Pharmacological properties of the drug Omaron
Pharmacodynamics. A combined drug that has a pronounced antihypoxic, nootropic and vasodilating effect. Piracetam activates metabolic processes in the brain by enhancing energy and protein metabolism, increasing the utilization of glucose by cells and their resistance to hypoxia, improves the processes of interneuronal transmission in the central nervous system, and regional blood flow in the ischemic area. Cinnarizine is a selective blocker of slow calcium channels, prevents the entry of calcium ions into cells and reduces their content in the plasma membrane depot, reduces the tone of smooth muscles of arterioles, reduces their response to biogenic vasoconstrictors (epinephrine, norepinephrine, dopamine, angiotensin, vasopressin). It has a vasodilating effect (especially of cerebral vessels, enhancing the antihypoxic effect of piracetam), without significantly affecting blood pressure. It exhibits moderate antihistamine activity, reduces the excitability of the vestibular apparatus, and reduces the tone of the sympathetic nervous system. Increases the elasticity of red blood cell membranes, their ability to deform, and reduces blood viscosity. Pharmacokinetics. Piracetam: quickly and completely absorbed into the gastrointestinal tract. The maximum concentration of piracetam in the blood plasma is achieved after 2–6 hours. The maximum concentration in the cerebrospinal fluid is achieved after 2–8 hours. Bioavailability is 100%. Does not bind to blood plasma proteins. Penetrates into all organs and tissues, passes through the placental barrier. Selectively accumulates in the cerebral cortex, mainly in the frontal, parietal and occipital lobes, cerebellum and basal ganglia. Not metabolized. After 30 hours, more than 95% is excreted by the kidneys. Cinnarizine: the maximum concentration of cinnarizine in the blood plasma is determined after 1–4 hours. It is 91% bound to plasma proteins. Actively and completely metabolized. The half-life is 4 hours. 1/3 m of metabolites are excreted in the urine, 2/3 in feces.
Acute cerebrovascular accidents are one of the most common pathological conditions in clinical practice. According to the World Federation of Neurological Societies, at least 15 million strokes are registered annually in the world. At the same time, there is reason to believe that these data are clearly underestimated, since in developing countries many cases of stroke are not registered or are completely ignored by doctors due to the inaccessibility of medical care. In Russia, the incidence of stroke is 3.4 per 1000 people per year. In absolute terms, this amounts to more than 450,000 new strokes per year [6]. The consequences of a stroke place a heavy burden on society, significantly reducing the level of family, social and work adaptation of patients.
The rapid increase in the incidence of acute cerebrovascular accidents and their “rejuvenation” form one of the most pressing problems of modern medicine - the problem of rehabilitation. As a rule, with a favorable course of ischemic stroke, the acute onset of neurological symptoms is followed by its stabilization and gradual regression. It is assumed that the reduction in the severity of neurological symptoms is based on the process of “retraining” of neurons, as a result of which intact parts of the brain take over the functions of the affected ones. At the cellular level, this process is caused by the formation of new dendrites and synapses between neurons and changes in the electrophysiological properties of neuronal membranes. There is evidence [1, 2] that active motor, speech and cognitive rehabilitation during the recovery period of ischemic stroke has a beneficial effect on the process of “retraining” of neurons and improves the outcome of ischemic stroke. It is generally accepted that rehabilitation measures should begin as early as possible and be systematically carried out during the first 6-12 months after an ischemic stroke. During these periods, the rate of restoration of lost functions is maximum.
When carrying out treatment and rehabilitation measures, it should be taken into account that the majority of patients, as a rule, have concomitant somatic pathology. This could be atrial fibrillation, atherosclerosis, dyslipidemia, hypertension, diabetes mellitus, etc. The presence of concomitant pathology involves the combined use of up to 5-10 or more drugs with different mechanisms of action, which ultimately leads to the problem of polypharmacy and associated negative phenomena (potentiated side effects, the risk of developing drug-induced damage to the kidneys, liver, etc.) . Difficulty also arises for the doctor in selecting an adequate dosage regimen for each drug, and for the patient in complying with it, which leads to deterioration of compliance or even refusal of treatment.
