Athlete's foot is a group of fungal diseases that have a common localization and similar clinical manifestations. They are very common and affect people of any age (rarely children), prone to a chronic relapsing course.
Infection occurs in bathhouses, showers, on beaches, gyms, when using someone else's shoes and other household items contaminated with fungal elements.
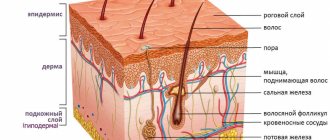
In the pathogenesis of the disease, the anatomical and physiological characteristics of the skin of the feet, increased sweating, changes in sweat chemistry, metabolic and endocrine abnormalities, injuries of the lower extremities, and vegetative dystonia are of significant importance. Pathogens can remain in a saprophytic state for a long time without causing active clinical manifestations. Athlete's foot has several clinical forms, each of which can be combined with nail damage.
Pathophysiology
Signals for pain and itching caused by skin causes are transmitted along the same pathways, but the afferent C-fibers differ functionally: one part of the nerve fibers is stimulated by histamine, the other by other substances that cause itching (for example, serotonin). There is evidence of similarities between neuropathic pain, itch and cough. Their common property is peripheral and central sensitization of the afferent nervous system. This explains the effectiveness of antiepileptic drugs and antidepressants for such a variety of conditions, as well as the ineffectiveness or low effectiveness of H1 blockers for some types of itch.
Mechanisms and mediators involved in the formation of the sensation of itching:
- amines (histamine, serotonin, acetylcholine);
- proteases and kinins (tryptase, chymase, kallikrein, bradykini, etc.);
- neuropeptides (substance P, neurotensin, etc.);
- cytokines (prostaglandin E reduces the threshold for susceptibility to itching);
- opioid receptors (metenkephalin, leuenkephalin, β-endorphin), naloxone reduces itching, opiates relieve pain but increase itching.
Classification
By prevalence
Localized:
- non-specific:
dry skin, parasitic diseases, skin diseases (eczema, bullous pemphigoid, etc.), fungal skin lesions, allergic skin manifestations, insect bites, contact dermatitis;
- specific for oncological diseases:
melanomatosis (for cancer of the anus and vulva), glioblastoma, metastatic skin lesions, paraneoplastic syndrome.
Generalized:
- non-specific:
primary skin diseases, endocrine diseases (hypothyroidism, thyrotoxicosis, diabetes mellitus), carcinoid syndrome, diseases accompanied by cholestasis, blood diseases (for example, Vaquez disease), neurological diseases, senile pruritus, psychogenic pruritus, pruritus caused by infectious diseases, iatrogenic pruritus ( side effects of drugs);
- specific for oncological diseases:
chronic lymphocytic leukemia, Hodgkin's disease, lymphomas, mycosis fungoides (a type of T-cell lymphoma), multiple myeloma, paraneoplastic syndrome.
By genesis
Central:
• neuropathic: brain abscess, brain injury, brain tumor, multiple sclerosis;
• neurogenic: cholestasis, opioids, paraneoplastic process;
• psychogenic: psychosomatic disorder manifested by itching.
Peripheral:
• cutaneous, “pruritoceptive”: cutaneous mastocytosis, medications (± rash), infestations (scabies, lice, fleas, mites), primary skin diseases, plant burns, urticaria;
• neuropathic: postherpetic neuralgia.
Mixed: central and peripheral – uremia.
Diagnostics
Anamnesis
- Localization : focal or generalized.
- Onset : acute onset is the least characteristic of systemic diseases.
- Duration.
- Nature/character : severe, constant itching, worsening in the evening - scabies;
- “burning” itching – perpetiform dermatitis;
- “tingling” – polycythemia.
Physical examination
- Careful examination of the skin: primary lesions;
- excoriation of the skin in various areas (pediculosis, scabies);
- inflammatory papules on the legs with a small vesicle in the center (flea bites);
- “butterfly” sign in the upper central part of the back (hepatobiliary pathology);
- uremic chills.
Laboratory research
Complete blood count with leukoformula, urea, creatinine, liver tests (markers of cholestasis - alkaline phosphatase, gamma-glutamyl transpeptidase (GGT), determination of bilirubin), thyroxine (T-4) and thyroid-stimulating hormone (TSH), blood glucose.
How to stop itching
The difficulty is to break the vicious circle of itching/scratching, and this is not at all as easy as it seems.
Cold showers, baths, and ice packs can help numb the itching.
Moisturizing should be the first step to getting rid of eczema, as moisture can help block the spaces between skin cells where allergens multiply. You can also use one of the over-the-counter medications to treat your symptoms.
If the itching continues to haunt you, it is recommended to consult a doctor.
Patient management
General events
- If your skin is dry, use soap substitutes with a moisturizing effect instead of soap, and apply moisturizing cream to your skin 2-3 times a day.
- Review the list of medications you are taking: if a possible cause of itching is a medication, it needs to be changed.
- For atopic/contact dermatitis: topical corticosteroids once a day for 2-3 days if there is inflammation but no infection.
- For scabies: topical permethrin or malathion.
- For cholestatic itching due to obstruction of the common bile duct: duct stenting – if possible.
Nonspecific treatment
It is carried out taking into account the condition of the skin - different approaches to local treatment on intact and macerated skin.
Antipruritic agents for topical use : 0.5−2% cream with levomenthol (menthol) is effective on intact skin if the itching is localized or more intense in a certain area.
