- home
- general surgery
- Gastroesophageal reflux disease
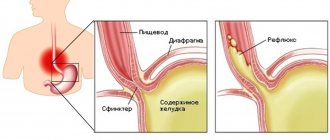
Gastroesophageal reflux disease (GERD) is a chronic disease of the digestive system in which, as a result of spontaneous or regularly repeated reflux of gastric or duodenal contents into the esophagus, an inflammatory process of the wall of its distal section develops. This disease is the most common among diseases of the digestive system; it is diagnosed in a third of the adult population.
The cause of reflux is most often the failure of the sphincter located at the border of the stomach and esophagus. Also, reverse reflux of contents can occur when the motor function of the upper part of the digestive tract is impaired. Unfavorable factors influencing the development of the disease are smoking, excess weight, diaphragmatic hernia, taking certain medications, and stress.
Symptoms of gastroesophageal reflux disease
The main symptom of the disease is persistent heartburn, its occurrence does not depend on food intake or physical activity. It can occur on an empty stomach or after eating, during active movements, especially when bending the body, and even in a lying position. Belching and regurgitation of food often occurs.
Pain may appear - bursting or burning, localized in the epigastrium, behind the sternum and even in the left hypochondrium; often the pain intensifies after eating or physical activity, and nausea and vomiting may occur. In advanced cases, difficulties with swallowing appear - dysphagia; The cause of this disorder may be impaired motility or narrowing of the lumen of the esophagus - stricture. Also, the symptoms of GERD can be supplemented by drooling during sleep, and hoarseness is possible after waking up.
Prokinetics
Prokinetics are only effective in treating mild forms of GERD. If GERD is more severe, in addition to prokinetics, drugs that inhibit the secretion of gastric juice are usually prescribed.
Of the prokinetic agents, metoclopramide (10 mg/day orally) is prescribed in European clinics - this is the most commonly prescribed regimen in adults with GERD. Long-term treatment with prokinetic drugs can be dangerous, with serious, even fatal, complications.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Complications
The result of aggressive contents entering the esophagus can be damage to the esophageal mucosa; due to regular exposure to an aggressive environment, an inflammatory process develops, which leads to the appearance of reflux esophagitis - inflammation of the lower parts of the esophagus. If left untreated, an ulcer may form - damage to the esophageal wall down to the submucosal layer. In severe cases there is a risk of bleeding. After the ulcer has healed, scars may remain that can cause stricture. The result of deterioration in the patency of the esophagus will be dysphagia in combination with heartburn, which only aggravates the situation.
One of the severe complications is Barrett's esophagus syndrome, in which the squamous cell epithelium in the esophagus is replaced by columnar gastric epithelium - metaplasia, and the likelihood of degeneration into cancer increases by 30-40 times.
Classification
Diseases of the esophagus
Among diseases of the esophagus, the most common are gastroesophageal reflux disease, tumors, and manifestations of pathology of other organs and systems.
Gastroesophageal reflux disease
Gastroesophageal reflux disease (GERD) is a failure of the motor and evacuation functions of the esophagus. With these disorders, there is a systematic reflux of food from the stomach into the esophageal canal. This causes damage to the mucous membrane of the lower esophagus. As a result, dystrophic changes develop in it, which provokes many complications. The reasons for the development of GERD are decreased tone of the lower sphincter of the esophageal tube, decreased peristalsis of the esophageal canal, and changes in the composition of gastric juice.
There are non-erosive and erosive forms. A complication of the erosive form is the so-called Barrett's esophagus.
Erosive form of GERD
occurs as a result of systematic damage to the esophageal mucosa. Gastric acids gradually corrode the membrane. Clinically manifested by heartburn, which worsens as a result of overeating, eating fatty, fried foods, and alcohol. A characteristic symptom is dysphagia.
This is difficulty swallowing food and liquids. Liquid food is difficult, but solid food does not cause difficulties. The occurrence of heartburn is also affected by body position: bending over, lying down after eating.