The result of numerous attempts to optimize the pharmacotherapy of neurological diseases has been the creation of combination drugs containing 2 or more components with different mechanisms of action, which have different effects on the pathogenesis and clinical manifestations of specific forms of pathology. Particularly popular are combination drugs that help normalize central regulatory mechanisms, improve cerebral metabolism and hemodynamics, stabilize cortical-subcortical interactions, containing active ingredients of both nootropic and vasotropic effects. Obviously, combining several active ingredients into one tablet makes taking medications easier and more convenient. But the benefits of combination drugs are far from limited to this. In modern pharmacology, the phenomenon of synergistic action of 2 or more different active substances is actively used. The positive effects that are observed when the components of combined drugs are simultaneously introduced into the body can be of fundamental importance for enhancing their therapeutic effect and improving patient tolerance.
A good example of this synergy is the combination of piracetam and cinnarizine, which is currently widely used for the treatment of vascular pathology of the brain [4]. The first of them acts on many neurochemical processes. The effect of piracetam on the vascular system is no less significant: the drug affects the degree of platelet adhesion to the surface of the epithelium of the vascular wall, reduces platelet aggregation and, thus, improves regional blood flow in the ischemic area. Cinnarizine, a selective blocker of calcium channels in cerebral vessels, improves cerebral circulation and has a clinically significant effect on microcirculation. By inhibiting the entry of calcium ions into vascular smooth muscle cells, it reduces the tone of arterioles, reduces their sensitivity to vasoconstrictor substances (epinephrine, norepinephrine, dopamine, angiotensin, vasopressin) and prevents pathological vasoconstriction. At the same time, cinnarizine is characterized by high affinity specifically for cerebral vessels, increases total and regional cerebral blood flow, exerting a selective effect on spasmodic vessels, without causing the “steal” syndrome, which ensures the implementation of a protective anti-ischemic effect. An important advantage of cinnarizine should be considered its ability to reduce the excitability of the vestibular apparatus, which expands the indications for its use in vestibular dysfunctions.
Currently, the domestic drug Omaron, containing 0.4 g of piracetam and 0.025 g of cinnarizine in one tablet, is widely used as a combination drug containing piracetam and cinnarizine. The activating effect of piracetam, reducing the sedative effect of cinnarizine, allows lobster to have a normothimic effect, ensuring good tolerability of the drug with long-term use. In turn, the sedative properties of cinnarizine optimally neutralize the phenomena of increased activation of the central nervous system and the associated symptoms of agitation and sleep disturbances, which are observed in some cases during therapy with single-drug piracetam [3]. Omarone improves brain metabolism due to its neuroprotective effect and optimization of cerebral blood flow [5].
The purpose of this study was to study the effectiveness and safety of the use of the drug Omaron in the early recovery period of ischemic stroke for the correction of cognitive, motor and speech disorders in patients.
Material and methods
The study was conducted on the basis of the rehabilitation treatment department of Voronezh city clinic No. 7.
It included 120 patients undergoing rehabilitation after an ischemic stroke. Of these, 50 (41.7%) people suffered a heart attack in the territory of the right middle cerebral artery, 54 (45%) in the left middle cerebral artery, and 16 (13.3%) in the vertebrobasilar territory. The time elapsed since the stroke ranged from 28 to 262 days, averaging 118.5±4.6 days; Patients prevailed (57.5%) who suffered an acute cerebrovascular accident 90-180 days before the study. The previous cerebral infarction was verified using CT or MRI of the brain in 77 (64.2%) subjects.
The criteria for excluding patients from the study were recurrent stroke; the presence of severe motor, speech, cognitive deficits, as well as decompensation of somatic diseases.
The clinical condition of the patients was assessed based on the results of a study of the neurological status and data from additional research methods.
Omaron was prescribed 1-2 tablets 3 times a day for 1-3 months, depending on the severity of the disease, for children - 1-2 tablets 1-2 times a day.
To assess the effectiveness of the therapy, the following methods were used: 1) assessment of the severity of neurological symptoms in points; 2) a brief scale for assessing higher mental functions - MMSE (Mini-Mental State Examination); 3) assessment of the patient’s activity in everyday life (according to the Barthel index); 4) clinical global impression scale - CGI; 5) assessment of the tolerability and effectiveness of the drug (0-5 points).
