Make an appointment by phone: +7 (343) 355-56-57
+7
- About the disease
- Cost of services
- Sign up
- About the disease
- Prices
- Sign up
Barrett's syndrome is a pathological change in the mucous membranes of the esophagus that can lead to the development of cancer. The problem is associated with constant exposure of the epithelium to hydrochloric acid and damage to the walls of the organ during gastroesophageal reflux. Requires comprehensive diagnosis and treatment under the supervision of a gastroenterologist.
Main causes of the disease
Barrett's esophagus is a common complication of gastroesophageal reflux disease (GERD).
According to doctors, heartburn increases the risk of the syndrome by up to 80%. The pathology most often develops in men aged 45 to 65 years, and if left untreated, leads to the formation of adenocarcinoma. The main reason is the regular reflux of gastric juice into the proximal esophagus. Acids destroy the thin epithelial layer and stimulate the growth of metaplastic cells. Under favorable conditions, the risk of their malignancy and cancer development significantly increases within 2-4 years.
The disease develops over a long period of time. Main risk factors:
- esophageal sphincter insufficiency;
- reflux disease;
- weakening of contractile function;
- increased production of gastric juice;
- smoking.
Increases the likelihood of Barrett's esophagus - poor diet, frequent alcohol consumption, excess weight. Sometimes the pathology develops against the background of constant use of drugs for the treatment of pancreatitis, enzymatic drugs based on natural bile.
Rehabilitation
Already from the first day, the operated patient gets out of bed, and the next day is allowed to take liquid food. Discharge from the clinic is possible after 1-3 days; a person begins work, as a rule, after 2-3 weeks. Following a strict diet is necessary for two months, then you can switch to a softer one, which should be followed for at least six months.
After RFA, the patient is under medical supervision for several months, during which time he is prescribed gastroscopy. If after surgery for a hernia (HH) the examination shows a decrease in the affected area of the mucous membrane, then the patient continues to be observed and is recommended to undergo FGS every six months. You can get a conclusion about the presence or absence of Barrett's esophagus after a year. If metaplasia is still present, RFA is indicated. In the future, the patient is under the supervision of a doctor, undergoing regular examinations.
Stages and forms of pathological changes
The rate at which the disease progresses depends on the underlying cause. Regardless of the risk factors, cell degeneration occurs in stages:
1.
Metaplasia - healthy epithelium of the esophagus is replaced by cells that are structurally identical to the cells of the mucous membranes of the stomach or intestines. This is a natural reaction of the body that protects the walls of the esophagus from damage by an acidic and alkaline environment. If metaplasia reaches 3−4 cm, the risk of adenocarcinoma increases 2−3 times. The presence of goblet cells, called intestinal metaplasia, is necessary to confirm the diagnosis of Barrett's esophagus.
2.
Dysplasia is already a prestage of gastric adenocarcinoma. There are different degrees of severity of precancerous dysplastic changes: mild and severe dysplasia.
It is possible to develop an erosive form of the disease - inflamed areas and open wounds form in the lower part of the esophagus, near the sphincter. Ulcers can bleed, cause severe pain behind the sternum, and are injured by the passage of solid food.
Argon plasma coagulation
Argon plasma coagulation (APC) is considered the most effective method for treating BE without foci of severe dysplasia [38]. The device for carrying out this type of ablation consists of a source of argon gas, a source of high-frequency electric current and a special catheter that supplies gas and current directly to the pathologically altered tissue [30]. The principle is based on the fact that when leaving the catheter, the gas is ionized by the electrode and provides a high-frequency current to the metaplastic epithelium of the esophagus [30, 38]. The depth of coagulation is usually 1–3 mm, but the depth of damage depends on the power of the generator (30–90 W), the flow rate of argon gas (1–2 l/min), and the distance from the catheter to the tissue (2–5 mm) and the time of exposure to the tissue itself [39]. Due to the ability to adjust the shape, size and energy of the plasma arc, APC provides ablation of even small areas of metaplastic epithelium in the esophagus without significant damaging effects on surrounding tissues [26]. Sequential APC with overlapping fields can also be used for fairly extended segments of metaplasia [38, 39]. In the work of S.S. Pirogov showed that in case of BE with a segment length of 3–4 cm, APC is effective in 80–90% of patients [39]. Complications (odynophagia, stenosis, perforation) after APC occur statistically significantly less frequently than with PDT [40, 41]. The results of long-term prospective observations of patients who underwent PCA have shown that the effectiveness of this method is higher when applying a higher voltage electric current or when combining PCA with high doses of PPIs [38–41]. A comparative analysis of prospective clinical studies monitoring patients with BE without dysplasia lesions who were treated with PCA is presented in Table 2.
Symptoms and signs of Barrett's esophagus
The first manifestations of pathological metaplasia go unnoticed due to the symptoms of gastroesophageal reflux disease. Often, altered cells are detected only when examining the epithelium. To avoid dangerous complications, you should contact a gastroenterologist if you have the following symptoms of Barrett's esophagus:
- painful sensations when swallowing a bolus of food (dysphagia);
- belching after eating;
- unpleasant sore throat, which intensifies when bending over;
- hoarse voice;
- the appearance of a dry, unproductive cough;
- chest pain;
- increased sensitivity of tooth enamel.