Barrett's esophagus
Barrett's esophagus is a pathological process during which the cells of the mucous membrane of the esophageal canal are replaced by intestinal-type epithelium. It occurs as a reaction to regular exposure to acids from the stomach contents during reflux. As a result, the risk of developing a cancerous tumor of the esophageal canal sharply increases. Symptoms are heartburn, belching, burning sensation and pain behind the sternum, dry cough, feeling of heart failure.
Neoplasms and tumors of the esophagus
Neoplasms are manifested symptomatically by vomiting and difficulty swallowing. Benign tumors are rare and are represented by leiomyoma, polyps, and diverticula.
Malignant tumors are more common. The clinical picture remains unclear only at the onset of the disease. In the future, progressive pain when swallowing, belching, and increased salivation are characteristic. Dysphagia manifests itself first as difficulty swallowing solid food, then liquid, until the complete cessation of food intake.
Stomach diseases
Stomach diseases often occur with mild symptoms. These include gastritis, peptic ulcers, and neoplasms. The leading role in the occurrence of gastritis, ulcers, and stomach cancer is played by the bacterium Helicobacter pylori. It contributes to the disruption of the protective properties of the gastric mucosa with the development of inflammation. As a result, it is destroyed by aggressive factors of gastric juice. Provoking factors include stress, poor diet (overeating, starvation), bad habits, consumption of foods with strong effects (coffee, strong tea, medications, alcohol, spicy and fatty foods).
Gastritis
Gastritis is an inflammatory process in the gastric mucosa. Often the acute form becomes chronic. Symptoms – pain in the upper abdomen, heartburn, nausea, flatulence, belching, bitterness in the mouth, stool disorders.
Peptic ulcer
Gastric ulcers are often caused by the bacteria Helicobacter pylori. Sometimes the appearance is associated with uncontrolled use of anti-inflammatory drugs. Symptoms: pain associated with eating. Pain syndrome can appear 30 minutes after eating, sometimes “hunger” pain appears.
The ulcer may be asymptomatic or with mild symptoms in the initial stages. The danger is that gastric ulcers without treatment and asymptomatic can cause severe complications - stomach cancer, ulcer bleeding, perforation of the ulcer, penetration and perforation of the ulcer. Such conditions often require emergency surgery due to the threat to the patient's life.
Due to the danger of developing severe situations that require urgent surgical intervention, patients with established ulcers are recommended to stay close to medical care points.
Neoplasms and tumors of the stomach
Gastric neoplasms are common; benign tumors account for no more than 4% of the diagnosis. They are mainly represented by polyps. As a rule, they are asymptomatic. Sometimes they manifest themselves as heartburn, aching pain after eating, dizziness and bowel disorders.
Malignant neoplasms are diagnosed more often. The main factors are chronic Helicobacter pylori infection and chronic peptic ulcer disease without treatment. In the early stages, it manifests itself as a decrease in appetite, perversion of taste - aversion to previously favorite foods, and weight loss. In later stages, vomiting of yesterday's food, severe pain, and bloody stools occur.
Diseases of the duodenum
Diseases of the duodenum are most often diagnosed in the form of duodenitis, duodenal ulcers.
Duodenitis
Duodenitis is an inflammatory process in the transitional part of the duodenum. Manifested by nausea, vomiting, weakness, cramps. The causes are Helicobacter pylori, the provoking factors are poor diet, bad habits (smoking, alcoholism).
Duodenal ulcer
Duodenal ulcer is a chronic disease that relapses with pronounced seasonality. An ulcer appears as a result of the activity of Helicobacter pylori infection and uncontrolled use of non-steroidal anti-inflammatory drugs. During the period of remission, the course of the disease is asymptomatic. Clinical manifestations become obvious during the period of exacerbation. These include “hunger pains,” which are relieved after eating. Symptoms of an ulcer will also include severe acute pain at night, belching, and heartburn. Complications of untreated duodenal ulcers include bleeding, perforation with peritonitis, and stenosis. Complications require urgent surgical intervention.
Diagnostics
- The main method for diagnosing gastroesophageal reflux disease is fibrogastroscopy, which allows assessing the condition of the mucosa, the degree of changes in the wall of the esophagus, in the stomach and duodenum. During the procedure, you can perform a biopsy - take particles of pathologically altered tissue for histological examination; Based on this analysis, treatment is planned.