Patients were examined before the start of therapy (1st visit), after 2 weeks of treatment with lobster (2nd visit) and after completion of the treatment course (3rd visit).
Results and discussion
During a neurological examination, the majority of patients revealed coordination (84.17%), sensory (95.8%) and motor (75.8%) disorders in the form of moderate right-sided hemiparesis - in 43 (35.8%) patients, left-sided hemiparesis in 42 (35%). Speech disorders were less common: elements of motor aphasia - in 19 patients, sensory aphasia - in 3, mixed aphasia - in 5 people.
Cognitive changes were noted in 69 (68%) patients with an average MMSE score of 23.6±0.5. The Barthel index averaged 72.7±1.6 points, which corresponds to the patient’s moderate dependence on others. In general, the severity of stroke in patients included in the study, with a score ranging from 0 (no changes) to 7 (very severe deficit), was assessed as a moderate deficit - 4.05 ± 0.06 points.
When assessing the neurological status of 120 patients at the end of treatment with omaron, a gradual regression of motor, sensory disorders and coordination disorders was noted, but the severity of the changes was not statistically significant (Table 1).
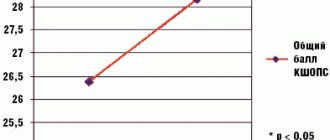
A statistically significant improvement was observed when assessing mental functions on the MMSE scale ( p
<0.001);
the severity of stroke significantly decreased by the end of the study ( p
<0.001) and the activity of patients in the sphere of daily life increased - Barthel index (
p
<0.05) in all groups of patients (see Table 1).
A significant effect of lobster on sleep indicators was revealed - in almost all patients the process of falling asleep improved. At the same time, lobster reliably ( p
<0.001) reduced the severity of somatovegetative manifestations - headache, dizziness (Table 2).
A reliable complex effect of lobster on autonomic dysfunction, asthenic syndrome, memory loss, anxiety and low mood was revealed.
By the time the study was completed, a therapeutic effect of varying severity was observed in all patients, including a very good therapeutic effect in 11 (9.13%), good in 80 (66.7%) and satisfactory in 29 (24.17). %) of patients.
Thus, an analysis of literature data [1] and our own clinical experience allows us to state that omarone, as a combination drug, can increase the effectiveness and expand the scope of use of its ingredients - piracetam and cinnarizine, while simultaneously ensuring the safety of their use.
The advantages of using lobster in clinical practice are expressed in the possibility of using proven standard effective combinations of active substances within one dosage form (simplification of the procedure for choosing a medicinal product for a practitioner); reducing forced polypharmacy while maintaining or increasing the effectiveness of treatment; improving compliance (ease of use for the patient and the doctor); increasing the economic accessibility of treatment.
If we take into account the low income of patients, which requires a reasonable selection of drugs that ensure effectiveness and compliance with treatment standards, then it can be noted that the domestic drug Omaron meets these requirements and can be recommended for the rehabilitation of stroke patients at the outpatient stage of their treatment.
Indications for use of the drug Omaron
Insufficiency of cerebral circulation (atherosclerosis of cerebral vessels, the recovery period of ischemic and hemorrhagic stroke, traumatic brain injury, encephalopathy of various origins, intoxication; other diseases of the central nervous system, accompanied by a decrease in intellectual and mnestic functions (impaired memory, attention, mood), psychoorganic syndrome with a predominance signs of asthenia and adynamia, asthenic syndrome; labyrinthopathy, Meniere's syndrome; mental retardation in children; prevention of migraine and kinetosis.