In advanced conditions and metaplastic changes in the epithelium, non-healing erosions occur on the wall of the esophagus. Characteristic signs are internal bleeding, chronic anemia, significant weight loss.
Pathogenesis
Barrett's disease develops as a result of the process of metaplasia of cells located at the bottom of the esophagus in front of the stomach under the influence of chronic acid damage and esophagitis , causing inflammation and erosive-ulcerative changes. Metaplasia of the esophagus comes down to the replacement of squamous epithelium with columnar epithelium, characteristic of the stomach, as a structure more capable of withstanding the effects of gastric acid. In this case, as a result of reparation, goblet and other columnar cells characteristic of metaplastic transformation are found.
Metaplasia due to GERD
In the future, the pathology can lead to mild or severe dysplasia in the form of enlargement of nuclei, changes in the nuclear and cytoplasmic ratio, increased mitotic activity, cytological and nuclear polymorphism. This occurs under the influence of hydrochloric acid, which increases the activity of enzymes - protein kinases , which initiate mutagenic and proliferative processes in cells while simultaneously inhibiting apoptosis in the area of the affected epithelium.
Diagnostic features
Comprehensive diagnostics using modern techniques helps determine the cause and select the correct treatment for Barrett’s esophagus.
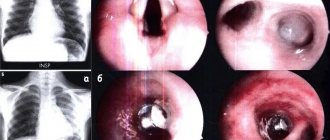
Esophagogastroscopy is the most informative method for early detection of metaplastic changes on the wall of the organ. During the procedure, the doctor takes biomaterial for histology and performs chromoscopy of the patient’s abdomen and stomach. Clinical recommendations indicate the following methods of examining a patient:
- X-ray of the stomach and esophagus;
- manometry;
- intraesophageal pH-metry.
If there is a change in the epithelium and anemia, a stool test for occult blood must be performed. In patients with hereditary risk factors, it is recommended to study markers of esophageal dysplasia.
Treatment methods for Barrett's syndrome
For mild damage to the mucous membranes of the esophagus, therapy is aimed at restoring healthy epithelium and reducing the risk of cell degeneration.
Clinical recommendations at this stage of treatment: taking drugs that normalize acidity and improve the movement of food to the stomach (prokinetics and proton pump inhibitors). When dysplasia grows, it is necessary to crop the affected area. The main methods used in gastroenterology:
- ablation of the esophagus with a bipolar electrode;
- cryodestruction;
- laser therapy;
- resection of damaged mucous membranes.
In difficult situations, a Nissen operation is performed: a special membrane is formed that prevents the reflux of gastric juice into the esophagus. If erosions or tumors form, part of the organ must be removed.
Operation
If metaplasia, as well as mild and moderate dysplasia is detected, we are talking about a benign process, in which case organ-preserving surgery is possible. If severe dysplasia or squamous cell carcinoma, a malignant disease, is diagnosed, Lewis surgery is performed. If areas of high-grade neoplasia with a likelihood of invasion are found in the area of metaplasia, then RFA can be performed. In case of deep damage, radical removal of a section of the esophageal mucosa using an endoscopic method is indicated.
Our clinic performs laparoscopy using the unique technique of Professor Puchkov. During the operation, a hiatal hernia is repaired, a physiological valve is created between the esophagus and the stomach, and pathological reflux is eliminated. Recovery occurs in a short time; already six months after the operation there is no need to take medications, there is no need to adhere to any strict diets, and for the rest of your life. The number of relapses has been reduced to 2%. Thanks to the use of modern materials during surgery, after healing there are no scars on the skin of the abdomen, only 3-4 incisions 5-10 mm long, which become invisible over time. By the way, in the clinic it is possible to simultaneously perform operations on the abdominal and pelvic organs during one anesthesia. In one operation, the clinic’s specialists can relieve patients from several pathologies at once.
Prevention of Barrett's esophagus: clinical recommendations
Advice from gastroenterologists helps to avoid complications and the development of the disease:
- early diagnosis and treatment of GERD;
- giving up cigarettes and alcohol;
- proper nutrition, eating fresh vegetables and fruits, reducing fatty and fried foods in the diet.
It is important to completely change your lifestyle and eating habits: do not overeat, reduce the amount of spices, sweets, carbohydrate foods, and reduce weight if you are obese. If dysplasia is detected, visit a doctor at least 2 times a year.
Barrett's esophagus is a chronic disease that can lead to dangerous consequences. Modern diagnostic and treatment methods make it possible to prevent serious complications and return the patient to the opportunity to lead an active lifestyle with minimal restrictions.
Complications
The main complication of Barrett's esophagus is malignant transformation into adenocarcinoma secondary to dysplasia.
On average, severe dysplasia is diagnosed in 20-25% of patients within 20-23 years after diagnosis. The likelihood of its development correlates with the length of the affected area and the degree of dysplasia:
- With low-grade dysplasia, the risks of malignancy are 0.8-1.9% per year.
- For severe dysplasia - 6-12.2% per year.
In addition, the number of foci of dysplasia is important. With multiple lesions, the likelihood of malignancy is three times higher than with single lesions.