A septum in the uterus is a malformation of this organ, which is quite rare in medical practice. The pathology is characterized by the formation of septa of varying lengths, which divide the uterus into two parts.
Often women with a similar diagnosis have a prognosis of miscarriage and, less often, infertility. Indeed, with an intrauterine septum, the risks of premature miscarriage increase significantly, as well as the risks of premature birth in the second trimester of pregnancy.
However, if you have been diagnosed with an intrauterine septum, you should not despair. Our clinic offers modern ways to eliminate this pathology. If you have difficulty conceiving with this diagnosis, our specialists will help you plan your pregnancy wisely and carry your child to term. All you need to do is strictly follow the doctors’ recommendations.
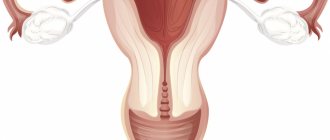
Saddle-shaped uterus: what does it mean, schematic image
To understand what we are talking about, we suggest you look at the picture below. It shows a normal-shaped uterus, saddle-shaped (arcuate) and bicornuate. The arcuate uterus differs from the usual one only in the depression in the form of a saddle in its bottom (the uppermost part). The developmental defect is minor. But it can become a source of problems if the “saddle” is pronounced, that is, deep. But this is rare.
More often, problems arise with a bicornuate uterus. Gynecologists have three definitions that they use: saddle uterus, bicornuate with a cavity partially divided into “horns” (in the bottom) and completely divided.
Back to contents
Symptoms
Often, especially with incomplete duplication and saddle uterus, there may be no serious symptoms.
The main pathological conditions are as follows:
- Menstrual irregularities are rare.
- Miscarriage is most often associated with impaired formation of the placenta and, as a consequence, malnutrition of the fetus.
- Infertility is a rare condition, since the duplication of the uterus itself cannot cause infertility. Pregnancy occurs even with complete doubling, and in this case it develops most often in one of the horns of the uterus (less often in both horns). As a rule, the cause of infertility is a combination with other developmental defects.
Causes of a “saddle” in the fundus of the uterus
This malformation of the female reproductive system is congenital, not acquired. At 10-14 weeks of pregnancy, in utero, that is, the formation of the uterus begins. At first, for everyone it consists of two cavities, completely separated by a septum, that is. Toward the end of pregnancy, only one cavity remains, but the uterus retains a slight deformation in the fundus (upper part). Many girls are born with an arcuate uterus. But there are also those whose uterus remains bicornuate from the prenatal period. Saddleback is the mildest developmental anomaly.
Back to contents
Surgery
Many women with uterine abnormalities do not require treatment. If the problem is pain, miscarriages, or infertility, your doctor may recommend surgical correction of the abnormality. In most cases, uterine abnormalities can be treated using minimally invasive methods, such as laparoscopy or hysteroscopy.
In the case of a unicornuate uterus, the blocked half of the uterus can be removed if the other side is intact and functioning properly. The septum may also be removed to expose the uterine cavity.
Signs of a saddle uterus on ultrasound and other diagnostic methods
There are several ways to diagnose or define this pathology.
- Hysterosalpingography (HSG, metrosalpingography, hysterography) - x-ray of the internal genital organs. A contrast agent is injected into the uterus through a narrow catheter. After which a photo is taken. The disadvantage of this type of study is that it is invasive, there are unpleasant sensations, plus small ionizing radiation.
- Magnetic resonance imaging (MRI) . Very informative, but there is a minus - it's expensive.
- Ultrasound . Pros: cheap, not painful, does not require anesthesia and has no contraindications. But not every specialist will be able to determine the irregular shape of the uterus by ultrasound. Apparently, for this reason, the detection rate of the arcuate uterus in comparison with the bicornuate uterus is so low. The specialist carefully examines the area of the uterine fundus, M-echo in this area, whether there is any bulging of the myometrium, measures the length and width of the uterus, with such malformations they are larger than average.
Back to contents
Is it possible to sunbathe after removal of uterine fibroids?
We often hear from patients that their doctor forbade them to sunbathe because he has fibroids. This is one of the deepest misconceptions among doctors, coming from the medical views that existed 20 years ago. It is reliably known that ultraviolet rays do not affect the growth of fibroid cells. This is a hormonally dependent tumor. She has many receptors for female sex hormones, which is why changes in hormonal levels are the main factor in her growth. Therefore, there is no point in restricting women with fibroids and prohibiting them from basking in the sun. After all, the sun synthesizes vitamin D in the body, the main element to strengthen the immune system.
Is treatment for uterine defects necessary and why is it dangerous?