Efficacy of Omaron in patients with dyscirculatory encephalopathy
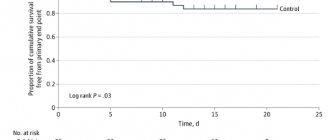
The clinical diversity of DE is conventionally reduced to emotional-volitional, mnestic, pyramidal, brainstem-cerebellar, parkinsonian and other syndromes [Schmidt E.V., 1985, Burtsev E.M. 1998, Yakhno N.N., 2000]. The leading role in the formation of cognitive impairment in DE is played by the separation of the frontal lobes and subcortical formations, which leads to secondary dysfunction of the frontal lobes of the brain. According to the theory of A.R. Luria, the frontal lobes are responsible for the regulation of voluntary activity: the formation of motivation, choosing the goal of the activity, building a program and monitoring its achievement [5]. At the same time, the dorsolateral frontal lobe of the cortex and its connections with the striatal complex provide switching of attention, which is necessary for changing the activity algorithm. The orbitofrontal regions are involved in the suppression of goal-irrelevant impulses, thus ensuring stability of attention and the adequacy of behavioral reactions. In addition, the orbitofrontal frontal cortex is in close relationship with the hippocampus, ensuring stability of attention in mnestic activity [7,9]. Therefore, treatment of DE should be aimed at the underlying vascular disease (etiotropic therapy), the main pathogenetic mechanisms and clinical symptoms, which lead to a deterioration in the quality of life of patients and their immediate relatives. From a pathogenetic point of view, the prescription of drugs that improve cerebral microcirculation, but do not cause a “stealing” effect, is justified. For this purpose, drugs of various pharmacological groups such as phosphodiesterase inhibitors (Ginkgo biloba extract, pentoxifylline), calcium channel blockers (cinnarizine, nimodipine), presynaptic α-adrenergic receptor antagonists (nicergoline, piribedil) are widely used in everyday clinical practice. To ensure neurometabolic protection of neurons, drugs are used that increase the survival of neurons under conditions of chronic hypoxia. The most common and well-studied drug that improves memory, attention, mental activity, and also increases the brain’s resistance to hypoxia, is piracetam, which is already well known to a wide range of clinicians. However, in recent years, interest in piracetam has grown due to the emergence of combination drugs, for example Omaron, one tablet of which contains piracetam (0.4 g) and cinnarizine (0.025 g). This combination allows you to add the properties of cinnarizine, which has an effect on the blood vessels of the brain, to the properties of the “ideal” nootropic. Omaron is a combination drug with a pronounced antihypoxic, nootropic and vasodilating effect [6]. Piracetam reduces tissue oxygen demand and increases the body's resistance under hypoxic conditions, which makes its use in patients with stages I and II DE pathogenetically justified. Cinnarizine is a selective blocker of slow calcium channels, inhibits the entry of calcium ions into cells and reduces their content in the plasma membrane depot, reduces the tone of the smooth muscles of arterioles, reduces their response to biogenic vasoconstrictors (epinephrine, norepinephrine, dopamine, angiotensin, vasopressin). It has a vasodilating effect (especially in relation to cerebral vessels, enhancing the antihypoxic effect of piracetam), without having a significant effect on blood pressure. It exhibits moderate antihistamine activity, reduces the excitability of the vestibular apparatus, and lowers the tone of the sympathetic nervous system. Increases the elasticity of red blood cell membranes, their ability to deform, and reduces blood viscosity. Both components of Omaron enhance each other's effects, while simultaneously reducing the number of side effects. In this regard, a clinical study was conducted on the use of Omaron in patients with DE. The purpose of the study was to evaluate the effectiveness and tolerability of the drug Omaron in patients with DE. Materials and methods The open study included 203 patients aged 40 to 75 years (average age 61.7 years) of both sexes with a documented diagnosis of stage II DE. All patients signed informed consent to participate in the study with the opportunity to be observed for 45 days. The diagnosis of DE was established in accordance with generally accepted criteria [4] and was manifested by cognitive impairment, usually reaching a moderate degree. Syndromic diagnosis of moderate cognitive impairment was carried out in accordance with the diagnostic criteria of Touchon J., Petersen R. 2004 [8]: cognitive impairment according to the patient or relatives; neuropsychological confirmation of cognitive impairment; worsening cognitive abilities compared to the recent past; no significant disturbances in daily activities; absence of dementia. Exclusion criteria from the study: parkinsonian syndrome, the patient’s inability to complete the proposed tests, depression level greater than 17 points on the Beck scale, age over 75 years. All patients included in the study were divided into study and control groups using simple randomization. There were no statistically significant differences between the groups in gender, age and the presence of background pathology. Patients