Lymphadenopathy is a condition that is characterized by an increase in the size of peripheral lymph nodes, a change in their consistency and mobility. It develops along with an increase in overall body temperature, an enlargement of the spleen and liver. Even a slight enlargement of the lymph nodes indicates that pathological processes are developing in the body that require adequate treatment. It can cover one or more structures and cause inflammatory processes.
The hematology department of CELT invites you to undergo diagnosis and treatment of lymphadenopathy in Moscow. You have the opportunity to consult with leading domestic hematologists, who have modern techniques and a powerful base that allows you to quickly and accurately establish a diagnosis. They provide treatment in accordance with international standards. You can find out the cost of services in the “Services and Prices” section. To avoid misunderstandings, do not forget to check the numbers during consultation or with our operators.
Lymphadenopathy: what is it?
Enlarged lymph nodes look like soft or dense rounded formations located under the lower jaw, in the cervical, axillary, groin or other areas. They can have a smooth or bumpy surface and very often develop after acute infections and inflammations. Sometimes their appearance is caused by traumatic injuries to the skin or the introduction of a vaccine.
Lymphadenopathy develops due to the accumulation of a certain type of cell in the lymphadenoid tissue. The reaction is often provoked by increased blood flow, an increase in the number of lymphocytes and macrophages in response to the appearance of foreign genes in the body. In just one week, the node can increase five to fifteen times. A pathological condition is spoken of if, along with an excess of size, there is a change in the density, mobility and surface of the structure. When palpated, it can be quite painful or painless.
Reasons for contacting our center for diagnosing lymphadenopathy in Moscow: independent identification of large nodes that do not hurt, a feeling of intense pain during palpation, other symptoms in the form of a rash, increased body temperature, weight loss, and rapid fatigue. Particularly dangerous can be nodes that do not go away for more than two months, located in different areas, with a diameter of more than two centimeters, the enlargement of which occurred for no apparent reason.
Lymphadenopathy: classification and causes
The classification of lymphadenopathy is based on a number of parameters, starting with the location of the affected structures and ending with their pain and size:
| Localization of the affected node/nodes | Etiological factors |
| Under the lower jaw | Diseases of the eyes, ear, throat, nose, damage to the skin in the head or neck area, dental problems. |
| Neck |
|
| Supraclavicular region | Malignant neoplasms:
|
| Armpits |
|
| Groin |
|
Lymphadenopathy: from syndrome to diagnosis
The increase in the size of lymph nodes is based on various pathological processes, which determines the clinical interdisciplinarity of LDP syndrome. In this regard, doctors of various specialties (internists, infectious disease specialists, oncologists, hematologists, morphologists, etc.) can become real participants in the diagnostic process for a patient with the presence of LDP. At the same time, the successful solution of the differential diagnostic problem largely depends on the constructive interaction of many specialists and their awareness of diseases manifested by an increase in lymph nodes. The main problem of differential diagnosis in LDP lies primarily in the similarity of the clinical picture of tumor and non-tumor LDP. Lymphadenitis and reactive lymph node hyperplasia are an important component of the LDP syndrome. According to a study at the Hematological Research Center of the Ministry of Health and Social Development of Russia, non-tumor LDPs account for 30% of the reasons for initial visits to a hematologist for enlarged lymph nodes. Nosological diagnosis is established only in 50% of cases in patients with non-tumor LDP.
Diseases and pathological processes accompanied by LDP
The main pathological processes that cause lymph node enlargement are infections, tumor lesions (primary or metastatic), immunoproliferative and dysmetabolic processes (Fig. 1).
LDP of infectious origin can be caused by direct infectious lesion of lymph nodes with the introduction of an infectious agent by hematogenous or lymphogenous route into the tissue of lymph nodes (tuberculosis, actinomycosis, purulent lymphadenitis, viral infections) or reactive inflammation in response to an infectious focus in the corresponding area (axillary lymphadenitis with felon, inguinal lymphadenitis with erysipelas of the lower limb or genital infection, submandibular lymphadenitis with oropharyngeal infection, etc.). A clear distinction between these 2 forms is to a certain extent arbitrary and is associated with the level of diagnostic examination (morphological, immunological, use of PCR, etc.). With the same infection, LDP can be both infectious and reactive in nature (primary tuberculous affect, tuberculosis of lymph nodes).
Tumor damage to lymph nodes can be primary (lymphoproliferative tumors) or secondary - in leukemia or cancer (metastatic process). Tumor LDPs account for about 70% of all patient visits to specialized departments due to lymph node enlargement.
Immunoproliferative LDPs. This term is not generally accepted and can be used in cases where the increase in lymph nodes is not associated with either infection or a tumor process. In this case, proliferation of immunocompetent cells or granulomatous inflammation occurs in the lymph nodes due to various disorders in the system of cellular, humoral and nonspecific immunity.