A bicornuate uterus is characterized by heavy, painful and prolonged periods. With the saddle shape, menstruation is normal, normal, if there is no concomitant gynecological pathology.
The woman does not notice any peculiarities. The intrauterine device is not contraindicated for her. There is no increased risk of uterine perforation during or after IUD insertion. Surgical abortions are performed. Although it is better to avoid them for any shape of the uterus, of course.
As for infertility, a slight decrease in fertility is possible. But we will talk about this a little below.
No abnormalities in the structure of the uterus are treated with drugs, only surgically. An operation called metroplasty . It can be done using hysteroscopic access, that is, the doctor inserts instruments directly through the vagina and cervix and creates a single cavity in the uterus. To ensure everything goes perfectly, laparoscopic (endoscopic) equipment is used as control, which is inserted through a tiny puncture in the abdominal wall. But, we repeat, the operation is performed only if necessary - if there is infertility due to the shape of the uterus, there have been miscarriages, or a history of premature birth. Many women successfully bear and give birth to children with a bicornuate uterus, not to mention a saddle uterus.
We bring to your attention a video with Elena Malysheva (TV show “Live Healthy”) about a bicornuate uterus. Including surgical treatment. Watch from 33 minutes.
Back to contents
Features of therapy at the S. A. Kapranov Center
Currently, Professor S. A. Kapranov and specialists from the Center for Endovascular Surgery have experience in the use of endovascular arterial embolization, unique for Russia. This allows them to treat not only the underlying disease, but also to combine treatment methods for focal, nodular, and diffuse forms with uterine fibroids and endometrial pathology.
Before endovascular intervention (EMA), most of our patients, due to the presence of severe uterine bleeding, had to undergo multiple unpleasant procedures for curettage of the uterine mucosa; many of them were prescribed ineffective hormonal therapy. As a result, women had to take strong hormonal drugs for a long time - from several months to 2 years. All this gave a minor effect: in rare cases – up to 6 months. In some cases, adenomyosis was not eliminated. The therapy had no effect at all.
Professor S. A. Kapranov and his colleagues have developed and are actively implementing special methods of endovascular treatment - staged and partial embolization of vessels, and carefully select the size of emboli, taking into account the individual characteristics of the structure of the patient’s blood vessels. Among other things, the use of only ultra-modern embolization drugs makes it possible to achieve colossal positive results in the treatment of women.
Is it possible to completely eliminate adenomyosis?
Yes!
This has been clinically proven. For a disease that proceeded without complications or concomitant diseases, a month after UAE, about 50% of patients noted a complete disappearance of symptoms.
Already 3 months after the intervention, the menstrual cycle is completely stabilized in 100% of patients.
5 months after surgery, there is a reduction in blood loss during menstruation. This allows you to increase the level of hemoglobin in the blood. The duration of menstruation stabilizes by 37%.
If adenomyosis was combined with fibroids, the clinical effectiveness of the technique is 97%. 5-6 months after the operation, pain disappeared in 78% of women, and menstrual function gradually stabilized. Moreover, it remains unchanged throughout the year and longer periods.
The following services are offered at the Professor Kapranov Center.
Targeted staged and partial embolization, taking into account the individual characteristics of the body and the degree of the disease.
Selection of drugs used depending on the size and shape of the vessels. Specialists use only the most modern means. These include: Contour (Boston Scientific), BeadBlock (Terumo, Japan) and Embosphere (Merit Medical, USA).
The main advantages of therapy at the center of Professor Kapranov include:
- Attentive attitude towards each patient. Before any therapy, a thorough examination is carried out. It allows you to find out all the characteristics of a woman’s body, possible reactions to the drugs used, and prevent the risks of any complications.
- Comfortable conditions for all procedures. Specialists always use modern painkillers. This eliminates any discomfort.
- Optimal cost of services.
How to get pregnant: positions for conception, reviews
If the saddle of the uterus is pronounced, this may slightly reduce the chances of rapid conception. In what position is it recommended to have sex to get pregnant faster? The position in which sexual intercourse will take place is not very important. But you need to try to ensure that the maximum number of sperm gets into the uterus, which means that immediately after sex you need to lie down, slightly raising your pelvis, placing a pillow under it. And this is more than enough.
Try to have a regular sex life. And this means - have sex 2-3 times a week . If you want to further increase your chances of conceiving, learn how to detect ovulation. This can be done through tests and observing how you feel. Typically, in the first half of the cycle, women have virtually no vaginal discharge. From about the eighth day of the cycle there is a small amount of thick white or yellowish. And 1-2 days before ovulation, a viscous transparent discharge similar to egg white appears. They are clearly visible if you squat and when urinating.
