiveness of all proton pump inhibitors in the long-term treatment of gastroesophageal reflux disease is the same. However, esomeprazole (Nexium) has advantages in cases where greater acid suppression is required. Using the example of a patient with erosive reflux esophagitis grade C according to the Los Angeles classification, the effectiveness of esomeprazole is considered.
Rice. 1. Reflux esophagitis
Rice. 2. Segmental distal esophagospasm
Rice. 3. Small non-fixed axial cardiac hiatal hernia
Rice. 4. Normoacid pH values of the stomach (middle and lower graphs), acidic gastroesophageal reflux (top graph)
Rice. 5. After eight weeks of Nexium therapy, no inflammatory changes in the esophageal mucosa were observed
Rice. 6. Esophageal manometry after eight weeks of Nexium therapy
Gastroesophageal reflux disease (GERD) is a condition in which reflux of stomach contents causes distressing symptoms and/or complications [1]. GERD is characterized by a wide range of both esophageal (heartburn, regurgitation, chest pain) and extra-esophageal symptoms (bronchial asthma associated with reflux, cough, laryngitis, etc.). In a third of patients, the disease is complicated by reflux esophagitis, the long-term existence of which leads to the development of stricture, Barrett's esophagus, and adenocarcinoma of the esophagus [2]. According to the results of the MEGRE study, the prevalence of GERD in Moscow reaches 23.6%, in other cities of Russia – 13.3% [3].
The pathogenesis of GERD is based on gastroesophageal reflux. The main mechanisms of its formation include the ineffectiveness of the antireflux barrier (decrease in pressure and transient relaxation of the lower esophageal sphincter (LES)), increased intra-abdominal pressure, hiatal hernia (HH). The source of reflux is the “acid pocket” that forms after eating [4].
Drug treatment is aimed at eliminating and controlling the symptoms of GERD, treating and preventing its complications [5]. Antacids and alginates are considered emergency medications for heartburn [6, 7]. Proton pump inhibitors (PPIs) are recognized as the most effective drugs for controlling symptoms and treating reflux esophagitis [8]. They reduce the volume and increase the pH (reduce the aggressiveness) of the “acid pocket” by reducing gastric acid production [9, 10]. The advantage of PPIs over H2-receptor blockers and prokinetics in the control of heartburn has been proven (relative risk (RR) of heartburn when using prokinetics 0.86; 95% confidence interval (CI) 0.73–1.01; when using H2-receptor blockers RR 0 .77; 95% CI 0.60–0.99; when prescribing a PPI, RR 0.37; 95% CI 0.32–0.44) [11]. Four-week use of PPI ensures healing of reflux esophagitis in 90% of patients [12]. However, in 10–40% of patients with GERD, symptoms cannot be completely relieved or reduced with a standard dose of PPI [13].
The ineffectiveness of PPIs in patients with GERD is due to the influence of many factors. Among them are insufficient suppression of acid production, associated with the pharmacokinetics of the drug, and patients’ non-compliance with doctor’s recommendations (dose and time of taking PPIs) [14, 15].
According to our data, in 154 patients with GERD who received PPI in a standard daily dose, in 13.6% of cases the therapy was ineffective. The reasons for the persistence of heartburn in 4.5% of cases were individual characteristics of the pharmacokinetics of the drug, in 9.1% - non-reflux mechanisms of symptom formation against the background of mental maladjustment [16].
The effectiveness of PPIs for GERD is determined by their ability to eliminate the acid pocket. Consequently, with a larger volume, a more pronounced suppression of gastric secretion is required - an increase in the dose or frequency of PPI administration, or its replacement with a more effective drug.
Clinical case
Patient X., 32 years old, applied to the Moscow Clinical Scientific and Practical Center (MCSC) in February 2014 with complaints of severe heartburn after eating, worsening when bending the body forward and in a lying position, “burning-burning” sensations in the epigastric region through 10–15 minutes after eating. Periodically there was a sensation of a lump behind the sternum when swallowing.