Dysmetabolic LDP is caused by the proliferation of phagocytic mononuclear cells in the lymph nodes or the deposition of amyloid in corresponding diseases.
Diagnostic search in patients with LDP
The direction of the diagnostic search for LDP is determined primarily by the clinical situation, i.e., information obtained during the initial examination of the patient (history, physical examination), data from routine laboratory tests - mainly peripheral blood parameters. In the differential diagnosis of LDP, the main guidelines are:
- age of patients;
- anamnestic information;
- the nature of the LDP (localization, prevalence, size, consistency, pain, mobility of lymph nodes);
- the presence of other clinical signs (enlarged spleen, fever, skin rashes, articular syndrome, lung damage, etc.);
- peripheral blood parameters.
Each of the above signs has a different and ambiguous diagnostic value. Thus, fever or anemia in a patient with LDP can be a manifestation not only of an infectious and tumor process, but also of some systemic vasculitis (systemic lupus erythematosus (SLE), Still's disease, etc.). At the same time, the detection of blast cells in the peripheral blood almost unambiguously indicates the presence of acute leukemia in the patient and requires only clarification of its morphological variant. A diagnostic search for LDP can conditionally include several stages, at each of which specific tasks are solved to achieve the ultimate goal - nosological diagnosis in a patient with the presence of LDP syndrome.
Stage I of the diagnostic search. Revealing
enlarged lymph node and its differences
from non-lymphoid formations
At this stage of the diagnostic search during the initial examination of the patient, the skills and abilities to identify enlarged lymph nodes should be developed. In this case, it is important to be able to distinguish an enlarged lymph node from non-lymphoid formations of various locations. Such non-lymphoid formations, which present difficulties in differential diagnosis, include neck cysts, fibromas, lipomas, accessory lobules of the mammary gland, thyroid nodules, hidradenitis, enlargement of the parotid salivary glands and more rarely encountered non-lymphoid nodular formations (Weber-Christian panniculitis, etc.) . Non-lymphoid space-occupying formations in the cervical and axillary areas occur in almost 5% of cases among patients referred to specialized institutions due to “enlarged lymph nodes.”
Stage II of the diagnostic search.
Localization and prevalence of LDP
After verifying the identified formation of an enlarged lymph node, it is necessary to determine the different localization and assess the prevalence of the lymph node. This may be important in determining the direction of further diagnostic search.
Localization of enlarged lymph nodes allows one to suspect a range of diseases for the purpose of further targeted research. Thus, posterior cervical lymph nodes are usually enlarged with scalp infections, toxoplasmosis, and rubella, while enlarged anterior (parotid) lymph nodes suggest infection of the eyelids and conjunctiva. Often detected local enlargement of cervical lymph nodes is a consequence of infections of the upper respiratory tract, nasopharynx, infectious mononucleosis, but it is also necessary to exclude both lymphoproliferative tumors (lymphogranulomatosis) and metastases in lymph nodes of tumors of various locations (head and neck, lungs, mammary and thyroid glands ). At the same time, an increase in supraclavicular and prescalene lymph nodes is almost never reactive, but is more often associated with lymphoproliferative tumors (lymphogranulomatosis), metastatic tumor process (tumors of the stomach, ovaries, lungs, mammary glands).
Depending on the prevalence, the following variants of LDP should be distinguished:
- local - enlargement of one lymph node in one of the areas (single cervical, supraclavicular lymph nodes);
- regional - enlargement of several lymph nodes in one or two adjacent areas (supraclavicular and axillary, supraclavicular and cervical, occipital and submandibular lymph nodes, etc.);
- generalized - enlargement of lymph nodes in three or more areas (cervical, supraclavicular, axillary, inguinal, etc.).
Despite the relativity of this division, the prevalence of LDP may be important when putting forward a preliminary diagnostic hypothesis after the initial examination of the patient.
The anatomical position of the lymph nodes in localized LDP allows in many cases to narrow the differential diagnostic search. So, for example, cat scratch disease is characterized by damage to the cervical and axillary lymph nodes, and in cases of sexually transmitted infections - to the inguinal lymph nodes. Enlargement of one lymph node often requires exclusion of a primary or metastatic tumor process; may be a reactive response to a local infectious-inflammatory process in the corresponding area (reactive inguinal lymphadenitis in genital infections, enlargement of submandibular lymph nodes in acute tonsillitis, etc.). Regional LDP with a predominant increase in the occipital and posterior cervical lymph nodes is more typical for infectious mononucleosis. Generalized LDP is detected in various diseases: infectious (viral infections, toxoplasmosis), systemic (SLE), lymphoproliferative tumors (chronic lymphocytic leukemia).