Sedating antihistamines can be prescribed 1 hour before bedtime; if the effect does not persist for a day, two-time use is possible:
- Hydroxyzine/Atarax, Vistaril 25 mg orally at night;
- promethazine/Pipolfen 25 mg orally at night;
- diphenhydramine/Diphenhydramine 50 mg orally 1–2 times a day;
- Dimetindene/Fenistil 1 mg orally daily plus Fenistil gel (0.1% dimethindene) topically 3 times a day will help in most difficult cases.
Some non-sedating antihistamines may have an antipruritic effect (eg, loratadine/Claritin, cetirizine/Zodac, Zyrtec).
Antihistamines for external use (for example, Fenistil cream) on intact skin are used for no longer than a few days in cases where itching is caused by the release of histamine (for example, acute drug rash).
TCAs with antihistamine properties : doxepin/Doxepin in a dose of 10-75 mg orally at night. Antidepressants will help in cases where anxiety or depression occurs.
Specific treatment
Table 1 and Appendix 1 present the principles and regimens of drug therapy for itching of various etiologies.
How to prevent itching
Hygiene of the skin of the feet is the main ally in the fight against itching, along with proper skin hydration.
Also try to wear socks made from natural materials and use breathable shoes. Foot fungus occurs when your skin is too wet, so try to always dry your feet after showering and don't let your feet sweat too much.
In addition, you do not have to worry too much about the fungus, because there are many drugs that can help you get rid of it at home. They will help you get rid of infection and itching.
The main thing is to remember that you need to put on socks and shoes only after your feet are completely dry.
Useful tips
Systemic treatment is often not necessary if the skin condition improves.
If your skin becomes dry, stop using soap; bathing in warm rather than hot water, lubricating the skin after bathing and at night, applying a damp cloth for 15–20 minutes, then applying cream or ointment.
For damp skin - protective cream (zinc paste), drying dressings with Burov's liquid (aluminum acetate 8%, diluted 1:10–1:20).
Local anti-itch remedies
Zinc oxide has anti-inflammatory, antiseptic and antipruritic effects, and is used in concentrations of 10–50% in creams, liniments, lotions, ointments and pastes that are effective in the treatment of localized forms of itching.
Menthol, when applied to the skin and mucous membranes, dilates blood vessels, causing a feeling of coldness and then numbness, significantly reducing itching. It is used in powders, ointments, and lotions in concentrations of 1–10%.
Camphor , when applied to the skin, produces a warm sensation followed by mild anesthesia, which reduces itching. It is used in the form of liniments, lotions and ointments in concentrations of 2–20%.
Important
It should be remembered that products with menthol and camphor cannot be used simultaneously on one area of the skin.
Calamine , a lotion containing zinc carbonate (calamine), zinc oxide and a small amount of phenol, is widely used in the treatment of itching and atopic dermatitis.
Problem
Itchy skin can appear on any part of the body, but most often we experience it on the skin of the arms and legs.
It can begin at any time of the day, but it is especially unpleasant to experience itching at night, when it is most difficult for us to resist the urge to scratch the itchy area.
In addition, when we rest, the body produces less adrenaline and cortisone, but there is an increase in the production of the hormone histamine, which makes us feel itching even more. It can become a symptom of the development of an infection, in particular, foot fungus .
Care Tips
- Prevention of scratching: short-filed nails, lightly rubbing itchy areas.
- After washing, dry your skin carefully using wet movements, use a soft towel or a hair dryer on a cold setting.
- Avoid long hot baths. Try a bath with sodium bicarbonate (baking soda) or medicated oils.
- Use loose clothing and loose bedding/blankets.
- Avoid overheating and sweating, especially during night sleep.
- Increase the humidity in the bedroom so that your skin loses less moisture.
- Wear cotton gloves at night to prevent scratching.
- Avoid damaging the skin with alcohol-containing rubbing, woolen clothing, and excessive hygiene procedures.
- Cleanse your skin gently using moisturizers.
- Use cooling, soft compresses.
- You can use an anesthetic mixture: aftershave cream with menthol 50 ml, Diphenhydramine 1% 3–5 ml, Lidocaine 2% 1–2 ml, Novocaine 0.5% 5–10 ml. Mix and serve chilled.
- Use relaxation and positive visualization techniques.
Physiological reasons
In a healthy person, edema may appear in the evenings after heavy physical exertion or prolonged standing as a result of increased hydrostatic pressure in the blood vessels. The likelihood of swelling increases in the heat, when staying in a stuffy room or at high altitude, when drinking a large volume of liquid, excessively enjoying salty foods, and abusing alcoholic beverages (salt and alcohol retain water).
Swelling of the feet is especially common in women when wearing high-heeled or high-platform shoes. Due to the unnatural position of the foot, blood circulation in the lower extremities is significantly impaired, which leads to stagnation and accumulation of fluid. Similar processes are observed if you wear too narrow shoes and shoes with flat soles.
For physiological reasons, the swelling is mild and symmetrically covers the ankles and feet (occasionally the lower legs). When pressed with a finger, they leave an instantly disappearing mark. After rest they disappear completely.
If the legs swell for physiological reasons in women and men, then there is no need for special treatment. It is enough to adjust your lifestyle.
Hormonal fluctuations in women
In women, before the onset of menstruation, the concentration of progesterone in the blood decreases, which can cause fluid retention, causing pasty (swelling) ankles. Swelling is most pronounced during premenstrual syndrome.
During menopause, hormonal levels are constantly changing, so women may periodically swell their lower extremities. This problem can also be the result of hormone replacement therapy.
During reproductive age, swelling of the legs may occur when taking oral contraceptives.