- Another effective method is radiography, during which a stricture, diaphragmatic hernia, or esophageal ulcer can be detected.
- To determine the level of gastric secretion and the presence of reflux, daily pH measurements are performed.
Depending on the course of the disease, the patient may be prescribed other examination methods: esophageal manometry, ultrasound, ECG, and may need to consult an otolaryngologist.
For a free written consultation, in order to identify the hiatal hernia and determine the degree of damage to the esophagus, as well as choosing the correct surgical treatment tactics, you can send me a complete description of gastroscopy, x-ray of the esophagus and stomach with barium for the hiatus, preferably an ultrasound of the abdominal organs, age and main complaints must be indicated. In rare cases, if there is a discrepancy between complaints, X-ray data and FGS, it is necessary to perform daily pH measurements and manometry of the esophagus. Then I will be able to give a more accurate answer to your situation.
1.Structure of the esophagus
Esophagus
- a muscular tube connecting the throat (pharynx) to the stomach. The length of the esophagus is about 20 centimeters, and its inner surface is a pink mucous membrane. There is a part of the esophagus called the upper esophageal sphincter (UES). This is a group of muscles at the top of the esophagus that work during breathing, eating, belching and vomiting. A person can consciously control this muscle group. The upper esophageal sphincter muscle also holds food and secretions that may come from the windpipe.
The lower esophageal sphincter (LES) is a group of muscles at the lower end of the esophagus where it connects to the stomach. When the lower esophageal sphincter is closed, it prevents acid and stomach contents from moving back out of the stomach. The muscles of the LES are not subject to conscious control.
Diseases of the esophagus
, in fact, not so little. Some of them are quite serious, some do not require complex and long-term treatment. Depending on the severity of the disease, it may be treated by gastroenterologists or thoracic surgeons, who perform operations on the esophagus when necessary for treatment.
A must read! Help with treatment and hospitalization!
Treatment
The goal of treatment is to relieve the symptoms of GERD and prevent the development of complications. For this purpose, medications are prescribed to neutralize the contents of the stomach or reduce its acidity. When taking medications, the patient also needs to constantly follow a diet; in case of obesity, weight normalization is recommended.
However, drug therapy is effective as long as the patient takes the medication; symptoms usually return after the end of the course of treatment. It should also be taken into account that long-term use of drugs that affect the acidity of gastric juice increases the risk of malignancy; suppression of secretion prevents the digestion of food, which entails a number of other disorders.
If drug therapy is ineffective, patients are recommended to undergo surgery. The indication for surgical treatment of GERD is the presence of complications, hiatal hernia, the appearance of strictures, ulcers, Barrett's esophagus, etc., as well as the presence of extra-esophageal symptoms: hoarseness, chest pain.
The purpose of surgery for GERD is to create a mechanism that prevents the reflux of stomach contents into the esophagus. Most domestic surgeons perform Nissen fundoplication. During the intervention, the fundus of the stomach is wrapped around the esophagus 360 degrees; This creates a cuff that prevents reflux.
However, this technique has its drawbacks. For example, the formation of a valve in the cardia zone leads to the fact that regurgitation or vomiting - natural protective mechanisms - is lost. With large portions during meals or when drinking carbonated drinks, it becomes impossible to remove them through the cardia, the stomach swells, pain and a feeling of heaviness appear. Often, 1-2 years after Nissen surgery, a relapse occurs due to cuff slippage.
Pathophysiology
The content of the article
Under normal conditions (in a healthy person), the contents of the gastric juice with high acidity periodically enter the esophagus, but internal protective mechanisms either reduce the amount of acid secreted to a minimum or remove the acid, which is quickly removed by “cleansing” the esophagus. Therefore, symptoms of acid irritation of the esophagus are not felt or are minimal.
Mechanisms that protect the esophagus from stomach acid include the lower esophageal sphincter (sphincter) and normal esophageal motility (motility). When these mechanisms are disrupted, reflux occurs and symptoms of GERD occur.