Along with the prevalence of LDP, it is necessary to evaluate the size and consistency of the lymph nodes. This is not a defining feature, but can serve as a justification for putting forward a preliminary diagnostic hypothesis (suspicion of a tumor process in the presence of a dense lymph node larger than 1 cm in size, pain during inflammation, fluctuation during abscess formation, etc.).
Stage III of the diagnostic search.
Identification of additional signs in patients with LDP
When determining the direction of the diagnostic search, it is important that the patient has additional clinical signs identified during the initial examination (anamnestic, clinical) and routine laboratory and instrumental studies (chest x-ray, general blood test).
The age of patients can be one of the guidelines that determines the direction of the diagnostic search, since a number of diseases manifested by LDP have a certain “age affinity”. It is known that infectious mononucleosis is more common in childhood and adolescence, and chronic lymphocytic leukemia is more common in elderly and elderly people. Of course, the patient’s age cannot be of decisive importance when making a diagnosis; it only serves as one of the guidelines.
Anamnestic information (extremity trauma, surgical interventions, the presence of an implant, travel, contact with certain patients, etc.) allows you to determine the direction of the diagnostic search, and in some cases can become decisive in the differential diagnosis of LDP (the presence of a disease in the patient, manifested by an increase in DR, taking certain medications).
Clinical signs. A thorough clinical examination of a patient with LDP is necessary in order to identify various additional symptoms, among which the most diagnostically important are:
- lesions of the skin and mucous membranes (maculous-papular rashes, hemorrhages, scratches, bites, ulcers, etc.);
- liver enlargement;
- splenomegaly;
- articular syndrome;
- fever;
- respiratory symptoms;
- changes from ENT organs;
- urogenital symptoms.
The detection of an enlarged spleen in a patient with LDP is more typical for viral infections (infectious mononucleosis), acute and chronic lymphocytic leukemia, systemic diseases (SLE, Still's disease in adults). Articular syndrome is more often associated with systemic diseases (rheumatoid arthritis, SLE, Still's disease). The presence of skin rashes first of all requires the exclusion of viral infections, SLE, and Still's disease.
Stage IV of the diagnostic search.
Peripheral blood examination
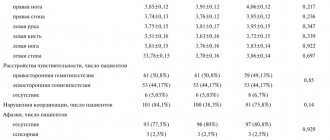
Among the routine laboratory methods of differential diagnosis in patients with LDP, the study of peripheral blood parameters is mandatory. When interpreting the detected changes in peripheral blood, it is necessary to take into account their unequal specificity. Thus, persistent absolute lymphocytosis with the presence of Gumprecht cells is a pathognomonic laboratory sign of chronic lymphocytic leukemia, and the presence of blast cells in the blood may indicate either lymphoblastic leukemia or leukemia of lymphomas. Signs such as neutrophilic leukocytosis, leukopenia (neutropenia), thrombocytopenia are not specific, since they can occur in a wider range of diseases accompanied by LDP (Table 1).
Along with a general analysis of peripheral blood, during the initial treatment of a patient with LDP, the mandatory tests are: chest x-ray, ultrasound of the abdominal organs, immunoserological studies (syphilis, HIV infection, hepatitis B and C). Figures 2 and 3 present diagnostic search algorithms for local (regional) and generalized LDP.
The difficulties of differential diagnosis in local or regional LDP lie primarily in the ability to identify a local inflammatory process of an infectious (more often) or non-infectious nature and to associate the identified local pathology with an increase in lymph nodes in the corresponding area. The most common local inflammatory processes, accompanied by an increase in regional lymph nodes, the identification of which must be focused on, are the following:
- acute tonsillitis (tonsillopharyngitis);
- stomatitis;
- otitis media;
- eczema of the face, limbs;
- conjunctivitis;
- acute thrombophlebitis of the extremities;
- erysipelas (face, limbs);
- boils, carbuncles;
- panaritiums;
- scratches, bites;
- inflammatory process of the external genitalia.
When a local inflammatory process is detected in patients with an increase in regional lymph nodes, the situation is regarded as reactive lymphadenitis. Methods of cytological and histological diagnosis in the acute phase of the disease are not very informative due to the difficulties of interpreting the morphological picture against the background of reactive hyperplasia of lymphoid tissue. For final verification of the nature of LDP, it is necessary to assess the dynamics of local inflammation and regional LDP against the background of ongoing therapy (antibiotics, surgical treatment) or spontaneous reverse development. In cases of persistent lymph node enlargement, despite the regression of the local inflammatory process, especially in the presence of dense lymph nodes, a lymph node biopsy for histological examination is indicated. Figure 4 shows the diagnostic value of additional clinical signs identified during the initial examination in patients with LDP.