in both groups received somatoprotective drugs (hypotensives, vasodilators, etc.), which did not have a nootropic or sedative effect and did not have direct synergism with Omaron. Therapy with Omaron, 2 capsules 3 times a day. for 45 days was carried out in 117 patients, 86 patients formed the control group. Both groups were divided into subgroups: 55 years and younger, the second - over 55 years. During the study, all patients were examined twice by a neurologist and an ophthalmologist - on the 1st day of the disease and on the 45th day. At each examination, patients underwent a complete clinical neurological examination, neuropsychological testing, neuro-ophthalmological examination (visual acuity, fundus examination, measurement of visual fields using standard methods), average daily blood pressure and pulse were measured, drug tolerability and side effects were assessed, and plasma cholesterol levels were examined. . Testing assessed sleep quality, personal and situational anxiety. The study included assessment of subjective complaints of patients, assessment of neurological status, measurement of blood pressure and pulse in order to determine whether Omaron affects the main hemodynamic parameters and the results of neuropsychological testing. A formalized assessment of the severity of subjective symptoms was carried out using 5-point rating scales with standardized criteria for assessing the severity of each subjective symptom (from 0 - no violations to 4 - gross violations, similar to subjective manifestations). The following subjective symptoms were assessed: headache, dizziness, noise in the head, memory and sleep disturbances, fatigue, general weakness, difficulty walking, decreased vision, speech impairment, urinary incontinence, feelings of internal tension, irritability, fears, numbness in the extremities. The neuropsychological examination included: Mini-mental scale examination (MMSE); to assess short-term visual memory, patients were presented with 16 pictures with an exposure of 30–60 s (the number of remembered pictures was recorded); To study short-term auditory memory, 10 words were used (the number of remembered words was recorded after one repetition) [3]. To study the level of attention, black and white Schulte tables were used (the time during which the patient found numbers from 1 to 25 in squares was recorded). In Bourdon's proofreading test, the time it took to complete the first and second half of the table was recorded, the productivity of attention was the number of characters viewed in 5 minutes, the accuracy of execution was the number of correctly and incorrectly crossed out numbers in 5 minutes). The last two research methods make it possible to analyze not only the level of attention, but also exhaustion during work. To subjectively assess the quality of life, we used the first section (General Health (GH) - general health status) of the quality of life questionnaire "SF-36 HEALTH STATUS SURVEY" - the patient's assessment of his current health status and treatment prospects (a high score indicates a better quality of life ) [10]. To subjectively characterize the quality of night sleep by the patient, a 5-point assessment of the following sleep indicators was used: speed of falling asleep, duration and depth of sleep, well-being after waking up, where 1 point is bad and 5 points is excellent. All indicators were summed into an overall sleep score. The level of personal and reactive anxiety was assessed using the Spielberger scale [3]. The doctor and the patient independently made a general assessment of the effect and side effects of the treatment, using the Clinical Global Impression'Scale (CGI), namely the subscale of the effectiveness index, which is calculated based on the totality of one of four degrees of therapeutic effect (noticeable, moderate, minimal, no change) and the severity of the side effect of the drug (absent, insignificant, significant, leveling the therapeutic effect). During the ophthalmological examination, visual acuity, the condition of the retinal vessels, and the values of the visual fields in both eyes of the patients were recorded. The sum of all meridians is normally 535 degrees, which we took as 100%. The study was carried out on the Förster perimeter, white mark 2 mm. When the visual field is limited, recorded along individual meridians, the sum of all meridians decreases, which was recorded by an ophthalmologist. For statistical analysis, mean values and standard deviation were calculated. Comparisons were made using the parametric Student's t-test and the non-parametric Mann-Whitney U-test; the Wilcoxon test was used to assess the effectiveness of treatment. Differences were considered significant at p<0.05. Statistical processing of the material was carried out using the computer program Statistica 6.0. Results of the study The main reasons for the development of DE in the 203 patients examined were hypertension - in 185 (91.1%) people, heart rhythm disturbances - in 51 (25.1%), diabetes mellitus - in 43 (22.6%), hypercholesterolemia – 25 (12.3%). Transient ischemic attacks occurred in 11 (5.4%) patients. The examined patients had the following complaints: headache in 64 (31.5%) people, dizziness in 46 (22.6%), memory impairment in 50 (24.6%), noise in the head - 85 (41.8%). %), sleep