Heartburn due to errors in diet had been bothering me since 2002, but the patient did not go to the doctor and took antacids and enzymes on her own. Over time, episodes of heartburn became more frequent. At the end of 2012, the severity of heartburn intensified, a “burning-burning” sensation appeared in the epigastric region after eating, and therefore the patient independently took PPIs for two to three weeks. During therapy, my health improved, but when the drugs were discontinued, after some time it worsened again (last PPI intake in November 2013). A significant deterioration in the condition was noted in January 2014 - heartburn became permanent. Then the “searing-burning” pain in the epigastrium resumed, and a sensation of a lump behind the sternum arose when swallowing food. The patient contacted the MCSC for examination and treatment.
From the anamnesis it is known that the patient grew and developed normally. There are no concomitant diseases. Works as an accountant and leads a sedentary lifestyle (work involves a computer). Smokes (half a pack or a pack a day) for 12 years. Denies the use of alcohol and drugs. There are no allergic reactions to medications.
On examination: normosthenic physique, moderate nutrition (body mass index 21.5 kg/m2). From the respiratory organs and cardiovascular system without pathology. The abdomen is of regular shape, symmetrical, painful on palpation in the epigastric region. The liver and spleen are not enlarged.
Results of esophagogastroduodenoscopy (EGDS): erosive reflux esophagitis grade C according to the Los Angeles classification (Fig. 1; in the lower third of the esophagus, the mucous membrane is swollen, hyperemic, irregularly shaped erosions are detected, spreading to two or more folds, covering less than 75% of the circumference of the esophagus , the bottom is covered with fibrin), chronic gastritis with the presence of erosions, duodenitis. To diagnose H elicobacter
pylori
during endoscopy, a rapid urease test was performed, as well as a blood test for immunoglobulin class G antibodies to
H. pylori
. Both methods gave negative results.
To determine the cause of dysphagia, esophageal manometry was performed. Segmental distal esophagospasm was diagnosed (Fig. 2; resting pressure of the LES 17.7 mm Hg (normal), residual pressure 4.6 mm Hg (normal), relaxation within normal limits. All contractions in the body of the esophagus are peristaltic with normal wave amplitude, in the distal body of the esophagus (3 cm from the level of the LES) contractions are long-lasting (15.2 s), multi-peak). X-ray examination of the upper gastrointestinal tract (GIT) with a contrast agent (Fig. 3) showed the presence of a small sliding hiatal hernia. There was no need for daily pH monitoring, since in the presence of reflux esophagitis there is no doubt about the diagnosis of GERD.
Based on clinical and instrumental data, a diagnosis was made: GERD in the stage of erosive reflux esophagitis, grade C according to the Los Angeles classification. HHH. Chronic gastritis with the presence of erosions, not associated with H. p ylori
, exacerbation.
For 20 days, the patient received omeprazole 20 mg twice a day 30 minutes before breakfast and dinner. During treatment, pain in the epigastric region was relieved, which contributed to a slight improvement in well-being. Heartburn and a feeling of a lump when swallowing persisted.
To establish the reasons for the ineffectiveness of therapy with omeprazole 40 mg/day, 24-hour pH measurements were performed (the esophageal sensor was installed 5 cm above the LES) (Fig. 4). Normoacid values of stomach pH were revealed (average value during the day 2.3), signs of acidic gastroesophageal reflux (DeMeester index 15.69 (normal
The patient was recommended a basic course of therapy lasting eight weeks. Heartburn did not bother me, the feeling of a lump behind the sternum when swallowing disappeared. During control endoscopy, after eight weeks of therapy, erosions in the esophagus were epithelialized, and endoscopic remission of GERD was achieved (Fig. 5).
During control manometry of the esophagus, positive dynamics were noted: no signs of segmental distal esophagospasm were detected, the picture corresponded to normal motility of the esophagus (all contractions in the body of the esophagus are peristaltic with normal amplitude and duration of waves) (Fig. 6).
Consequently, esophagospasm was secondary in nature against the background of inflammation. This was also evidenced by the disappearance of complaints about the sensation of a lump behind the sternum when swallowing during antisecretory therapy.
Maintenance treatment with Nexium 20 mg 30 minutes before breakfast is recommended for a long time; if heartburn occurs, increase the dose to 40 mg/day.