Additional examination methods should be used taking into account the preliminary diagnostic hypothesis put forward on the basis of the nature of the LDP and the presence of additional signs (anamnestic, clinical, laboratory). Prescribing antibiotics to patients with LDP is indicated only in cases of proven bacterial infection. The use of glucocorticoids for unclear LDP is inappropriate.
Literature
- Williamson MAJ Lymphadenopathy in family practice: A discriptives study of 240 cases // J. Fam. Pract. 1985. Vol. 20. R. 449.
- Dvoretsky L.I. Differential diagnosis for lymphadenopathy. Handbook of a practicing physician. 2005. T. 3. No. 2. P. 3–12.
- Vorobiev A.I. (ed). Guide to Hematology. M., 1990. T. 1. P. 423–426.
- Henry P., Longo D. Enlarged lymph nodes and spleen. In the book: Internal medicine according to Tinsley R. Harrison. M.: Praktika, 2002. pp. 410–417.
- Pangalis GA et al. Clinical approuch to lymphadtnopathy // Semin. Oncol. 1993. Vol. 20. R. 57.
- Cohen J. Infectious mononucleosis and other infections caused by the Epstein-Bar virus. In the book: Internal medicine according to Tinsley R. Harrison. M.: Praktika, 2002. T. 1. P. 1330–1338.
- Melikyan A.L. Algorithm for diagnosing non-tumor lymphadenopathy // Clinical Oncohematology. 2009. No. 4. pp. 306–316.
- Ferrer R. Lymphadenopathy: differential diagnosis and evaluation // Am Fam Physician. 1998 Oct 15. Vol. 58(6). R. 1313–1320.
Lymphadenopathy: diagnosis
Before starting treatment of lymphadenopathy in adults, CELT hematologists conduct comprehensive studies to accurately diagnose and determine the cause of the development of the pathological condition. The following node parameters must be taken into account:
- Dimensions - determine the degree of the disease (first - 5 mm-14 mm, second - 15 mm-24 mm, third - 25 mm or more);
- Painful symptoms - most often it occurs during inflammatory processes, in particular purulent lymphadenitis;
- Quantity – one, two or several nodes located in one area can be affected. Multiple lesions are a sign of an active pathological process;
- Density - usually inflamed nodes are soft, their fluctuation is a sign of a purulent process, tight plasticity - lymphoma, hardness - metastases;
- Connectivity - several nodes combined into one whole can be a sign of tuberculosis, Besnier-Böck-Schaumann disease, or damage to lymphatic tissue.
In addition to the examination, the patient is prescribed diagnostic tests:
- Detailed blood test;
- Test for hepatitis and HIV;
- Ultrasound scanning of internal organs and affected nodes;
- Histology of biopsy samples from the affected node;
- X-ray examination;
- Magnetic resonance or computed tomography.
Features of the pathology
Considering that there are more than 600 lymph nodes in the human body, we can assume the development of pathology in any organ and system of the body, both in an adult and a child. Most often, in the practice of a hematologist at a medical center, it is necessary to diagnose lymphatic lesions in places such as:
- abdomen;
- mediastinum;
- groin;
- submandibular zone;
- neck;
- armpits.
The presence of pathology of the lymph nodes in any of these areas of the body indicates an existing underlying disease. And, unfortunately, often it can be oncology. According to statistics, in 1% of cases in patients diagnosed with lymphadenopathy, additional examination reveals malignant formations.
Lymphadenopathy: treatment
The development of treatment tactics is carried out by CELT specialists based on the diagnostic results obtained and the patient’s individual indicators. First of all, efforts are directed toward eliminating the pathological condition that has become the initiating factor for the development of lymphadenopathy. If purulent lesions of the lymphatic structures or bacterial infections are detected, the patient is prescribed antibacterial therapy. If indicated, surgical removal of the node is possible.
If the etiological factors involve damage by viral agents, the patient is prescribed antiviral and immunomodulatory pharmacological drugs. If he suffers from pain - painkillers. Most often, lymphadenopathy goes away within one to one and a half months after the cause that caused it is eliminated. Otherwise, the hematologist prescribes a biopsy and develops a new treatment strategy.
The hematology department of our clinic receives candidates, doctors and professors of medical sciences. Their practical and scientific work experience ranges from twenty-five years. You can make an appointment with them online or by contacting our information line operators. If necessary, you can make an appointment with specialists at any of our departments and undergo the necessary procedures. In particular, septoplasty is available in the otolaryngology department, which can improve the patient’s quality of life.
At CELT you can consult a hematologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
By making an appointment with a hematologist, you can get a comprehensive consultation. The doctor is competent to treat various blood diseases, most of which can be identified in the early stages and prescribe timely treatment to cope with the disease quickly and easily.