disturbance – in 144 (70.9)%, increased fatigue – in 164 (80.8%), general weakness – in 91 (44.8%), difficulty walking – in 34 (16.7%), decreased vision - in 103 (50.7%), speech impairment - in 6 (3%), urinary incontinence - in 1 (0.5%), feeling of internal tension - in 28 (13.8%), irritability - in 10 ( 4.9%), fears – in 4 (2%), numbness and weakness in the upper and lower extremities in 24 (11.8%). A neurological examination revealed symptoms such as mild pyramidal insufficiency in the form of increased tendon reflexes or anisoreflexia in 105 (51.7%), reflexes of oral automatism in 34 (16.7%), slight ataxia in the limbs in 45 (22.1%) , cerebroasthenic manifestations - 78 (38.4%), dysarthria in 11 (5.4%), dysphonia - 9 (4.4%), scattered microfocal neurological symptoms in 53 (26.1%). In both the main and control groups, no significant changes in the neurological status were observed after the course of treatment. When analyzing the results of the Mini-Mental State Examination (MMSE), the score ranged from 16 to 30 points, the average score was 25; on the 45th day there was no significant difference in both groups. The dynamics of subjective complaints of patients are noted in Figure 1. When statistically processing the data, differences were obtained between the main and control groups on the 45th day of the examination (Figure 1): improvements in the main group compared to the control were registered in the following signs: headache (p< 0.01), dizziness (p<0.01), memory impairment (p<0.05), decreased vision (p<0.01), numbness and weakness in the upper and lower extremities (p<0.05). On the first day of the study, the number of correctly named pictures was inversely proportional to the patient's age. In the main group, the volume of visual memory after a 45-day course of treatment increased statistically significantly (p<0.01) in both age subgroups (younger, older) of patients from 10.3 (pictures) to 12.0 and from 8.1 to 9 .8, respectively, and also compared with the control group, which showed an improvement in visual memory only from 9.1 to 10.4 and from 8.7 to 9.1. The state of verbal memory functions in patients before the start of the study corresponded to the lower limits of normal for all assessed parameters. While taking the drug in the main group, clear positive changes were observed in almost all assessed indicators. There were no statistically significant differences between age subgroups. By the 45th day of taking Omaron, there was an increase in the volume of long-term memory in the main group and a lack of dynamics in patients in the control group. The increase in voluntary auditory memory as a result of treatment is presented in Figure 2. The study of indicators of voluntary attention revealed a significant improvement in the main group: indicators such as the volume of voluntary attention, functions of concentration, distribution and switching improved. Optimization of attention functions was expressed in a decrease in the time spent viewing tables, and the overall indicator of work efficiency also increased. Improvement in voluntary attention indicators in the main group was expressed in a decrease in the time required to find numbers according to Schulte tables (Fig. 3). The average time for processing all squares did not change in the control group and significantly decreased in the main group: statistically significant differences (p = 0.01) were obtained for the first, second tables and the average time of all tables. The effect of “workability” in the form of a decrease in the time spent working with the fifth square is present in the main group. Those. in the main group there is an increase in mental tempo and speed of orienting-search movements of the gaze when performing a task. It should be noted that a statistically significant improvement was achieved in the main group only due to patients in the older age subgroup; no changes were observed in the young subgroup, because the time indicators in it corresponded to the age norm of 48 and 50 s. An analysis of the level of mental performance during therapy with Omaron showed that while patients were taking it, the volume of processed information increased and, at the same time, the quality of mental activity improved in the form of a decrease in the number of errors. The dynamics of mental performance and accuracy of task completion were assessed in the Bourdon proofreading test (Table 1). It was noted that patients receiving Omaron, after treatment, showed incomparably better results in terms of speed and accuracy of the test. Statistically significant results in the main group compared to the control were obtained for the total time to complete the task (p<0.01) and the first half of the task (p<0.01), the number of characters viewed (p<0.05) and characters crossed out correctly ( p<0.05), the number of errors decreased statistically insignificantly. Errors were more often made by patients under 55 years of age. When presented with the first section (General Health (GH) - general health status) of the quality of life questionnaire "SF-36 HEALTH STATUS SURVEY", patients of all ages and groups gave a good assessment of their health and did not note a deterioration in it over time. The figures for all estimates ranged from 3.4 to 3.7. The effectiveness of treatment was assessed