Discussion
Persistence of heartburn despite a standard dose of PPI is becoming an increasingly common problem in clinical practice. The reasons for the ineffectiveness of PPIs are usually divided into two groups:
- the patient has a confirmed diagnosis of GERD, but taking a PPI does not eliminate the symptoms;
- The patient does not have GERD, so PPIs do not have an application point.
In the first case, the symptoms are caused [14]:
- persistence of pathological acid reflux (due to decreased bioavailability and accelerated metabolism of PPIs, low patient compliance, incorrect prescription of PPIs in relation to food intake);
- increased sensitivity of the esophagus, due to which “normal” acid reflux causes symptoms (hypersensitivity esophagus);
- non-acid reflux (duodenogastric reflux, bile reflux).
- Other pathologies not associated with gastroesophageal reflux [17]:
- functional heartburn;
- motor disorders of the esophagus (achalasia, esophagospasm, scleroderma);
- eosinophilic, drug-induced, infectious esophagitis;
- diseases of neighboring organs (cholelithiasis, cancer, diseases of the cardiovascular system, neuromuscular diseases, etc.).
The detection of typical reflux esophagitis in patient X. during endoscopy left no doubt about the diagnosis of GERD. One of the most common reasons why heartburn persists due to GERD is an incorrect regimen of PPIs in relation to food intake. Most PPIs should be prescribed 30 minutes before breakfast, which allows for maximum drug concentrations in the blood plasma during the period of maximum stimulation of acid production by food [18]. Only 46% of patients adhere to this PPI regimen. 39% take the drug more than an hour before meals, 30% after meals, 28% before bed, 3% as needed, which reduces the effectiveness of treatment [19]. Patient X. received omeprazole 30 minutes before meals twice a day.
If symptoms persist due to insufficient acid suppression and persistence of acid reflux, the dose should be increased or the PPI replaced [20]. It has been shown that 80–90% of patients with GERD with reflux esophagitis grades A and B according to the Los Angeles classification respond to therapy with standard doses of PPI, and the same number of patients with grades C and D respond to double doses. Among patients with non-erosive reflux disease standard doses of PPI are effective in 50–60%; of the remaining 40%, about 60–70% respond to double doses of PPI. This leaves approximately 10% of patients who require either different treatment or a revision of the diagnosis [21].
One of the reasons for the persistence of symptoms during treatment is the peculiarities of PPI metabolism. In patients with accelerated metabolism, the concentration of the drug may not reach values sufficient to ensure an adequate antisecretory effect [22]. Esomeprazole (the S-isomer of omeprazole) is metabolized to a lesser extent by the liver cytochrome P450 system compared to the R-isomer of omeprazole, which reduces the variability of its clinical effects [23].
According to a multicenter study of 99 patients with GERD whose symptoms persisted despite taking a standard dose of PPI for eight weeks, when replacing the PPI with esomeprazole (Nexium) at a dose of 40 mg, there was a significant reduction in the incidence and severity of heartburn, regurgitation and epigastric pain [24].
Particular attention was paid to the diagnosis of H.
pylori
, the absence of which was confirmed by two methods.
The need for its diagnosis and treatment in patients who are planning long-term treatment with PPIs (usually with erosive reflux esophagitis) is due to the fact that long-term suppression of acid production in patients infected with H. pylori
, without eradication, contributes to the progression of atrophy of the gastric mucosa [25 ].
A meta-analysis of randomized clinical trials (ten studies, 15,316 patients) showed the superiority of esomeprazole over other PPIs in the healing of reflux esophagitis. After four weeks, its effectiveness was higher by 10% (RR 1.1; 95% CI 1.05–1.15), after eight weeks of therapy - by 5% (RR 1.05; 95% CI 1.02–1 ,08). The greatest advantage of esomeprazole was observed in patients with severe reflux esophagitis: the NNT indicator (number needed to treat, the number of patients who need to be treated to achieve one good result) was 50 for grade A according to the Los Angeles classification, 33 for grade B, 14 – for grade C, 8 – for grade D [26].