Gastroesophageal reflux
Author's technique of modified fundoplication
During the operation, I use a Toupet partial fundoplication of 270 degrees, in which a cuff is created from the stomach wall to prevent the reflux of stomach contents into the esophagus. Thanks to the improved technique, for which a patent has been received, the functioning of the sphincter between the stomach and esophagus remains undisturbed, while the gag reflex and belching - protective functions - are also preserved.
The surgical intervention is performed using laparoscopy, using high-quality endoscopic equipment, which allows all manipulations to be performed with maximum precision, without the risk of damaging the structures located in this area: vessels, fascial spaces, vagus nerve. During laparoscopic surgery, I create a functional valve between the stomach and esophagus, which allows the patient to do without medications in the future. Due to the fact that all manipulations are performed through 3-4 small incisions, an excellent cosmetic result is guaranteed, since after healing, the marks from the incisions will become almost invisible.
When isolating the stomach and esophagus, I use the LigaSure device for dosed electrothermal tissue ligation, thanks to which the vessels can be “sealed” without damaging the surrounding tissues. The use of the latest generation of absorbable suture material and anti-adhesion barriers allows the operation to be performed quickly and efficiently.
If there are several diseases that require surgical treatment, in our clinic the patient can count on a simultaneous operation. Instead of several interventions, the interval between which should be 5-6 weeks, the person being operated on during one anesthesia can immediately get rid of a number of diseases.
Patients are discharged, as a rule, on days 1-3, and after 2-3 weeks they return to their usual activities. For the first two months you will have to adhere to a strict diet; over the next six months, the diet will gradually expand. In the future, a person who has undergone treatment in our clinic will be able to do without medications and without following a strict diet. We managed to reduce the number of relapses during the first year to 2%; five years after the operation, this figure does not exceed 4%.
I have performed more than 2000 operations on the stomach and esophagus, the accumulated experience is summarized in three monographs and more than 50 scientific publications, which can be found in professional peer-reviewed publications published in our country and abroad.
Clinical picture
There are physiological narrowings in the esophagus, where malignant growth primarily begins. These narrowings are caused by passing near other anatomical formations - the aorta and the forks of the trachea into the bronchi; at the junction of the pharynx into the esophagus and the esophagus into the stomach there is also a slight narrowing. It is believed that the mucous membrane here is more susceptible to minor injuries from rough food, which means inflammation occurs more often. However, in the cervical region the incidence of cancer is 10%, in the lower third of the esophagus - 30%, and 60% of cancers are formed in the middle segment.
Malignant cells not only grow into the thickness of the organ, as happens with most cancers, they also migrate through small lymphatic vessels. The vessels form a complete lymphatic network inside the esophageal wall, spreading the tumor inside, so the length of the tumor can be 5, 10, or 15 centimeters.
In the advanced stage, localization determines the symptoms, and the first signs are considered to be the feeling of food sticking to the same place or scratching the mucous membrane with a piece of food. As it progresses, it becomes difficult to pass first solid pieces, then porridge, then liquid. All this is called dysphagia. First, the patient washes down pieces of food with water, pushing them through, but after that this no longer helps, nutrition is disrupted, and the person loses weight. Contact of the tumor with food leads to inflammation, an unpleasant putrefactive odor appears, and with regular trauma, the loose mucous membrane of the tumor begins to bleed, and life-threatening bleeding can develop.
Pain occurs as the esophagus contracts with peristaltic waves, the pain is spastic in nature. The growth of the tumor through the entire thickness of the esophageal wall makes the pain constant; it is localized between the shoulder blades. Infiltration of the mediastinal tissue by the tumor involves the recurrent nerve, which is responsible for the movement of the vocal cords, in the process, hoarseness and choking when drinking appear. The nerve can be compressed by lymph nodes enlarged by metastases and the sonority of the voice will disappear.
As with achalasia, a tumor forms an expansion above the narrowing of the esophagus, where food accumulates. Nighttime reflux of accumulated food masses into the windpipe can also lead to pneumonia. And during the day I am worried about severe weakness and fever. If the respiratory tract is involved in the process, an anastomosis may form between the esophagus and the trachea or large bronchi - a fistula, through which food crumbs will enter the breathing tube, causing coughing and pneumonia. If such a fistula opens from the esophagus into the mediastinum, its inflammation will lead to death.
Get a treatment program