Directly on the day of ovulation, stabbing pain is usually felt from the ovary, in which the follicle ruptures. The stomach may ache quite severely. Some women mistake this as a sign that their period is about to begin. But there is still quite a long way to go. 14 days. After a few hours the pain goes away. After another couple of weeks, all the discharge disappears...
If you are “trying” to conceive a child during ovulation, while your partner is fertile, and pregnancy does not occur for more than 1-2 years, you need to look for the reason for this. Perhaps there is an endometrial polyp and it needs to be removed, there is a submucous myoma - a neoplasm that deforms the uterine cavity, synechiae or a septum in the uterus, chronic endometritis - there can be a lot of reasons. You should not attribute your failures to the saddle of the uterus.
Back to contents
Uterine artery embolization
This technique allows you to save the uterus. This is what is very important for any woman. In this case, adenomyosis does not bother the patient. She does not suffer from constant bleeding, pain, or weakness. The risk of anemia is significantly reduced.
What is the essence of treatment?
Let us remember that adenomyosis is a disease in which the endometrium begins to grow where it should not be. During embolization, the nutrition of those branches that feed the pathological formations is stopped. In this case, healthy parts of the endometrium are not affected. This is achieved by introducing special embolization particles into the vessels.
To embolize the uterine arteries, a puncture is necessary. It is carried out in the upper thigh. The puncture is carried out under local anesthesia and does not cause pain.
After this, a catheter is inserted into the vessel. It is carried out in the uterine artery. Advancement of the catheter through the vessels also does not cause discomfort. After installing the catheter, special embolization particles are injected through it. They have a size of 0.5 mm, do not cause discomfort, and do not in any way affect the patient’s health. Usually the procedure lasts 1-1.5 hours.
Within 7-8 hours after the procedure, the patient experiences pain in the abdominal area. This is due to blockage of the arteries of the uterus. Special painkillers are usually prescribed. They allow you to completely eliminate discomfort.
The main advantages of uterine artery embolization:
- Impact on all pathological foci. Adenomyosis is completely eliminated.
- Possibility of organ preservation. Adenomyosis often leads to the need to remove the uterus. Embolization eliminates such risks.
- Low trauma and no blood loss. The only puncture is a puncture. The bleeding stops quickly. This reduces the risk of anemia.
- No cosmetic defects. The puncture mark disappears within a few months. Even if it persists, it is only in the form of a tiny scar. It is almost impossible to notice it with the naked eye. No incisions are made in the peritoneal area. Thanks to this, there are no large scars left on the patient’s abdomen.
- Low percentage of relapses in the long term.
- No general anesthesia. This allows you to reduce the negative impact on the patient’s body.
- Reducing menstrual bleeding, dysfunction of the bladder and other organs.
Can adenomyosis develop into a malignant tumor?
Such cases are recorded extremely rarely. With a pronounced reaction of the body to the introduction of estrogens into endometrial tissue, changes may occur that contribute to malignancy. But rebirth occurs only in isolated cases.
Important! This does not mean that you do not need to engage in treatment! Any woman should always monitor her health. If there are any signs of illness, you should consult a doctor. It should be understood that bleeding is dangerous, pain significantly reduces the quality of life.
Features of pregnancy and childbirth with an arcuate uterus
Pregnancy, including through IVF (in vitro fertilization) and natural childbirth are not contraindicated. Caesarean section (CS) is performed only if there are other indications for this operation. For example, the incorrect position of the child in the uterus, if the fetus is located across it at the time of birth. Buttock and pelvic presentation are indications for CS only if the fetus is male or female, but large, presumably more than 4 kg, or the woman has already had a cesarean section in the past, that is, there is a scar on the uterus. Premature birth of twins at a very early stage, for example, at 26 weeks of pregnancy, is in many cases also a reason to undergo surgery.
There is an opinion that the arcuate uterus provokes miscarriage or frozen pregnancy, poses a threat to early pregnancy, and provokes tone. This is wrong. A similar situation is only possible with a bicornuate uterus, if the fetus develops in a small horn.
Back to contents
What complications does the disease cause?
The main danger is that internal endometriosis can spread to other tissues and organs. If the ovaries and fallopian tubes are negatively affected, infertility occurs. When tissue grows into the bladder or rectum, the activity of the gastrointestinal tract and urinary tract is disrupted. This leads to severe pain not only in the uterus, but also in all pelvic organs. It is also dangerous that the tissue can grow into the nerve plexuses of the lumbosacral region. In this case, the patient experiences extremely severe pain. During treatment, discomfort can be relieved, but only if it is carried out correctly.