by the doctor and the patient, independently of each other, on a global clinical impression scale (maximum score - 3). Patients receiving Omaron gave the following ratings: those under 55 years old - 2.5, the older group rated the treatment at 1.6 points. At the same time, more objective changes in cognitive functions occurred in the older group of patients. Doctors gave scores of 2.4 and 2.2, respectively, to the younger and older subgroups. The dynamics of patients' anxiety are presented in Table 2. Personal anxiety did not undergo significant changes in both groups: for people under 55 years of age, the anxiety value was moderate: 43.1–45.3; in patients of the older age group, personal anxiety was higher: 47.6– 50.1. The initial survey revealed a high level of reactive anxiety in the older subgroups, and in the main group, as a result of treatment, it significantly decreased to moderate (p <0.01); in the control group it even increased slightly. There were no statistically significant changes in younger age groups. Taking into account the results of processing the data obtained during a survey of patients about a significant improvement in vision when taking Omaron, we made an attempt to objectify these changes in the visual analyzer. A standard method of visual field studies was also carried out in 203 patients (406 eyes). During the initial examination in the main group, the results were obtained (in% of the norm): a change from 79 to 97% in the younger age subgroup and from 45 to 90% in the older. The absolute increase in visual fields after 45 days of taking Omaron ranged from 0 to 11% in the younger age subgroup and from 0 to 28% in the older subgroup. Visual fields in the control group did not change after 45 days. The improvement in visual fields in the group of patients over 55 years of age who took Omaron turned out to be statistically significant (p <0.01) - the increase in visual fields was an average of 10.3% (Fig. 4). All patients included in the study received a full course of treatment. Side phenomena when taking Omaron were noted by one patient in the form of a headache, upon recruitment she revealed rise to blood pressure, and headaches have disappeared during its normalization. Conclusions in this way, the use of an omaron - a combined drug with a pronounced antihipoxic, nootropic and vasodilating effect in the daily dose of 6 tablets is safe and effective for the correction of cognitive disorders in DE. The main effects of the use of Omaron are expressed in a reliable improvement compared to the control group in terms of the severity of headaches, dizziness, memory disorders, reduction of vision, numbness and weakness in the upper and lower extremities. By the 45th day of the admission of Omaron, an increase in the volume of long -term memory in the main group and the lack of dynamics in patients of the control group were noted. Assessment of indicators of arbitrary attention revealed their reliable improvement in the main group: such indicators as volumes of arbitrary attention, the function of concentration, distribution and switching have improved. An analysis of the level of mental performance during the treatment of Omaron showed that in patients, in the background of its intake, the volume of processed information increased and in parallel the quality of mental activity in the form of a decrease in the number of errors. A statistically reliable increase in vision fields in patients with DE older than 55 years with initial disorders has been proved. Thus, the use of Omaron allows you to improve the condition of patients with DE, reducing the severity of the main symptoms of the disease, as well as improving the basic intellectual and modest indicators. Treatment is well tolerated by patients, does not cause serious side effects.
Literature 1. Damulin I.V. Alzheimer's disease and vascular dementia / Ed. N.N. Yakhno. M., 2002. 85 p. 2. Damulin I.V., Parfenov V.A., Skoromets A.A., Yakhno N.N. Circulatory disorders in the brain and spinal cord // Diseases of the nervous system. Guide for doctors / Ed. N.N. Yakhno, D.R. Shtulman. M., 2003. pp. 231–302. 3. Belova A.N. Scales and questionnaires in neurology and neurosurgery. M., 2004. 4. Zakharov V.V. Clinic, diagnosis and treatment of dyscirculatory encephalopathy // Russian Medical Journal. 2009. T. 17. No. 2. P. 140–144 5. Luria A.R. Higher cortical functions of humans. M.: Moscow State University Publishing House, 1969. 6. Parfenov V.A., Belanina G.R., Vakhnina N.V. and others. The use of Omaron in patients with moderate post-stroke cognitive impairment // Journal of Neurology and Psychiatry named after. S.S. Korsakov. 2009. No. 6. pp. 47–51. 7. Piliponich A.A., Zakharov V.V., Damulin I.V. Frontal dysfunction in vascular dementia // Clinical gerontology. 2001. T. 5. No. 6. P. 35–41. 8. Petersen RS, Touchon J. Consensus on mild cognitive impairment. Research and practice in Alzheimer's disease. // EADS–ADCS jont meeting. 2005. No. 10. P. 24–32 9. Roman GV Vascular dementia: NINDS AIREN diagnostic criteria // New concepts in vascular dementia / A. Culebras, J. Matias Guiu, G. Roman (eds). Barcelona: Prous Science Publishers, 1993. P.19. 10. Ware JE, Snow KK, Kosinski M. Et al. SF–36 Health Survey. Manuel and Interpretation Guide. Lincoln, RI: Quality Metric Inc. 2000. 150 rub.
Special instructions for the use of the drug Omaron
Should be used with caution in persons with liver and/or kidney disease. For mild to moderate renal failure (especially with creatinine clearance ≤60 ml/min), the therapeutic dose should be reduced or the interval between doses should be increased. In persons with impaired liver function, it is necessary to monitor the level of liver enzymes. You should avoid drinking alcohol during treatment. The drug is prescribed with caution for increased intraocular pressure, as well as Parkinson's disease. During treatment, caution should be exercised when driving vehicles and operating machinery.
Omaron
Omarone (piracetam + cinnarizine) is a combined nootropic drug. It is used for circulatory disorders in cerebral vessels (in the presence of atherosclerotic plaques in their lumen, during the rehabilitation period after an ischemic or hemorrhagic cerebral hemorrhage, TBI), diseases of the central nervous system, the manifestations of which are depression of cognitive functions, organic defects with asthenic and adynamic manifestations, diseases Meniere, delayed intellectual development in childhood, in order to prevent motion sickness syndrome and migraines. Piracetam stimulates metabolic processes in brain cells by intensifying protein metabolism and energy metabolism, increasing the ability of cells to absorb glucose and tolerate a lack of oxygen. Piracetam also promotes more productive transmission of nerve impulses to the central nervous system and improves regional blood circulation in ischemic areas. Cinnarizine – selectively blocks L-type calcium channels (the so-called “slow calcium channels”), prevents the entry of calcium ions into cells and their accumulation in the plasmalemma, causes relaxation of the smooth muscle “cocoon” of small arteries, reduces their sensitivity to the effects of endogenous vasosuppressors. It exhibits vasodilating properties (mainly in relation to cerebral vessels, potentiating the antihypoxic effect of its “partner” - piracetam), without causing a significant decrease in blood pressure. Acts as a histamine antagonist, desensitizes the vestibular apparatus, and reduces sympathetic tone. Makes erythrocyte membranes more elastic and resistant to deformation, improves the rheological characteristics of blood. Piracetam is quickly and almost completely absorbed from the gastrointestinal tract.
Bioavailability (an indicator reflecting the ability of a drug to be absorbed in the body) approaches 100%. Accumulates in the cerebral cortex. It does not undergo metabolic transformations, unlike cinnarizine, which is metabolized in full. Piracetam is excreted mainly in the urine, cinnarizine in the feces. Omarone is contraindicated in persons with hypersensitivity to piracetam, cinnarizine or auxiliary components of the drug, severe liver and kidney damage, Parkinson's disease, pregnant and lactating women. In pediatrics, the drug is used starting from the age of 5. Single dose for children and adults – 1-2 tablets. Frequency of application: three times a day (adults), 1-2 times a day (children). The duration of the medication course is 30-90 days. Possible unwanted side effects: dyspepsia, headache, sleep disorders, allergic reactions (in rare cases). When using Omaron with drugs that suppress the activity of the central nervous system, alcohol, and antihypertensive drugs, the sedative effect may be potentiated. Vasodilators potentiate the effect of Omaron. In persons with liver and kidney diseases, the drug should be used with extreme caution. It is recommended to abstain from alcohol during treatment. With a long course of medication (2.5-3 months), the main functional indicators of the liver and kidneys should be monitored. During the medication course, it is recommended to refrain from activities that require increased attention and concentration (including driving a car and working with potentially dangerous mechanisms).