In 1391 patients with reflux esophagitis and heartburn, esomeprazole 20 mg/day was superior to lansoprazole 15 mg/day in maintaining clinical endoscopic remission for six months (83% (95% CI, 80–86% vs 74% (95) % CI, 70–78%), p
Conclusion
In long-term treatment of GERD, the effectiveness of all PPIs is similar [5]. At the same time, esomeprazole (Nexium) has advantages in situations requiring more pronounced suppression of acid production - when symptom control is ineffective when using a standard dose of other PPIs, as well as for achieving and maintaining endoscopic remission of the disease in patients with reflux esophagitis of degrees C and D according to Los Angeles classification.
Esomeprazole-Vial, 40 mg, enteric-coated tablets, 14 pcs.
Esomeprazole is the S-isomer of omeprazole and reduces gastric acid secretion by specifically inhibiting the proton pump in gastric parietal cells. The S- and R-isomers of omeprazole have similar pharmacodynamic activities. Mechanism of action.
Esomeprazole is a weak base that transforms into an active form in the highly acidic environment of the secretory tubules of the parietal cells of the gastric mucosa and inhibits the proton pump - the enzyme H + / K + - ATPase, thereby inhibiting both basal and stimulated secretion of hydrochloric acid.
Effect on the secretion of hydrochloric acid in the stomach.
After oral administration of 20 mg or 40 mg, the effect of esomeprazole develops within 1 hour. When taking the drug daily for 5 days at a dose of 20 mg once a day, the average maximum concentration of hydrochloric acid after stimulation with pentagastrin is reduced by 90% (when measuring the acid concentration 6-7 hours after taking the drug on the 5th day of therapy).
In patients with gastroesophageal reflux disease (GERD) and clinical symptoms, after 5 days of daily oral esomeprazole 20 mg or 40 mg, intragastric pH values above 4.0 were maintained for an average of 13 and 17 hours out of 24 hours. When taking esomeprazole at a dose of 20 mg per day, intragastric pH values above 4.0 were maintained for at least 8, 12 and 16 hours in 76%, 54% and 24% of patients, respectively.
A correlation was identified between the concentration of the drug in plasma and the inhibition of hydrochloric acid secretion (to assess the concentration, the AUC parameter was used - the area under the concentration-time curve). The therapeutic effect achieved as a result of inhibition of hydrochloric acid secretion.
When taking the drug at a dose of 40 mg, healing of reflux esophagitis occurs in approximately 78% of patients after 4 weeks of therapy and in 93% of patients after 8 weeks of therapy.
Treatment with esomeprazole 20 mg twice daily in combination with appropriate antibiotics for one week results in successful eradication of Helicobacter pylori in approximately 90% of patients. Patients with uncomplicated peptic ulcer disease after a week-long eradication course do not require subsequent monotherapy with drugs that reduce the secretion of gastric glands to treat the ulcer and eliminate symptoms. The effectiveness of esomeprazole in bleeding from peptic ulcers, confirmed endoscopically, has been shown.
Other effects associated with inhibition of hydrochloric acid secretion During treatment with drugs that reduce the secretion of gastric glands, the concentration of gastrin in the plasma increases as a result of a decrease in the secretion of hydrochloric acid. Due to decreased secretion of hydrochloric acid, the concentration of chromogranin A (CgA) increases. Increased concentrations of CgA may affect the results of examinations for the detection of neuroendocrine tumors. To prevent this effect, it is necessary to temporarily stop taking esomeprazole 5 days before the CgA concentration test.
In patients receiving esomeprazole for a long time, an increase in the number of enterochromaffin-like cells was observed, probably associated with an increase in plasma gastrin concentrations.
Patients taking drugs that reduce the secretion of gastric glands for a long period of time are more likely to develop glandular cysts in the stomach. These phenomena are caused by physiological changes as a result of pronounced inhibition of hydrochloric acid secretion. Cysts are benign and undergo reverse development.
The use of drugs that suppress the secretion of hydrochloric acid in the stomach, including proton pump inhibitors, is accompanied by an increase in the content of microbial flora in the stomach that is normally present in the gastrointestinal tract. The use of proton pump inhibitors may lead to a slight increase in the risk of infectious diseases of the gastrointestinal tract caused by bacteria of the genus Salmonella spp. and Campylibacter spp and possibly Clostridium difficile in hospitalized patients.
In two comparative studies with ranitidine, esomeprazole was superior in treating gastric ulcers in patients receiving nonsteroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors.